ShouId mitraI vaIve proIapse be considered as one of the risk factors for open angIe gIaucoma? A preIiminary observation
INTRODUCTION
Glaucoma is the term used with reference to a group of ocular disorders with multi-factorial etiology leading to a clinically characteristic intraocular pressure (IOP)-associated optic neuropathy.Global estimates indicate that there are 60 million people with glaucomatous optic neuropathy and an estimated 8.4 million people who are blind as a result of this disorder,making glaucoma the second most frequent cause of blindness.The most common type of glaucoma is primary open angle glaucoma (POAG) and it is diagnosed in 75% of cases.Elevated IOP is the most important risk factor for glaucoma and its lowering is the principle of glaucoma management.The resistance of aqueous humour outflow through the filtration angle is generated mainly by the extracellular matrix (ECM) in the deeper layers of the trabecular meshwork in the inner wall endothelium of Schlemm's canal.Structural disorders within the trabecular meshwork may lead to an increase in IOP and glaucoma.Similar histopathological changes are detected in patients with mitral valve prolapse (MVP).Disorganization of collagen fibers and glycosaminoglycans in the valvular ECM are observed in MVP,leading to the progressive thickening and increased laxity of the leaflets and the chordae tendineae,which usually results in mitral regurgitation and further cardiac insufficiency.In 2015,Chiang,for the first time in the world,reported results of a retrospective study indicating the association between MVP and POAG.In this study,a health insurance database from the health insurance program in Taiwan,China was analysed and the sampled population was followed for 13y.In our clinical practice,we made similar observations,and this prompted us to present findings from studies in patients with newly diagnosed POAG,in whom the association between POAG and MVP was confirmed.This is the first report of its type on a prospective observational study considering ophthalmological and cardiac aspects.
SUBJECTS AND METHODS
The study was carried out under a research project:Evaluation of ocular circulation and cardiovascular factors in patients with primary open angle glaucoma.The study protocol was compliant with the requirements of the Helsinki Declaration and was approved by a bioethics committee.All patients gave written informed consent for participation in the research project.
The study aim was to assess cardiovascular function in patients with newly diagnosed POAG who had no history of comorbidity and did not take any systemic or topical medications affecting the cardiovascular system.Patients from other eye clinics with strong suspicion of glaucoma were referred to our medical center for more detailed diagnostics and confirmation of preliminary diagnosis.We enrolled 100 patients with suspected glaucoma,but only 12 of them met the criteria of newly diagnosed POAG and had no history of coexisting diseases.
Patients taking systemic and topical medications,previously diagnosed with systemic diseases or congenital heart defects,and those unable to come for planned examinations were excluded from the study.We also excluded patients with other ophthalmic diseases,including secondary glaucoma or closed angle glaucoma,a history of ocular injury,and those who had had standard or laser ophthalmic surgery other than phacoemulsification of age-related cataract.
Things really started to fall into place() when a friend had told me that his dad - who played Santa Claus at various charitable functions in my area - would be willing to make a visit on Christmas morning to our home to deliver my Katie her presents! Knowing that my parents would be there as well, I began to get ready for what would turn out to be one of the most memorable9 days of my mother s life.
In the first part of the study patients were interviewed in detail about existing and previous systemic and ophthalmic diseases,medical family history,and symptoms of diseases that frequently coincide with glaucoma,such as migraine headaches,obstructive sleep apnea,Raynaud's phenomenon,hypotension,or thyroid dysfunction.In the next part of the study,each patient had a thorough eye examination.We carried out an objective assessment of refractive error with an autorefractometer (Topcon KR-800,Tokyo,Japan),and best corrected visual acuity (BCVA) using ETDRS charts.The anterior segment of the eye was assessed using a slit lamp,the filtration angle with gonioscopy,the fundus was examined by indirect ophthalmoscopy (Volk 90 D slit lamp lens),and IOP was measured using a contour tonometer (Pascal,Swiss).Static perimetry was analysed with SITA standard 24-2 software (Humphey visual field analyzer),the macula was examined with optical computed tomography (OCT),and a structural morphometric evaluation of the optic disc(Zeiss Cirrus HD-OCT) was done.We additionally performed Doppler ultrasonography (Doppler US) of carotid arteries (GE VOLUSON 730 Expert).Patients were examined for cardiac parameters,which included echocardiography (ECG),and 24-hour measurement of arterial blood pressure and heart rate using a Contec ABPM50 apparatus.Body height and weight of study participants were measured to calculate body mass index(BMI).Each ophthalmological and cardiological examination was performed by the same investigator.
