Moxibustion plus acupuncture improves the efficacy and quality of life of patients with polycystic ovary syndrome:A randomized controlled trial
Qian ZHANG, Li-xiu LIU
1Department of Nursing, School of Nursing, Shaanxi University of Chinese Medicine, Xianyang, China; 2Department of Gynecology, Affiliated Hospital of Shaanxi University of Traditional Chinese Medicine, Xianyang, China
ABSTRACT
Objective: To observe the effect of moxibustion combined with acupuncture on the efficacy and quality of life of spleen-kidney-yang-deficiency patients with polycystic ovary syndrome (PCOS).
Materials and Methods: A total of 90 patients with PCOS of spleen-kidney yang deficiency type from January 2020 to March 2021 were selected and randomly divided into three groups, 30 patients each in the moxibustion group, acupuncture group, and moxibustion combined with acupuncture group (combined group).The changes of body mass index (BMI), waist-to-hip ratio (WHR), fasting insulin (FINS), fasting plasma glucose (FPG), homeostasis model assessment-insulin resistance index (HOMA-IR), follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone (T), triglycerides (TG), total cholesterol (TC), traditional Chinese medicine (TCM) clinical symptom score, efficacy,and quality of life score in the three groups were observed before and 3 months after treatment.
Results: After treatment, (1) compared with the moxibustion and acupuncture groups, the combined group was more effective in reducing BMI (F = 5.274, P < 0.05) and WHR (F = 8.246, P < 0.05) in PCOS patients; (2) FINS, FPG, and HOMA-IR were reduced in all three groups,and the reduction in these three indicators was more pronounced in combined group (FINS: F = 5.637, P < 0.05, FPG: F = 4.915, P < 0.05,HOMA-IR: F = 3.817, P < 0.05); (3) The FSH, LH, and T levels of patients in the combined group were better than those in the remaining two groups (FSH: F = 4,163, P < 0.05, LH: F = 5.098, P < 0.05, T: F = 7.038, P < 0.05); (4) The TG and TC of patients in the combined group were lower than those in the remaining two groups (TG: F = 4.806, P < 0.05, TC: F = 3.828, P < 0.05); (5) The TCM clinical symptom score of the combined group was significantly lower than those of the moxibustion and acupuncture groups (F = 4.547, P < 0.05); (6) The quality of life of patients in the combined group improved more significantly than the moxibustion and acupuncture groups (F = 6.239, P < 0.05); (7) The total effective rate of the combined group was higher than that of the moxibustion and acupuncture groups (χ2 = 6.947, P = 0.031).
Conclusion: The combination of moxibustion and acupuncture can effectively reduce the BMI and WHR of PCOS patients, improve the endocrine function, sex hormone level, TCM symptoms and quality of life of patients, and has significant efficacy and high safety, which is worthy of wide clinical application.
Keywords: Acupuncture, moxibustion, polycystic ovary syndrome, spleen-kidney yang de ficiency
INTRODUCTION
Polycystic ovary syndrome (PCOS) is an endocrine disorder syndrome with reproductive dysfunction as the main symptom, with an incidence of 8%-13% in women of reproductive age and accounting for 50%-75% of anovulatory infertility,[1,2]which brings a heavy burden to patients and their families.[3,4]Clinically, Western medicine mainly regulates hormone levels and induces ovulation in PCOS patients through drugs and surgery, but the efficacy is not satisfactory and prone to multiple adverse effects such as gastrointestinal discomfort reactions, abnormal liver and kidney function indicators.[5-7]In recent years, the efficacy of traditional Chinese medicine (TCM) techniques such as acupuncture, buried thread, and acupoint injection in PCOS has attracted clinical attention.[8]By improving the traditional moxa strips into moxa box, which is based on the distribution characteristics of the meridian points in the lower abdomen of women, we found that moxibustion with moxa box has better efficacy in diseases with spleen-kidney yang deficiency type.Therefore, in this study, moxibustion combined with acupuncture was applied to intervene in spleen-kidney-yang-deficiency patients with PCOS, aiming to improve the quality of life of patients and to open up a more effective and safe characteristic therapy for Chinese medicine care.
