A rare case of severe toxic optic neuropathy induced by formaldehyde vapor under working in mushroom cultivation room
Min Gong, Yan-Nian Hui, Hong-Jun Du
Dear Editor,
We are writing this letter to present a rare case of severe toxic optic neuropathy induced by formaldehyde (FA)vapor under working in mushroom cultivation room. Since such circumstance exists popularly in rural China, this case warns us to pay more attention to avoid similar cases.
A 49-year-old male complained of bilateral vision loss after continuous working for 11h in an air-tight greenhouse filled with FA vapor on 03/15/2018. Soon after work, the patient felt weakness, dizziness, and nausea. Instead of asking for medical consultation, he went home to sleep. The next day, the patient was found to be in a coma with dyspnea and was taken to the local hospital by his family. His blood pressure waved around 70-80/50-65 mm Hg, and then maintained at 100/80 mm Hg by catecholamines. He was diagnosed with acute FA poisoning, pulmonary edema, metabolic acidosis, respiratory alkalosis, and hypotension and was given symptomatic relief and supportive measures. On 03/18/2018,he regained consciousness and found his bilateral vision decreased to count fingers. Supplementarily, FA-induced toxic optic neuropathy was diagnosed. However, no systematic treatment for visual impairment was received. Later, the patient suffered from anxiety and insomnia, weight losing, intermittent chest pain, and acroanesthesia.
To seek further ophthalmic diagnosis and treatment, he was referred to our hospital on 04/28/2018. At the time of consultation, his eyesight was light perception in both eyes.Anterior segment examination revealed bilateral 5-mm,dilated, and sluggishly reactive pupils. The rest of anterior segments was normal. Fundus examination showed bilateral pallor optic discs with clear demarcation and 0.5 of the cupto-disc ratio. Also, attenuation of the vasculature was noticed(Figure 1A1, 1B1). B ultrasonic examination revealed rough reflex from the posterior pole and shrunken optic disc in both eyes (Figure 1A2, 1B2). Optical coherence tomography(OCT) of the retinae showed thinning of the nerve fiber layer (Figure 1A3, 1B3). Fluorescence fundus angiography(FFA) showed normal retina perfusion but fewer capillaries on the surface of the optic disc (Figure 1A4, 1B4). Visual electrophysiological examination results displayed decreased amplitude of the flash-electroretinogram (F-ERG) in right eye and significant decreased amplitude of the flash-visual evoked potential (F-VEP) in both eyes. The pattern-visual evoked potential (P-VEP) was not detected due to poor vision(Table 1). Magnetic resonance imaging (MRI) demonstrated abnormal signals in the bilateral frontal cortex and basal ganglia (Figure 2A, 2B), which prompting possible metabolic diseases and poisoning. Diffusion-weighted imaging (DWI;Figure 2C) signal was slightly higher in the bilateral frontal lobe, parietal lobe, bilateral side ventricle. No obvious abnormality was noticed in orbital enhanced MRI (Figure 2D).Electroencephalography (EEG) revealed that α and β waves were symmetrically distributed in each function area and 0.42-0.35 μV. δ waves were mainly inspected in the frontal area,which indicating slightly abnormal neurological electrical activities[1]. Based on the above test results, toxic optic neuritis and neuratrophy caused by FA were diagnosed.
Prednisone acetate (60 mg/d) was then applied orally for one week, followed by a weekly reduction of 5 mg till withdrawal.Other treatments, including 1.5 mg/d of mecobalamin tablets and 20 mg/d of vitamin B6 tablets, and hyperbaric oxygen therapy were given for 4wk. At the end of the treatment,his systemic symptoms disappeared except for fatigue and acroanesthesia. However, his bilateral vision did not improve.

Figure 1 Examinations of the right eye (A1-A4) and the left eye (B1-B4) A1, B1: Paled optic discs with a clear boundary, and 0.5 of the cup-to-disc ratio; A2, B2: B ultrasonic examination revealed rough reflex from the posterior pole and shrunken optic disc; A3, B3: OCT scans of the maculae showed the thinning of nerve fiber layer; A4, B4: FFA examination demonstrated the reduced fluorescence and fewer capillaries around the optic discs.
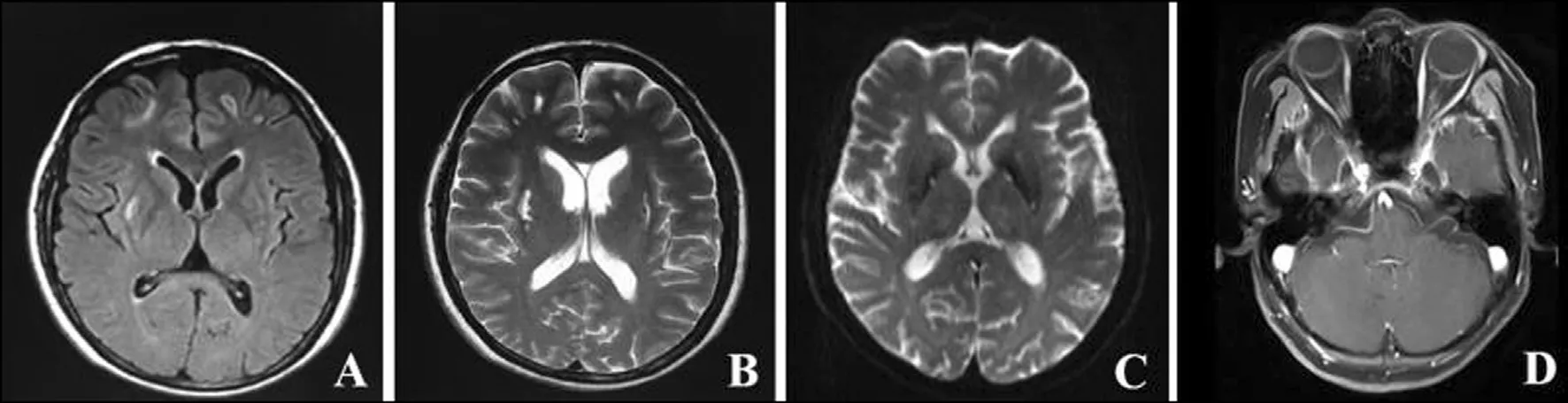
Figure 2 Different MRI sequences of the brain A, B: Long T1 and long T2 showed signals in bilateral frontal cortex and the bilateral basal ganglia; C: DWI signal showing slightly hyperintensity in the bilateral frontal lobe, parietal lobe, bilateral side ventricle; D: Enhanced MRI indicating the normal orbital structure.

