Efficacy and safety of endoscopic transpapillary gallbladder drainage in acute cholecystitis:An updated meta-analysis
David M Jandura,Srinivas R Puli
David M Jandura,Department of Gastroenterology,University of Illinois College of Medicine at Peoria,Peoria,IL 61637,United States
Srinivas R Puli,Department of Gastroenterology and Hepatology,University of Illinois College of Medicine at Peoria,Peoria,IL 61637,United States
Abstract BACKGROUND Percutaneous transhepatic gallbladder drainage has been the most frequently performed treatment for acute cholecystitis for patients who are not candidates for surgery.Endoscopic transpapillary gallbladder drainage (ETGBD) has evolved into an alternative treatment.There have been numerous retrospective and prospective studies evaluating ETGBD for acute cholecystitis,though results have been variable.AIM To evaluate the efficacy and safety of ETGBD in the treatment of inoperable patients with acute cholecystitis.METHODS We performed a systematic review of major literature databases including PubMed,OVID,Science Direct,Google Scholar (from inception to March 2021) to identify studies reporting technical and clinical success,and post procedure adverse events in ETGBD.Weighted pooled rates were then calculated using fixed effects models for technical and clinical success,and post procedure adverse events,including recurrent cholecystitis.RESULTS We found 21 relevant articles that were then included in the study.In all 1307 patients were identified.The pooled technical success rate was 82.62% [95%confidence interval (CI):80.63-84.52].The pooled clinical success rate was found to be 94.87% (95%CI:93.54-96.05).The pooled overall complication rate was 8.83%(95%CI:7.42-10.34).Pooled rates of post procedure adverse events were bleeding 1.03% (95%CI:0.58-1.62),perforation 0.78% (95%CI:0.39-1.29),peritonitis/bile leak 0.45% (95%CI:0.17-0.87),and pancreatitis 1.98% (95%CI:1.33-2.76).The pooled rates of stent occlusion and migration were 0.39% (95%CI:0.13-0.78) and 1.3% (95%CI:0.75-1.99) respectively.The pooled rate of cholecystitis recurrence following ETGBD was 1.48% (95%CI:0.92-2.16).CONCLUSION Our meta-analysis suggests that ETGBD is a feasible and efficacious treatment for inoperable patients with acute cholecystitis.
Key Words:Endoscopic transpapillary gallbladder drainage;Acute cholecystitis;Inoperable treatment;Double pigtail stent;Nasobiliary drainage
INTRODUCTION
Cholelithiasis is a common condition that affects 6% of men and 9% of women in the United States[1].Acute cholecystitis is a syndrome of right upper quadrant abdominal pain,fevers and leukocytosis that is associated with inflammation of the gallbladder.Occurring in about 6%-11% of patients with symptomatic gallstones,it is the most common gallbladder syndrome[2].The standard of care treatment for acute cholecystitis is antibiotic therapy and definitive surgical intervention with cholecystectomy.For patients unsuitable for surgery,the ideal choice has been percutaneous transhepatic drainage.
Percutaneous drainage is well established in the literature with strong technical success rates of nearly 97%,and with more variable clinical response rates ranging from 56%-100%[3-5].Though effective,complications related to externalized drainage including bile leakage,peritonitis,bleeding and catheter misplacement/removal have been noted[6].Patient satisfaction and quality of life have also been of concern,with patient discomfort occurring in up to 25% of patients[7].Coagulopathy and decompen-sated liver disease with ascites have also been contraindications to percutaneous drainage[8,9].Another drawback to percutaneous drainage is that it may be an impermanent solution.Patients who did not undergo cholecystectomy following percutaneous catheter removal had significant recurrence rates of cholecystitis ranging from 22%-47%[10,11].
Endoscopic techniques for gallbladder drainage have been evaluated in inoperable patients with cholecystitis who are not suitable for percutaneous drainage.Two endoscopic approaches to gallbladder drainage exist,they include a transmural approach performed with endoscopic ultrasound (EUS),and endoscopic transpapillary gallbladder drainage (ETGBD) which utilizes endoscopic retrograde cholangiopancreatography (ERCP).EUS guided gallbladder drainage was first described in 2007,with well-established efficacy.Technical and clinical success rates of 84.6%-100% and 86.7%-100% respectively have been demonstrated[12,13].Drawbacks,such as the need for a high level of expertise,procedure costs and the risk of adverse events in the setting of technical failure,have been noted.The development of lumen opposing stents (LAMS) has improved the feasibility and efficacy and has helped to decrease the rate of procedure related complications.Nevertheless,there is uncertainly of the effects of retained LAMS and its contribution to adverse events as well as its effect on future surgical options.