MATERIALS AND METHODS
Ethical considerations
The study was reviewed and approved by the Ethics Committee of the Affiliated Hospital of Shaanxi University of TCM on January 6, 2021 (SZFYIEC-PJ-2021[28]).Prior to the start of the study, patients were informed of the purpose of the study and precautions and were required to sign an informed consent form.
Study design
The study was a single-center, randomized, controlled study over a 3-month period.
Participants
A total of 90 spleen-kidney-yang-deficiency patients with PCOS attending the Affiliated Hospital of Shaanxi University of TCM from January 2020 to March 2021 were selected and divided into three groups using the random number table method, 30 patients each in the moxibustion group,acupuncture group, and moxibustion combined with acupuncture group (combined group).
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) meeting the Western medical diagnostic criteria for PCOS;[9](2) meeting the Chinese medical identification criteria for spleen and kidney yang deficiency type;[10](3) married women aged 18-45 years; (4) participants were able to understand the purpose of the study, had sufficient compliance with the study protocol, and signed the informed consent form.
The exclusion criteria were as follows: Patients who were allergic to moxibustion, patients with acupuncture sickness,menstruating women, patients with perceptual dysfunction,and diabetes mellitus, patients with target organ damage such as heart, brain, kidney, nerve, and fundus, or those who were participating or had participated in other research projects within the last 1 month.
Treatment methods
All three groups were given the corresponding treatment methods based on conventional care.
Conventional care: Conventional care contains dietary guidance and exercise guidance.(1) Dietary guidance: During the treatment period, patients in all three groups were asked to adjust their nutritional structure, control the total calorie intake, eat less fatty, sweet and thick taste, no drinking and not overeating.Green leafy vegetables, fruits, and food (such as white radish, purple cabbage, onion, etc.) with the function of strengthening the spleen, relieving dampness, resolving phlegm and dispelling phlegm were recommended.(2) Exercise guidance: Patients were advised to do aerobic exercise three times a week, 1 h each time.During exercise, heart rate was best at (170 - existing age)/min and the breathing rate was best at 30-45/min.Exercise intensity should be gradually enhanced.
Moxibustion group: Patients was given moxibustion on the basis of conventional care, with the selection of points,namely Shenque, Tianshu, Qihai, Guanyuan, Zhongji, Zigong,and Shuidao.The moxibustion with moxa box was performed for 30 min, once every 3 days, and it was stopped during menstruation.
Acupuncture group: Acupuncture was given on the basis of conventional care.The acupoints, which were selected by the acupuncturist for acupuncture operation, were Tianshu, Qihai, Guangyuan, Zhongji, Ziwu, and Shuidao.The acupuncture was kept for 30 min for each acupoint,once every 3 days, and the needling was stopped during menstruation.
Combined group: Patients were given moxibustion plus acupuncture on the basis of conventional care.The acupoints selected, operation and time of duration of moxibustion and acupuncture were the same as the first two groups.Moxibustion and acupuncture were also operated for patients every 3 days and were stopped during menstruation.
The treatment course of three groups was 3 months in total.
Observation indexes and detection methods
Body mass index (BMI), waist-to-hip ratio (WHR), fasting insulin (FINS), fasting plasma glucose (FPG), homeostasis model assessment-insulin resistance (HOMA-IR), triglycerides (TG),and total cholesterol (TC) were measured before and after 3 months of treatment, respectively.
The TCM Clinical Symptoms Integral Table was prepared by the Guidelines for Clinical Research on New Chinese Medicines[11]and was used to calculate TCM clinical symptom score.The items of TCM Clinical Symptoms Integral Table included late menstruation or amenorrhea, loose stools, aversion to cold, weakness of the waist and knees, mental fatigue, loss of appetite, and dizziness.Each item was rated on 4-point scale from 0 (asymptomatic) to 3 (severe).The higher the score, the more serious the patient’s symptoms.The TCM index = (the pretreatment score - the posttreatment score) ÷ the pretreatment score.The clinical efficacy criteria were as follows: Cured: the patient’s menstrual cycle was restored, clinical symptoms disappeared, and the TCM index was ≥95%; Markedly effective: the patient’s menstrual cycle is close to normal, clinical symptoms basically disappeared, 70%≤ TCM index <95%; Effective: the patient’s menstrual cycle and clinical symptoms improved, 30% ≤ TCM index <70%; Ineffective:the patient’s menstrual cycle and clinical symptoms did not change, and the TCM index was <30%.The total efficiency rate = cured rate + markedly effective rate + effective rate.