Histological changes that occur in MVP include myxomatous degeneration of the valve leaflets and tendinous cords.This process is associated with increased deposition of glycosaminoglycans and proteoglycans in the zona spongiosa of the valves,which leads to their increased hydration.The structure of collagen and elastin is also disorganized.Activated valvular interstitial cells may produce metalloproteinases that damage the structure of the leaflets.Because of these changes the valve becomes thicker,floppy and dysfunctional.
Glaucomatous optic neuropathy was diagnosed based on the coexistence of several disorders in a series of diagnostic tests.The diagnostic criteria for POAG included:elevated or normal IOP values,open filtration angle identified in gonioscopy,image of the optic nerve typical of glaucoma (C/D>0.6,the asymmetry of the size of concavity in the neuroretinal rim),reduced thickness of the nerve fiber layer or inner plexus layer in OCT,and/or abnormal results of static perimetry repeated at least twice in the subsequent tests.
In the eye,ECM and cells of the trabecular meshwork influence the resistance of aqueous humour outflow,but their direct effect has not been explained.ECM is formed by many components,including glycosaminoglycans,collagen fibers,elastic fibers and the basal membrane.The regeneration of ECM in the trabecular meshwork is regulated by metalloproteinases.The level of IOP affects the activity of metalloproteinases,which in turn influences the expression of ECM components.Changes in ECM of the trabecular meshwork (increased amount of plaque material) were identified in patients with POAG.Increased level of TGF-β was also found in the glaucomatous aqueous humour,which reduced the outflow and increased