产前超声测量肺头比评估胎儿肺囊腺瘤样畸形预后的价值
陈淑华 龚炜 梁倩虹
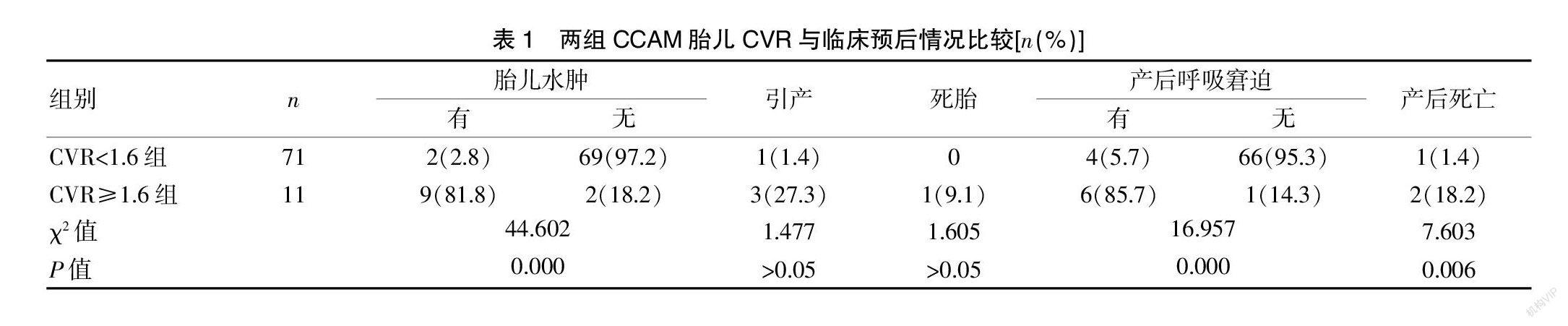
[摘要] 目的 通过产前超声测量CCAM胎儿肺头比(CVR),探讨CVR在CCAM胎儿预后评估中的价值。 方法 选取2018年1—12月广州市番禺区妇幼保健院进行产前超声测量肺头比评估胎儿肺囊腺瘤样畸形预后的胎儿82例,均为产前超声诊断为CCAM,测量胎儿CVR,分为CVR<1.6组和CVR≥1.6组,观察并比较产前超声声像图特征及分型、随访结果及临床预后。 结果 在82例CCAM胎儿中,女胎29例,男胎53例;肿块位于左肺48例,右肺34例;CCAM Ⅰ型17例,CCAM Ⅱ型41例,CCAM Ⅲ型24例。82例CCAM胎兒均可显示肺部肿块血供来源自肺动脉。CVR<1.6组胎儿水肿有2例(2.8%),无69例(97.2%),引产1例(1.4%),死胎0例,产后发生呼吸窘迫4例(5.7%),无66例(95.3%),产后死亡1例(1.4%);CVR≥1.6组胎儿水肿有9例(81.8%),无2例(18.2%),引产3例(27.3%),死胎1例(9.1%),产后发生呼吸窘迫6例(85.7%),无1例(14.3%),产后死亡2例(18.2%),因此,CVR<1.6组及CVR≥1.6组在胎儿水肿、产后呼吸窘迫及产后死亡发生率方面比较,差异有统计学意义(P<0.05)。 结论 CVR≥1.6的CCAM胎儿水肿发生率及产后呼吸窘迫发生率均升高,CVR是产前评估胎儿CCAM预后的有效指标。
[关键词] 肺囊腺瘤样畸形;产前超声;预后;测量肺头比;胎儿
[中图分类号] R714 [文献标识码] B [文章编号] 1673-9701(2021)24-0074-04
Value of prenatal ultrasound measurement of volume-to-head ratio in evaluating the prognosis of fetal congenital cystic adenomatoid malformation
CHEN Shuhua GONG Wei LIANG Qianhong
Department of Ultrasound, He Xian Memorial Hospital in Panyu District of Guangzhou, Panyu Maternal and Child Care Service Centre of Guangzhou, Guangzhou 511400, China
[Abstract] Objective To measure the fetal congenital cystic adenomatoid malformation (CCAM) volume-to-head ratio (CVR) by prenatal ultrasound,and to explore the value of CVR in evaluating the prognosis of CCAM fetus. Methods A total of 82 fetuses who were diagnosed as CCAM in Panyu Maternal and Child Care Service Centre of Guangzhou from January 2018 to December 2018 by prenatal ultrasound were selected as objects. After measuring CVR,they were divided into CVR<1.6 group and CVR≥1.6 group. Prenatal ultrasound features and classification,follow-up results and clinical prognosis were compared between two groups were observed and compared. Results Among 82 CCAM fetuses, there were 29 females and 53 males. The lump was located in the left lung in 48 cases and the right lung in 34 cases. There were 17 cases of type Ⅰ CCAM, 41 cases of type Ⅱ CCAM and 24 cases of type Ⅲ CCAM. All 82 cases of CCAM fetuses showed that the blood supply of lung mass came from pulmonary artery. In CVR<1.6 group,there were 2 cases (2.8%) of fetal edema, 69 cases (97.2%) without fetal edema, 1 case (1.4%) of induced labor, 0 case of stillbirth, 4 cases (5.7%) of postpartum respiratory distress, 66 cases (95.3%) without fetal edema and 1 case of postpartum death (1.1%). In CVR≥1.6 group, there were 9 cases(81.8%) of fetal edema, 2 cases(18.2%) without fetal edema, 3 cases (27.3%) of induced labor, 1 case (9.1%) of stillbirth, 6 cases (85.7%) of postpartum respiratory distress, 1 case (14.3%) of non-abortion, and 2 cases (18.2%) of postpartum death. Therefore, there were statistical differences in edema rate, postpartum respiratory distress rate and postpartum death rate between CVR<1.6 group and CVR≥1.6 group (P<0.05). Conclusion The incidences of fetal edema and postpartum respiratory distress in CCAM with CVR≥ 1.6 are increased, which show that CVR is an effective indicator for prenatal evaluation of fetal CCAM prognosis.