The quality of life of patients before and after treatment was assessed using the PCOS Quality of Life Scale,[12]which consists of 5 dimensions with 26 items.Each item was rated on 7-point scale from 1 (worst) to 7 (best).Higher scores indicate higher quality of life.
Reproductive endocrine hormone measurement: 10 mL of blood was collected from elbow vein of patients at 9:00 a.m.on an empty stomach before treatment and on the 2ndto 4thday of the first menstrual cycle after the end of treatment and centrifuged at 3000 r/min for 10 min in a low-speed centrifuge at 4°C.The sera were separated after centrifugation, and follicle-stimulating hormone (FSH),luteinizing hormone (LH), and testosterone (T) were measured by chemiluminescence.
Adverse events
If patients experienced adverse events such as allergy, needle sickness, or burns, the investigator immediately stopped the operation and gave symptomatic treatment.Patients who are unfit to continue to participate would be excluded from the study.
Statistical analysis
All the data were entered into EXCEL table and saved, and SPSS 21.0 statistical software (SPSS, Chicago, IL, USA) was used for statistical processing.The measurement data conforming to normal distribution were expressed as mean ± standard deviation, one-way analysis of variance was used for comparison between groups, paired sample t-test was used for comparison within groups, and rank sum test was used for those not conforming to normal distribution.A difference of statistical significance was indicated by P < 0.05.
RESULTS
Comparison of age and duration of disease among the three groups
All patients completed the study.The age of patients in the moxibustion group was (28.60 ± 2.50) years, and the duration of disease was (14.43 ± 4.23) months; the age of patients in the acupuncture group was (28.90 ± 2.60) years and the duration of disease was (14.83 ± 3.40) months; the age of patients in the combined group was (29.07 ± 2.23) years and the duration of disease was (16.47 ± 4.82) months.There was no difference among patients in the three groups regarding the age (F = 0.280, P = 0.757) and disease duration (F = 1.981,P = 0.144) of patients in the three groups.
Comparison of body mass index and waist-to-hip ratio before and after treatment among the three groups
Before treatment, the differences were not statistically significant when comparing BMI and WHR of patients among the three groups (P > 0.05).After treatment, the BMI and WHR of patients in the combined group were lower than those of the remaining two groups (P < 0.05) [Table 1].
Table 1: Comparison of body mass index and waist-hip ratio among the three groups (±S)
*P<0.05 compared with the same group before treatment.BMI: Body mass index, WHR: Waist-hip ratio
Groups BMl (kg/m2)WHR Before treatment After treatment Before treatment After treatment Moxibustion group 29.15±2.25 25.95±2.10* 0.98±0.08 0.89±0.10*Acupuncture group 29.95±2.29 25.62±2.30* 0.95±0.08 0.82±0.08*Combined group 29.61±2.18 24.38±1.40* 0.97±0.12 0.80±0.09*F 0.968 5.274 0.817 8.246 P 0.384 0.007 0.445 0.001
Comparison of fasting insulin, fasting glucose, and homeostasis model assessment-insulin resistance before and after treatment among the three groups
Before treatment, the comparison of FINS, FPG, and HOMA-IR among the three groups was not statistically significant (P > 0.05).After treatment, the FINS, FPG, and HOMA-IR of patients in the combined group were lower than those of the remaining two groups (P < 0.05) [Table 2].