Transpapillary gallbladder drainage is an important option for inoperable patients requiring treatment of acute cholecystitis.It consists of ERCP bile duct cannulation followed by endoscopic transpapillary gallbladder stenting or endoscopic nasobiliary gallbladder drainage (ENGBD).Both approaches have been useful in patients with concomitant choledocholithiasis or in the presence of biliary stricture.Unlike ENGBD,a transpapillary approach has evolved as an especially advantageous method due to its relatively non-invasive nature with improved patient quality of life without the need for externalized drainage.Drawbacks to this method include the potential for post ERCP complications,along with the technical difficulty of the procedure itself,though there have been variable results in the literature.We performed a systematic review including more recent studies evaluating ETGBD in inoperable patients with acute cholecystitis.We present an updated meta-analysis evaluating the technical and clinical success of ETGBD.We also evaluate the safety of ETGBD by analyzing pooled rates of procedural adverse events.
MATERIALS AND METHODS
Search methodology
We performed a literature search using the electronic database engines PubMed,OVID,ScienceDirect,Google scholar from inception to March 2021 to identify published articles and reports which addressed the use of ETGBD as treatment for acute cholecystitis.The search terms “endoscopic transpapillary gallbladder drainage”,“acute cholecystitis”,“complications”,“technical success”,“clinical success”,“adverse events” in different combinations were used.The reference lists of eligible studies were reviewed to identify additional studies.The retrieved studies were carefully examined to exclude potential duplicates or overlapping data.Resultant titles and abstracts were selected from the initial search,they were scanned,and the full papers of potential eligible studies were reviewed.
Study eligibility
The relevance of the studies was initially screened based on title,abstract and the full manuscript.Published studies were eligible for inclusion if they reported the use of ETGBD for the treatment of acute cholecystitis.Studies that evaluated technical and clinical success,along with procedure related adverse events were included.Articles were excluded if they were not available in English,or if they did not have reported outcomes.In studies that compared multiple methods of treatment for acute cholecystitis,data from the cohort of patients who underwent EGTBD were collected and analyzed.Each article title and abstract was reviewed by two investigators(Jandura DM and Puli SR).They obtained full articles that met the inclusion and exclusion criteria,and after an independent review of the full content of each article,they extracted the data.Any differences were resolved by mutual agreement.The agreement between reviewers gave a Cohen’s κ 1.0.
Data extraction and quality assessment
The following data was independently abstracted into a standardized form:Study characteristics (primary author,year of publication),study design,baseline characteristics of study population (number of patients enrolled,patient demographics) and intervention details (procedure indications) and outcomes (technical and clinical success,adverse events).The risk of bias was rated by two authors independently.
Outcome definition
The primary outcome of interest was assessment of ETGBD efficacy in terms of technical and clinical success.Clinical success was calculated based on the cohort of patients that achieved technical success in each study.The secondary outcomes that were assessed were overall and individual procedure related adverse events,and the rates of recurrent cholecystitis following the intervention.
Statistical analysis
This meta-analysis was performed by calculating pooled proportions.First,the individual study proportions was transformed into a quantity using a Freeman-Tukey variant of the arcsine square root transformed proportion.The pooled proportion was calculated as the back-transform of the weighted mean of the transformed proportions,using inverse arcsine variance weights for the fixed effects model and DerSimonian-Laird weights for the random effects model[14,15].Forest plots were drawn to show the point estimates in each study in relation to the summary pooled estimate.The width of the point estimates in the forest plots indicates the assigned weight to that study.The effect of publication and selection bias on the summary estimates was tested by the Harboud-Egger indicator[16].Also,funnel plots were constructed to evaluate potential publication bias[17,18].
RESULTS
Study selection
In summary,21 studies identified by our search using the literature databases were included for our analysis.A flow diagram of this systematic review is included in Figure 1.

Figure 1 Flowchart of search results.
Characteristics of the included studies
In all,8 studies were performed in Japan,6 were performed in the United States,and 4 were performed in South Korea.3 of the remaining studies included in our metaanalysis were originally performed in Germany,Denmark and Italy.Most of the studies were retrospective,however prospective and one random controlled trial was included.
Participants
A total of 1307 patients from 21 studies were included in the meta-analysis.In this meta-analysis,61.44% of the patients included were males and 38.56% were females.The median age of study subject was 68.41 (range:48.5-79.7).
Interventions
ETGBD was performed in inoperable patients with acute cholecystitis with placement of a double pigtail stent in 57.1% of studies.Plastic stents were used in 40.0% of studies.Nasobiliary stenting was performed in 45.0% of the studies included in the meta-analysis.