Table 1 Analysis of the electroretinogram and visual evoked potential
DISCUSSION
FA is a pungent, flammable, and colorless gas, which is widely used in environmental and industrial activities such as space disinfectant, adhesives, melamine formaldehyde resins, particle or fiber wood board, and cosmetics production.People can expose to FA occupationally or residentiallyviathe airway, digestive tract or skin. The occupational formaldehyde exposure limit is 0.94 mg/m3or less than 0.94 mg/m3on an 8-hour time-weighted average, and the short-term exposure limit is 2.5 mg/m3[2-3]. FA is normally present in both indoor and outdoor spaces, and inhalation at a lower level is the most common way of contact[4]. Given its widespread use, volatility and toxicity, FA has been classified as a known human carcinogen by the World Health Organization and International Agency for Research on Cancer[3,5].
Acute FA intoxication is defined mainly as injures induced by exposing to high concentration FA in a short time. Mucosal injury is the most common toxic effect, often leading to irritated eyes, tearing, coughing, sneezing, chest congestion,asthma, fever, lethargy, skin sensitization and dermatitis[1,3].There are many reports of central nervous system damage caused by acute FA exposure, while FA-induced optic neuropathy had been rarely reported.
After working for 11h in an air-tight inoculation room filled with high concentrations of FA vapor, which was used to sterilize the room, this patient developed dizziness, nausea,drowsiness, coma, and later found severe vision loss.Since the patient came to our hospital too late, we did not get chance to test the concentration of the FA vapor in the mushroom cultivation room. Based on his medical history,general manifestations and the ophthalmic examinations (vision,ocular fundus, OCT and visual electrophysiology), acute FA poisoning and toxic optic neuritis were diagnosed. Wanget al[6]once reported a case of severe vision loss due to two days staying in a newly renovated house. Combined with the results of room formaldehyde and benzene tests, the patient was diagnosed as acute toxic optic neuritis. However, due to the presence of toxic benzene gas, FA could not be determined as the only cause of optic nerve damage in this patient.
After being absorbed, FA can be oxidized into formal acid and methanol, and cause further tissue damages[7-9]. As FA can pass through the blood-brain barrier, it may affect the central nervous system function, lead to emotional or cognitive behavior alternation[7,10-13]. Hayasakaet al[14]found that FA, methanol and formic acid had toxic effect on the optic nerve and retina when injected intravitreally, while FA was the most toxic one. Regarding the mechanism involved,in vitroandin vivostudies showed that FA exposure leads to enhanced reactive oxygen species (ROS) generation, reduced glutathione (GSH), elevated level of tumor necrosis factor alpha (TNF-α), interleukin-1 beta (IL-1β), and caspase-3, thus to induce subsequent oxidative stress, inflammatory responses,mitochondrial dysfunction, cytochrome C release, caspase cascade activation, cell apoptosis, and necrosis[1-2,15-19]. Using CRISPR-based functional genomics screening method, a newly study suggested the potential roles of one-carbon metabolism,fatty acid synthesis and mTOR signaling in FA toxicity[20].
In term of treatment, high dose of systemic glucocorticoid is currently considered to be the most important and effective treatment[21]. Recent studies found that the combination of erythropoietin with corticosteroid might achieve a stronger protective effect at the beginning[22-23]. FA-induced mitochondrial dysfunction leads to a depletion of adenosine triphosphate (ATP), which is involved in many essential biological processes. Studies showed that intravenous ATP administration significantly prevented the oxidative stress and histological destruction in optic nerve tissue. As this patient was in a coma, his visual impairment could not be identified at the beginning, so the initial treatments were mainly focused on systemic symptoms. Later, even comprehensive treatments such as glucocorticoid and hyperbaric oxygen therapy were given, his vision did not improve.
FA is now widely used in agricultural and industrial activities.This case reminds us that enough attention needs to be paid,and corresponding preventive measures need to be taken to avoid the similar cases. In addition, the possibility of FAinduced optic nerve damage should be considered in such situation, and the necessary treatment should be applied at the very beginning, especially when the patient is in a coma.
ACKNOWLEDGEMENTS
Conflicts of Interest:Gong M, None; Hui YN, None; Du HJ,None.
 International Journal of Ophthalmology2021年12期
International Journal of Ophthalmology2021年12期
- International Journal of Ophthalmology的其它文章
- Comparison of trifocal toric and bifocal toric intraocular lens implantation in patients with cataract and high corneal astigmatism
- Comparison of perioperative parameters in one-handed rotational phacoemulsification versus conventional phacoemulsification and femtosecond laser-assisted cataract surgery
- Decreased retinal microvasculature densities in pterygium
- Fourier analysis of corneal Scheimpflug imaging: clinical use in keratoconus
- Establishment of a prediction tool for ocular trauma patients with machine learning algorithm
- Role of orthoptics and scoring system for orbital floor blowout fracture: surgical or conservative treatment