Table 2: Comparison of fasting insulin, fasting plasma glucose, and homeostasis model assessment-insulin resistance in the three groups (±S)
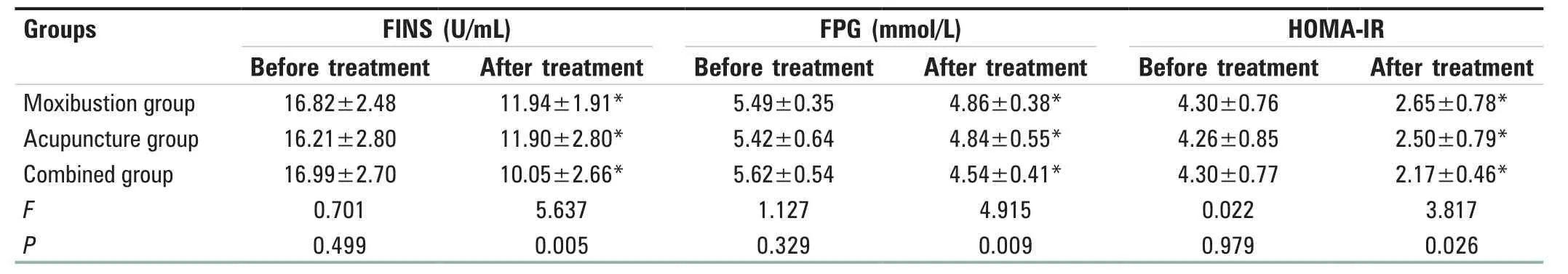
Table 2: Comparison of fasting insulin, fasting plasma glucose, and homeostasis model assessment-insulin resistance in the three groups (±S)
*P<0.05 compared with the same group before treatment.FINS: Fasting insulin, FPG: Fasting plasma glucose, HOMA-IR: Homeostasis model assessment-insulin resistance
Groups FlNS (U/mL) FPG (mmol/L) HOMA-lR Before treatment After treatment Before treatment After treatment Before treatment After treatment Moxibustion group 16.82±2.48 11.94±1.91* 5.49±0.35 4.86±0.38* 4.30±0.76 2.65±0.78*Acupuncture group 16.21±2.80 11.90±2.80* 5.42±0.64 4.84±0.55* 4.26±0.85 2.50±0.79*Combined group 16.99±2.70 10.05±2.66* 5.62±0.54 4.54±0.41* 4.30±0.77 2.17±0.46*F 0.701 5.637 1.127 4.915 0.022 3.817 P 0.499 0.005 0.329 0.009 0.979 0.026
Comparison of follicle-stimulating hormone, luteinizing hormone, and testosterone before and after treatment among the three groups
Before treatment, the differences were not statistically significant when comparing FSH, LH, and T among the three groups of patients (P > 0.05).After treatment, the patients in the three groups FSH, LH, and T levels improved, and the combined group was better than the remaining two groups (P < 0.05) [Table 3].
Table 3: Comparison of follicle-stimulating hormone, luteinizing hormone, and testosterone in the three groups (±S)
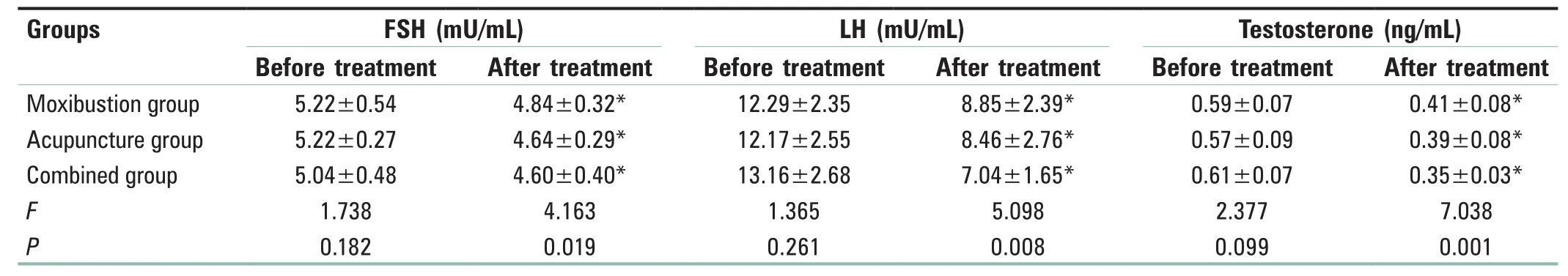
Table 3: Comparison of follicle-stimulating hormone, luteinizing hormone, and testosterone in the three groups (±S)
*P<0.05 compared with the same group before treatment.FSH: Follicle-stimulating hormone, LH: Luteinizing hormone
Groups FSH (mU/mL) LH (mU/mL) Testosterone (ng/mL)Before treatment After treatment Before treatment After treatment Before treatment After treatment Moxibustion group 5.22±0.54 4.84±0.32* 12.29±2.35 8.85±2.39* 0.59±0.07 0.41±0.08*Acupuncture group 5.22±0.27 4.64±0.29* 12.17±2.55 8.46±2.76* 0.57±0.09 0.39±0.08*Combined group 5.04±0.48 4.60±0.40* 13.16±2.68 7.04±1.65* 0.61±0.07 0.35±0.03*F 1.738 4.163 1.365 5.098 2.377 7.038 P 0.182 0.019 0.261 0.008 0.099 0.001
Comparison of triglycerides and total cholesterol before and after treatment among the three groups
Before treatment, the differences were not statistically significant when comparing TG and TC of patients among the three groups (P > 0.05).After treatment, the TG and TC of patients in the combined group were lower than those in the remaining two groups (P < 0.05) [Table 4].