Outcomes
Technical success was reported by all the studies included in the analysis.The prevalence of successfully performed procedures ranged from 70.59%-100%.The pooled rate of technical success of ETGBD was 82.62% [95% confidence interval (CI):80.63-84.52].The individual study rates and the pooled proportion of technical success is shown as a forest plot in Figure 2.
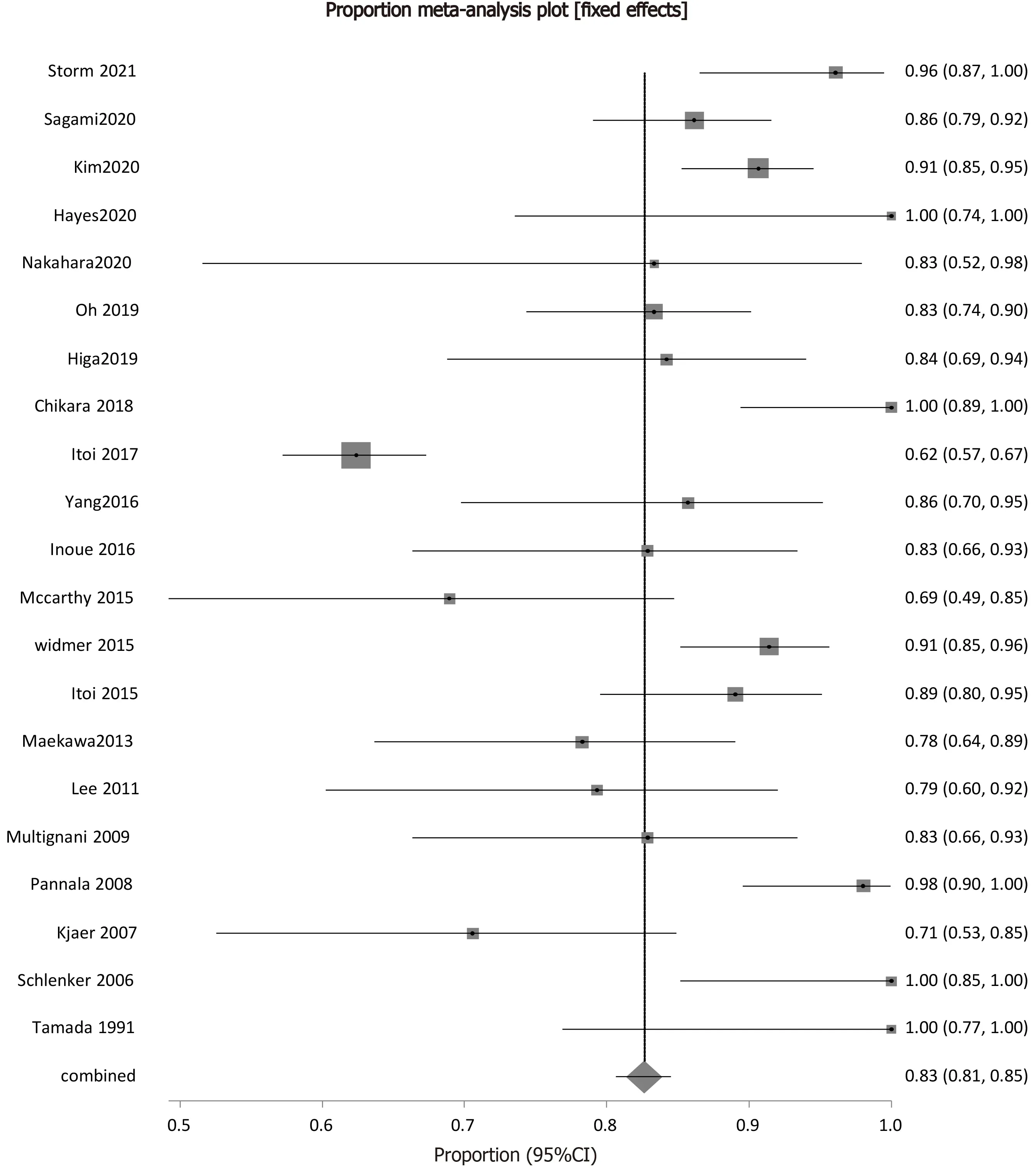
Figure 2 Forest plot showing the individual study proportions of endoscopic transpapillary gallbladder drainage technical success in relation to the pooled rate[7,9,22,24-40].
Efficacy
Procedure efficacy,as represented by clinical success was described by all the studies included in the analysis.Prevalence of ETGBD efficacy in successful treatment of cholecystitis ranged from 64.29%-100%.The pooled proportion of clinical success of ETGBD was 94.87% (95%CI:93.54-96.05).Figure 3 shows the forest plot of the pooled proportion of clinical success.