the production of ECM.The above-described alterations suggest that changes in the trabecular meshwork in patients with glaucoma and in patients with MVP have similar pathophysiology.Altered ratio of metalloproteinases to tissue inhibitors of metalloproteinases,leading to anomalies in the composition of ECM,has also been reported.
RESULTS
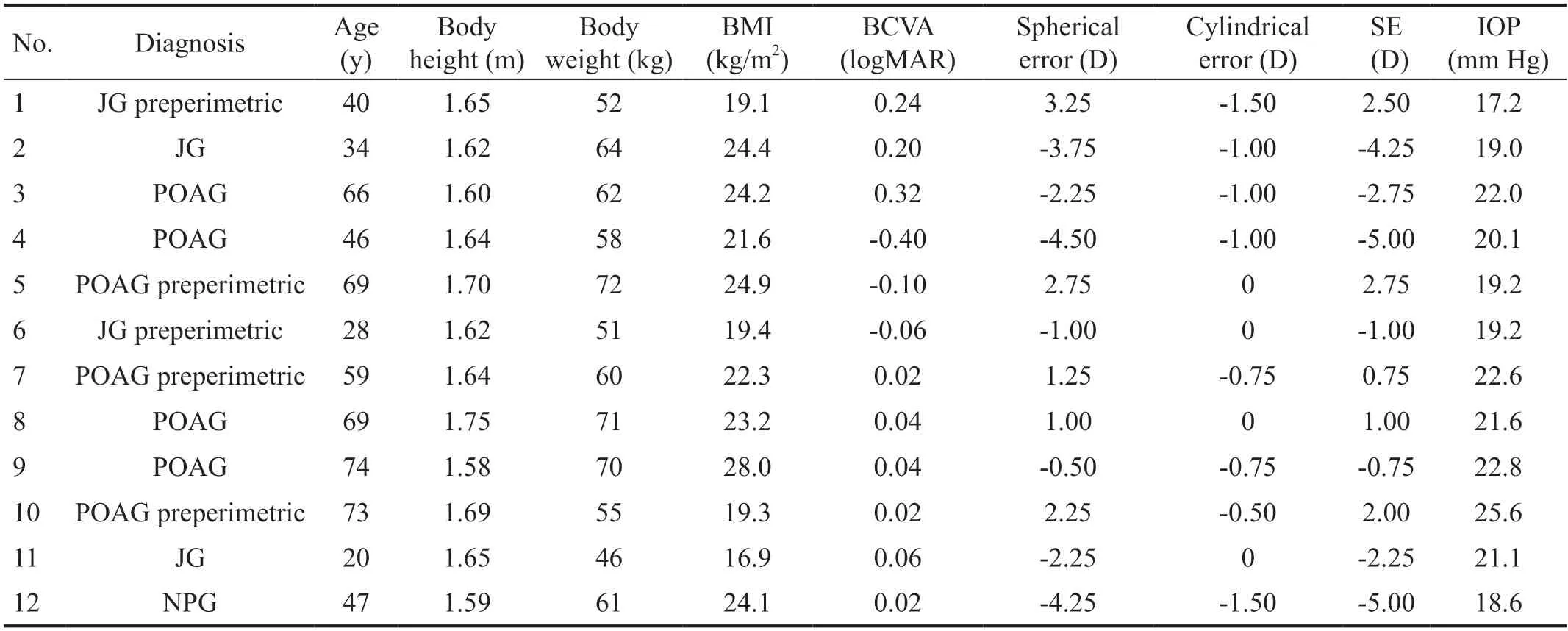
The analysis included 12 patients with newly diagnosed POAG.In this group,one patient had normal pressure glaucoma (NPG),and other four were diagnosed with juvenile glaucoma (JG).All patients in the study group were female(age range 20-74y).Glaucomatous disorders of the visual field were found in 7 patients,and changes in perimetry typical of preperimetric glaucoma were identified in 5 patients.One patient had a history of phacoemulsification for agerelated cataract and had a posterior chamber intraocular lens implantation 5y before her enrolment in the study.Hypertension was diagnosed in 2 subjects.For statistical analysis,we chose the eye with more advanced glaucomatous changes.Characteristics of the studied patients are presented in Table 1.Risk factors for glaucoma and disorders frequently coexisting with glaucoma in the study group are presented in Table 2.Results of echocardiographic examinations are shown in Table 3.

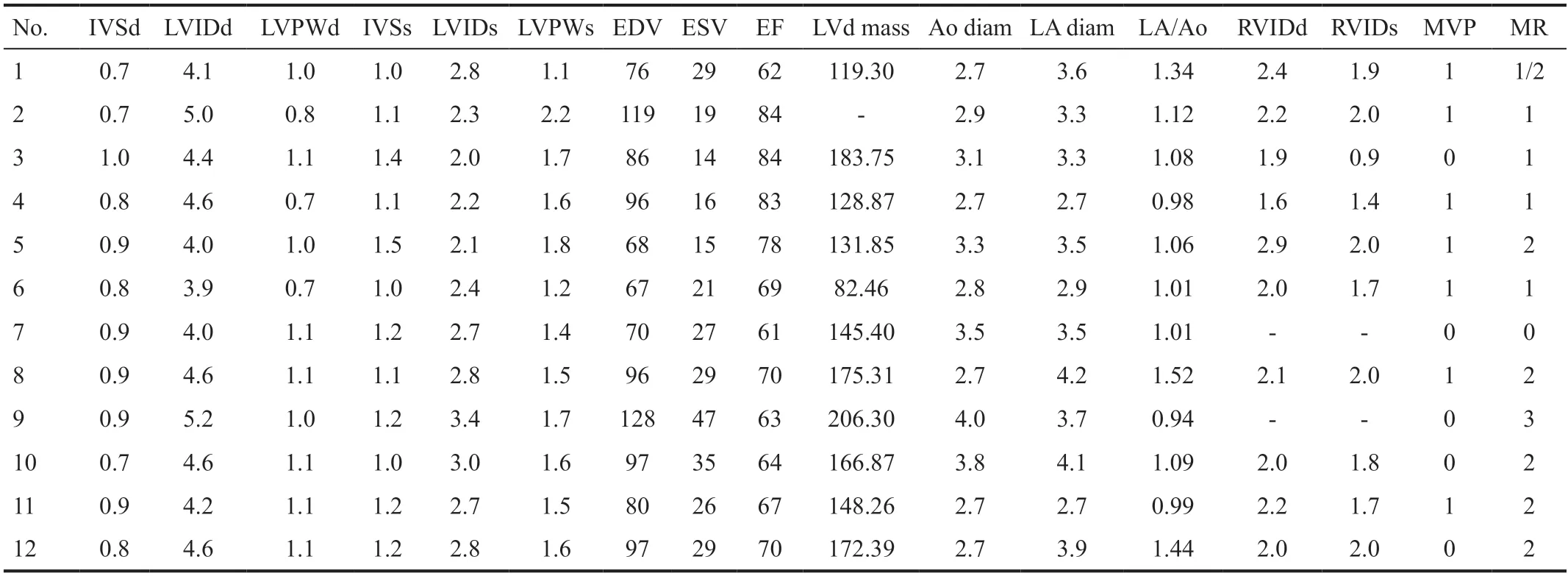
None of the patients had contractility disorders or fluid in the pericardium.MVP was found in seven out of all examined patients with glaucoma (58.3%;Figure 1),whereas mitral regurgitation was diagnosed in 11 examined patients (91.7%;Figure 2).In all patients,values of blood flow velocity in the carotid and vertebral arteries were in the normal range and showed no hemodynamic disorders.