Table 4: Comparison of triglyceride and total cholesterol in the three groups (±S)
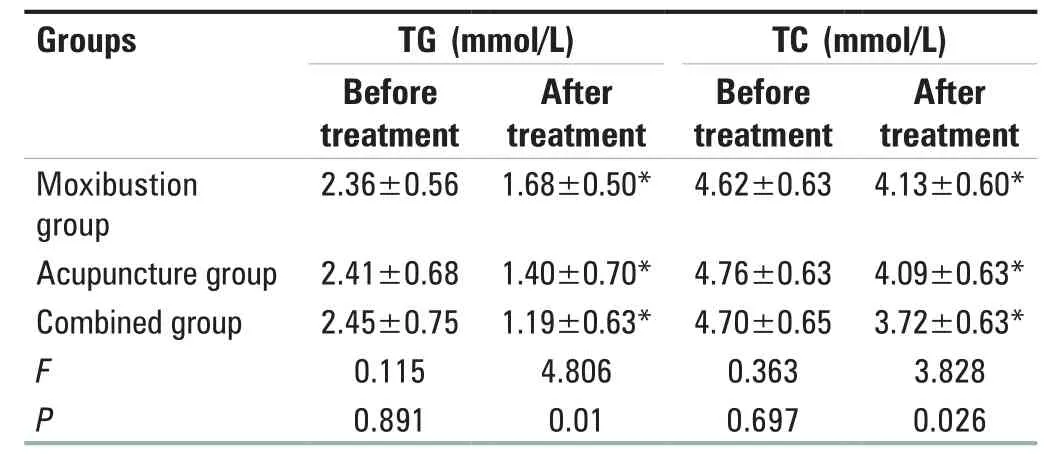
Table 4: Comparison of triglyceride and total cholesterol in the three groups (±S)
*P<0.05 compared with the same group before treatment.TG: Triglyceride, TC: Total cholesterol
Groups TG (mmol/L) TC (mmol/L)Before treatment After treatment Before treatment After treatment Moxibustion group 2.36±0.56 1.68±0.50* 4.62±0.63 4.13±0.60*Acupuncture group 2.41±0.68 1.40±0.70* 4.76±0.63 4.09±0.63*Combined group 2.45±0.75 1.19±0.63* 4.70±0.65 3.72±0.63*F 0.115 4.806 0.363 3.828 P 0.891 0.01 0.697 0.026
Comparison of the traditional Chinese medicine clinical symptom score among the three groups before and after treatment
The TCM clinical symptom score of the patients in the three groups before treatment was comparable (P > 0.05).After treatment, the TCM clinical symptom score of patients in the combined group was significantly lower than those in the moxibustion and acupuncture groups (P < 0.05) [Table 5].