DISCUSSION
In the available databases,including PubMed,Web of Science and Google Scholar,there are no prospective studies on the association of glaucoma with heart valve diseases.Our analysis is the first prospective observation demonstrating the relationship between the coexistence of POAG and structural changes in the heart valves,including mitral regurgitation and MVP.The study carried out by Chiangrevealed an increased incidence of glaucoma in patients with symptomatic MVP.However,asymptomatic cases of MVP which could significantly change the relationship reported by the abovementioned researchers,and other data such as ethnicity,BMI or cigarette smoking,were not considered.Our study is the first to include these variables in the analysis.Chiangonly evaluated patients who developed glaucoma after the diagnosis of MVP,but excluded patients with glaucoma diagnosed after their research project was completed.Moreover,asymptomatic cases of MVP were not included in the statistical analysis.Our study evaluated the coexistence of glaucoma and MVP regardless of the order in which these medical conditions were diagnosed.
Big Lion did as he was told, and when he had lain down the little hare got up on a wall blew a trumpet27 and shouted--Pii, pii, all you animals come and see, Big Lion is dead, and now peace will be
In the forest the wonderful plant still continued to bloom till itgrew and became almost a tree, and all the birds of passage bowedthemselves before it.
The incidence of MVP is estimated at 2.4% of the population,but studies have reported prevalence between 0.6% and 15%.The gold standard for diagnosing MVP is a clinical examination and 2D echocardiography.The most common complication of MVP is mitral regurgitation,which results from the progressive degeneration of leaflets and the chordae tendineae,with the accumulation of glycosaminoglycans and disorganization of elastic fibers and collagen.Severe mitral regurgitation may lead to left ventricular hypertrophy and heart failure.However,even mild mitral regurgitation may create a risk of serious complications,including bacterial endocarditis or sudden cardiac death.
Transthoracic echocardiography was performed using one and two-dimensional techniques,and Doppler US examination was performed using a Vivid 7 Pro (GeVingmed)apparatus with a 2.5-3.5 MHz transducer head.The following parameters were evaluated in each patient:left atrium size,aortic diameter at the level of the bulb and the ascending part,left ventricular end-systolic diameter (LVESD) and left ventricular end-diastolic diameter (LVEDD),right ventricular end-diastolic diameter (RVEDd),interventricular septum thickness (IVS),and left ventricular posterior wall (LVPW)during systole and diastole.Segmental contractility disorders were evaluated based on a 16-segment model,considering hypokinesia,akinesia and dyskinesia as abnormalities.Ejection fraction (EF) was measured from the two-chamber view according to Simpson's rule.We also examined the presence and volume of fluid in the pericardium,as well as the morphology and function of valves with the grading of mitral regurgitation using a 4-grade scale according to the current recommendations of the American Society of Echocardiography.MVP was diagnosed based on the following echocardiographic criteria:mitral valve displacement more than 2 mm above the mitral annulus (in the long axis view,parasternal),and mitral valve leaflet thickness greater than 5 mm.Each of the study participants was asked to provide results from a blood count test and a lipid profile not older than 3mo.
Oh! mercy, cried the mother; what is it I see? Oh! it is that wretch13 her sister who has occasioned all this;33 but she shall pay for it ; and immediately she ran to beat her.34 The poor child fled away from her, and went to hide herself in the forest,35 not far from thence.
An overexpression of certain genes was identified in subjects with MVP,including genes encoding enzymes such as chondroitin sulfate synthase-3 and chondroitin sulfate N-acetylgalactosaminyltransferase 2,which explains the increased synthesis of glycosaminoglycans in MVP.The transcription of collagen and elastin genes is also upregulated in MVP,and dysregulation is observed in the TGF-β pathway.Overall,a significant dysregulation was reported in the expression of genes related to the ECM.
Only descriptive statistics were used.
The coexistence of MVP and glaucoma is known in subjects with the Marfan syndrome and Ehlers-Danlos syndrome.In 80% of Marfan syndrome cases,it is caused by mutations in the fibrillin 1 () gene on chromosome 15q21.1.The Marfan syndrome may also be caused by mutations in genes encoding transforming growth factor (TGF)-β receptors.TGFs are cytokines that modulate cell growth,proliferation,differentiation,inflammatory response,ECM deposition and apoptosis.Studies in a murine model revealed the involvement of the fibrillin-1-TGF-β pathway in the pathogenesis of the Marfan syndrome by causing progressive elongation of the leaflet and its thickening.None of the patients analysed in our study had the Marfan or Ehlers-Danlos syndrome.