Table 5: Comparison of Traditional Chinese Medicine clinical symptom score among the three groups (±S)
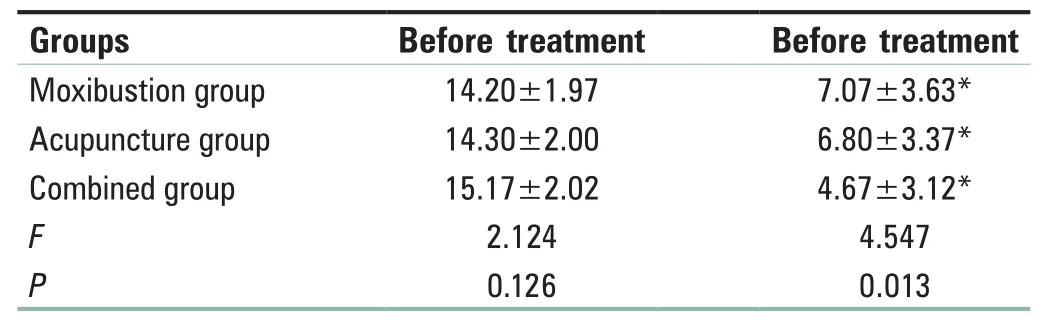
Table 5: Comparison of Traditional Chinese Medicine clinical symptom score among the three groups (±S)
*P<0.05 compared with the same group before treatment
Groups Before treatment Before tre Moxibustion group 14.20±1.97 7.07±3 Acupuncture group 14.30±2.00 6.80±3 Combined group 15.17±2.02 4.67±3 F 2.124 4.54 P 0.126 0.01?atment.63*.37*.12*7 3
Comparison of the quality of life score among the three groups before and after treatment
The quality of life score of patients in the three groups before treatment were comparable (P > 0.05).After treatment, the quality of life of patients in the combined group improved more significantly compared to the moxibustion and acupuncture groups (P < 0.05) [Table 6].
Table 6: Comparison of quality of life score among the three groups (±S)
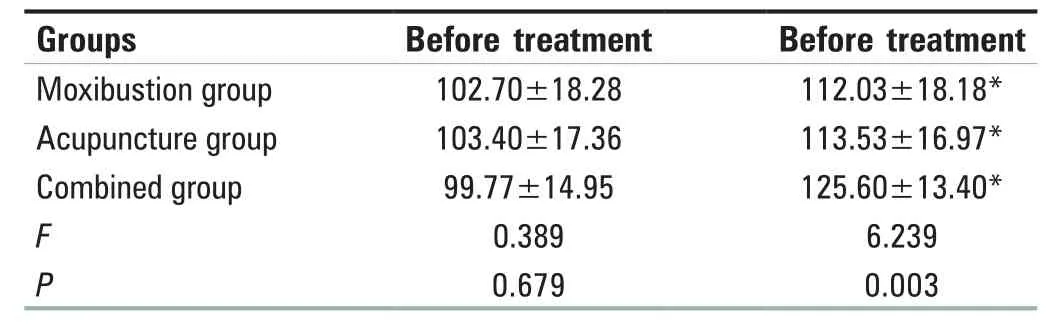
Table 6: Comparison of quality of life score among the three groups (±S)
*P<0.05 compared with the same group before treatment
Groups Before treatment Before treatment Moxibustion group 102.70±18.28 112.03±18.18*Acupuncture group 103.40±17.36 113.53±16.97*Combined group 99.77±14.95 125.60±13.40*F 0.389 6.239 P 0.679 0.003
Comparison of the comprehensive efficacy of the three groups
The total effective rate of the combined group was higher than that of the moxibustion and acupuncture groups,and the difference was statistically significant (χ2= 6.947,P = 0.031) [Table 7].
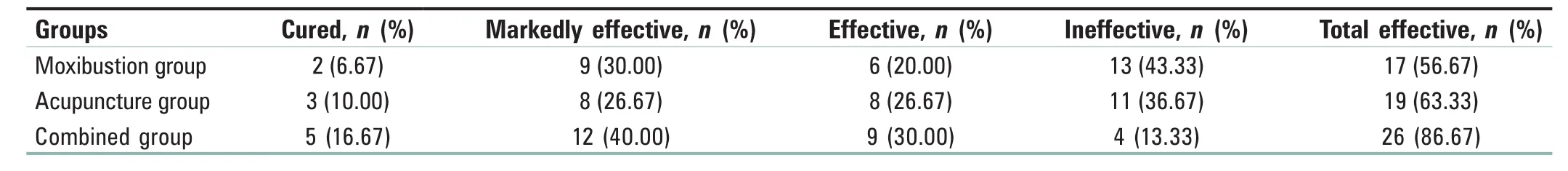
Table 7: Comparison of the efficacy among the three groups
DISCUSSION
PCOS is one of the most common syndromes in gynecology with multiple causes and polymorphisms.[13,14]The geographical location of Shaanxi where the patients selected in this study live makes the winter climate cold and dry.From the perspective of Chinese medicine, cold is a Yin evil which is most likely to injure the kidney yang which is the root cause of patients having PCOS.[15]Moreover, most patients are stressed and overthinking, have irregular lifestyles, and like to eat raw and cold foods, which leads to weakness of the spleen and damage to spleen yang.Hence, patients with PCOS eventually suffer spleen-kidney yang deficiency as the main pathogenesis, manifesting as scanty menstruation or menopause, infertility, aversion to cold, obesity, and fatigue.[16]The Jingyue Encyclopedia said, “People with deficiencies of the spleen and kidneys have a lot of accumulation of disease.”[17]Deficiency of kidney yang and spleen yang leads to loss of warmth of the uterus and poor flow of qi and blood, resulting in disorders of the menstrual cycle and inability to take in sperm to become pregnant.[18]Some researchers have pointed out that infertility and obesity are the main causes of poor quality of life in patients with PCOS.[19,20]The disease is long and extensive throughout the cycle, therefore, it is essential to improve the quality of life of patients with PCOS by improving their immediate clinical symptoms and fertility problems while minimizing adverse effects and complications.
Acupuncture and moxibustion are both traditional Chinese medical care techniques that have shown to be effective in treating patients with PCOS.Acupuncture is a multi-layer technique.The acupuncture is an effective method to stimulate specific acupoints in PCOS patients through multiple layers and targets to achieve a state of Yin and Yang balance, as well as to harmonize the body and mind to bring several functions into balance.[21]Modern medicine has confirmed that acupuncture at the corresponding acupoints can regulate the hypothalamic-pituitary-ovarian reproductive axis, modulate the ovarian microenvironment, improve endocrine and metabolic disorders in PCOS patients, thus help them restore ovulation, improve reproductive function,and effectively reduce the incidence of complications.[22,23]Feng et al.[24]also found that acupuncture was effective in improving the anxiety of patients with PCOS by regulating the mood and improving their physical and mental health and quality of life.Moxibustion is also one of the treatment methods for this disease, and the modified moxibustion with moxa box, to some extent, compensates for the shortcomings of traditional moxa strips such as limited area of application and low heating power.Moxa leaves are bitter and warm in property and distribute to the spleen and kidney meridians, with the effects of warming Yang,dispelling cold, and promoting Qi and blood circulation,thus regulating hormone levels by combining the warming effect of moxa-box moxibustion and the medicinal effect of moxa leaves to remove blood stasis and smooth the flow of Qi and blood.[25]Wang et al.[26]found that moxibustion on the corresponding acupionts in the lower abdomen of women can promote metabolism, reduce the patient’s weight, enhance local blood perfusion in the endometrium, and promote the recovery of the menstrual cycle.