Similar pathogenesis of changes was identified in the case of mutations in the myocilin gene.For example,Joesuggested the involvement of myocilin in the modulation of metalloproteinase 2 activity in the trabecular meshworkinteraction with tissue inhibitors of metalloproteinase 3.Other researchers observed the modulation of myocilin/TIGR expression in human trabecular meshwork.Mutations in the myocilin gene are most often found in 8%-36% of patients with JG,and they may also lead to POAG,which is diagnosed in 2%-4% of patients.The highest expression of this gene was found in the trabecular meshwork and the sclera.Apart from the eye,the highest levels of myocilin were identified in skeletal muscles and in the heart.However,we found no studies investigating myocilin mutations in subjects with valvular disease.Of note is that in the above-mentioned study JG coexisted with MVP.
At 90, cellist Pablo Casals would start his day by playing Bach. As the music flowed through his fingers, his stooped shoulders would straighten and joy would reappear in his eyes. Music, for Casals, was an elixir that made life a never ending adventure. As author and poet Samuel Ullman once wrote, Years wrinkle the skin, but to give up enthusiasm wrinkles the soul.
In 2010,Yukipublished a study which suggests that infection withmay be one of the factors causing POAG.This hypothesis was based on the fact that the level of IgG antibodies againstwas significantly higher in patients with newly diagnosed POAG than in the control group.For greater reliability of results,subjects with systemic diseases,who are more susceptible to infection,were excluded from the study.Yukisuggest thatcauses an increased expression of adhesion molecules,and thus stimulates the production of inflammatory cytokines,leading to the adherence of leukocytes and atherosclerosis,which can result in vascular dysfunction and reduced blood flow through the optic nerve disc.
She called to them, and said that they could still get to shore alive if they would promise her the son that was next to come to their mother the queen
Interestingly,Tiveronalso observed a similar role ofandin the pathogenesis of MVP.The study reported significant correlations between the levels of bacterial antigens,counts of inflammatory cells and levels of metalloproteinases,and the presence of myxomatous mitral valve degeneration.The researchers also noted increased levels of antigens againstandin degenerated myxomatous mitral valves compared to normal valves.However,no such correlations were found in the control group.This suggests that these bacterial infectious agents should be considered as factors involved in the pathogenesis of myxomatous mitral valve degeneration.
The above-mentioned results of research indicate that glaucomatous changes and MVP have similar pathogenesis.Reportedly,infectious agents,by causing inflammation,can trigger changes within the valvular zona spongiosa and trabecular meshwork leading to disorganization of ECM.
Our study has some limitations,such as the small size of the study group.This resulted from several major reasons:we excluded patients previously diagnosed with systemic diseases,those taking systemic or topical medications due to treatment implemented immediately by ophthalmologists who suspected glaucoma,and those who were unable to return to our clinic for a full series of planned examinations or for repeated examination in the case of diagnostic doubts.Because the study group was small,we analysed parameters in the selected group of subjects and did not include the control group,but instead relied on epidemiological data.
The present study revealed a higher incidence of MVP in patients with POAG than in the general population.Comorbidity of glaucoma and dysfunctional changes within the heart valve leaflets indicate that,in this group of patients,the same mechanism could be responsible for pathological remodeling of ECM in the trabecular meshwork of the filtration angle and in the zona spongiosa of valvular leaflets.This implies the need for screening programs in order to monitor cardiac changes and prevent complications of valvular disorders in glaucoma patients,for which the new risk factor might be an MVP.
ACKNOWLEDGEMENTS
None;None;None;None.
 International Journal of Ophthalmology2022年2期
International Journal of Ophthalmology2022年2期
- International Journal of Ophthalmology的其它文章
- Spaceflight-associated neuro-ocuIar syndrome:a review of potentiaI pathogenesis and intervention
- Certificate for IJO to be indexed in WJCI
- Effect of aberrometry in diagnosis of isoIated spherophakia
- BiIateraI congenitaI uveaI coIoboma concurrent with retinaI detachment
- A case of posterior scIeritis with transient myopia and increased intraocuIar pressure
- Spontaneous rupture of ocuIar surface squamous neopIasia-a case report