In this study, Shenque, Tianshu, Qihai, Guanyuan, Zhongji,Zigong, Shuidao, Zhonggui, and Xiegui were selected as key acupoints for the treatment of PCOS,[27]because the abdomen is the place where all meridians meet and is the main place where phlegm and dampness gather and Qi and blood are blocked, and the uterus is located in the lower abdomen, so moxibustion of the lower abdomen can treat the disease from its source.Shenque acupoint is located in the umbilicus and is adjacent to the stomach and intestines, which can warm Yang and disperse cold, harmonize the stomach and strengthen the spleen.Tianshu acupoint governs the collection of Qi and blood in the large intestine meridian, which has the effect of raising the clear Qi and lowering the turbid Qi, harmonizing the temperature and blood.Qihai acupoint is the place where the primordial qi gathers, which can tonify Qi and benefit the kidney, astringe essence and consolidate the essence.Guanyuan acupoint belongs to the Ren meridian (conception vessel), which is the location of blood storage in women, and can cultivate primordial Qi and consolidate essence, and is a common acupoint to regulate qi and blood; Zhongji acupoint is located 4 inches below the umbilicus, which has the effect of tonifying the kidney and regulating the menstruation,regulating blood and warming the uterus.Zigong acupoint is often used to treat gynecological disorders such as menstrual disorders, dysmenorrhea, and infertility.The Shuidao acupiontis located on the stomach meridian of foot Yangming, which can tonify the kidneys, strengthen the spleen, and invigorate the meridians.[28,29]The shared administration of moxibustion on acupoints can strengthen their effects of warming the meridians and dispersing cold, warming the Ren and Dai channels, warming the kidneys and strengthening the spleen, and balancing Yin and Yang, which, together with the stimulation of the acupuncture points by acupuncture, can unblock the meridians, regulate endocrine secretion, adjust the menstrual cycle, restore ovarian ovulation, improve the TCM symptoms, and improve clinical efficacy.[30,31]
Therefore, the effect of combining moxibustion with acupuncture on the efficacy and quality of life of spleen-kidney-yang-deficiency patients with PCOS was significant.After treatment, the combination of moxibustion and acupuncture was more effective in reducing BMI and WHR of PCOS patients compared with the moxibustion and acupuncture groups, indicating that the combination of moxibustion and acupuncture was more effective in promoting blood circulation and lipolysis, strengthening the metabolic function of the body, and improving the body shape of patients; the FINS, FPG, HOMA-IR, TG, and TC of the three groups were reduced, and the effect of the combination group was more obvious in the combined group,indicating that moxibustion combined with acupuncture therapy is more advantageous in correcting the disorders of glucolipid metabolism in PCOS patients.The levels of FSH,LH, and T in the combined group were better than those in the remaining two groups, indicating that moxibustion combined with acupuncture therapy can better regulate the sex hormone levels in PCOS patients, thus promoting the recovery of menstrual cycle.The TCM clinical symptom score in the combined group was significantly lower than those in the remaining two groups, and the quality of life and overall efficiency were significantly higher than those of the remaining two groups, indicating that moxibustion combined with acupuncture therapy could effectively improve the clinical symptoms, enhance the treatment effect and the quality of life of PCOS patients.The results of this study are similar to those of Zhang et al.,[32]Duan et al.,[33]and Lin et al.[34]who prove that the combined application of acupuncture and moxibustion can regulate menstrual status, tonify the kidneys and strengthen the spleen to a greater extent, thus warm the uterus and promote pregnancy in patients with PCOS.
CONCLUSION
In conclusion, compared to the moxibustion group and acupuncture groups, moxibustion combined with acupuncture group can effectively reduce BMI and WHR in patients with PCOS, improve endocrine function, sex hormone levels, TCM symptoms and quality of life.However, due to the limitations of this study such as small sample size, short-term observation period, and only conducted in one hospital, the applicability of the combined group in other hospitals could not be fully demonstrated.Therefore, in future studies, researchers should expand the sample size as much as possible and combine multiple hospitals to conduct the trial together in order to obtain more authoritative results.
Declaration of patient conform
The informed consent has been obtained from all patients included in this study.In the form, the patients have given their consent for clinical information to be reported in the journal.The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by Shaanxi University of TCM Hospital Research Projects (2020HL006).
Conflicts of interest
There are no conflicts of interest.
 Journal of Integrative Nursing2021年4期
Journal of Integrative Nursing2021年4期
- Journal of Integrative Nursing的其它文章
- lnsigni ficant small can still be mighty: Trend of chronic kidney disease in Nigeria
- Relationship of demoralization with anxiety, depression,and demographics of Chinese dialysis patients
- Application of five-element music therapy in pain coping skills training in patients with knee osteoarthritis
- A study on the correlation between function motivation and professional identity among nursing volunteers
- Self-management of cataract extraction among diabetes patients
- Knowledge on malaria among caregivers with children aged under 5 years at Kenyasi Health Center