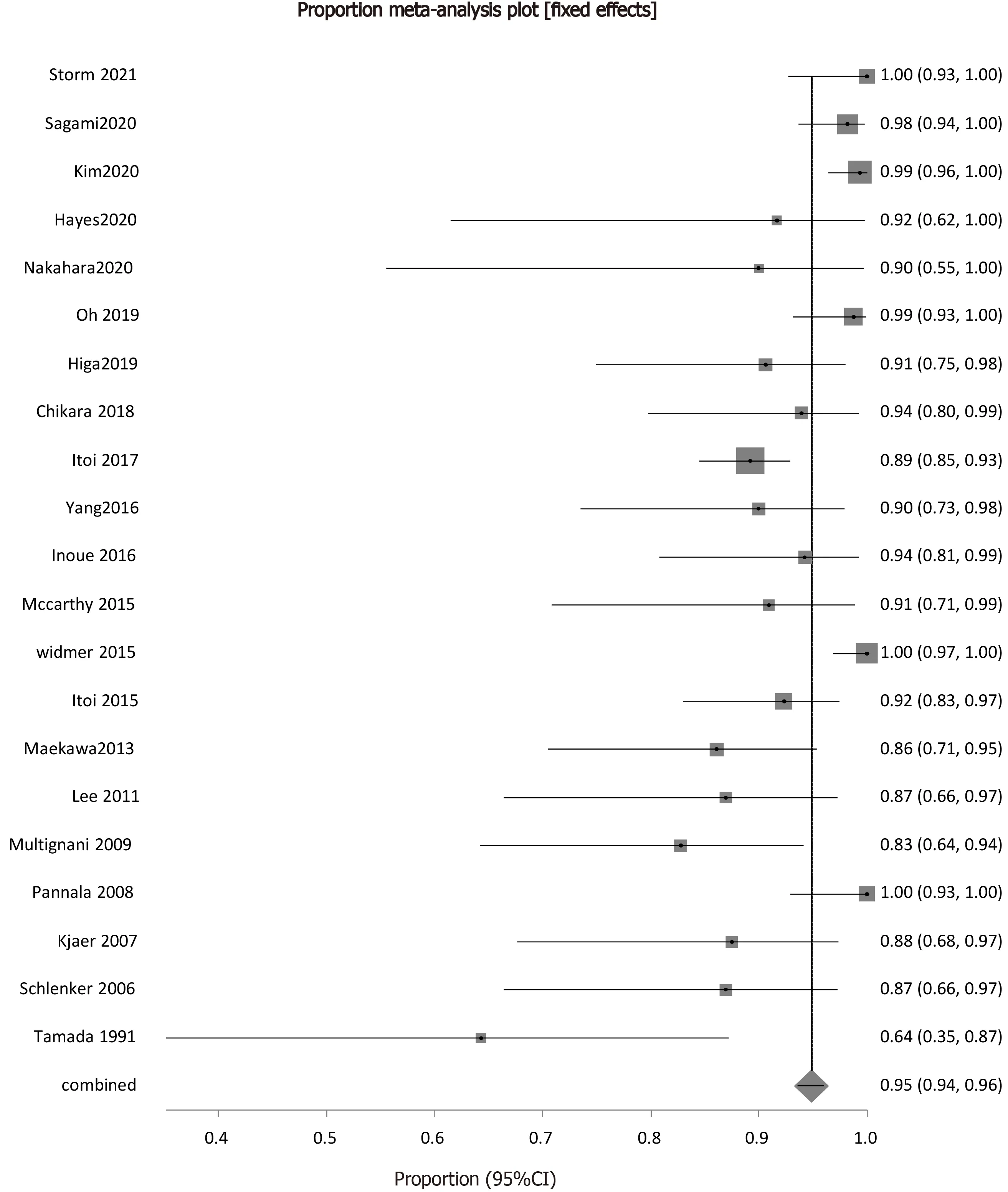
Figure 3 Forest plot showing the individual study proportions of endoscopic transpapillary gallbladder drainage clinical success in relation to the pooled rate[7,9,22,24-40].
Safety
The overall pooled rate of post procedural complications was 8.83% (95%CI:7.42-10.34).The forest plot depicting the pooled proportion of complications is in Figure 4.The pooled proportion of patients with bleeding as an adverse event following ETGBD was 1.03% (95%CI:0.58-1.62).Pooled proportion of patients with perforation as an adverse event following ETGBD was 0.78% (95%CI:0.39-1.29).Peritonitis/bile leak as an adverse event following ETGBD was calculated as a pooled proportion and was 0.45% (95%CI:0.17-0.87).The pooled proportion of patients with pancreatitis following ETGBD was 1.98% (95%CI:1.33-2.76).
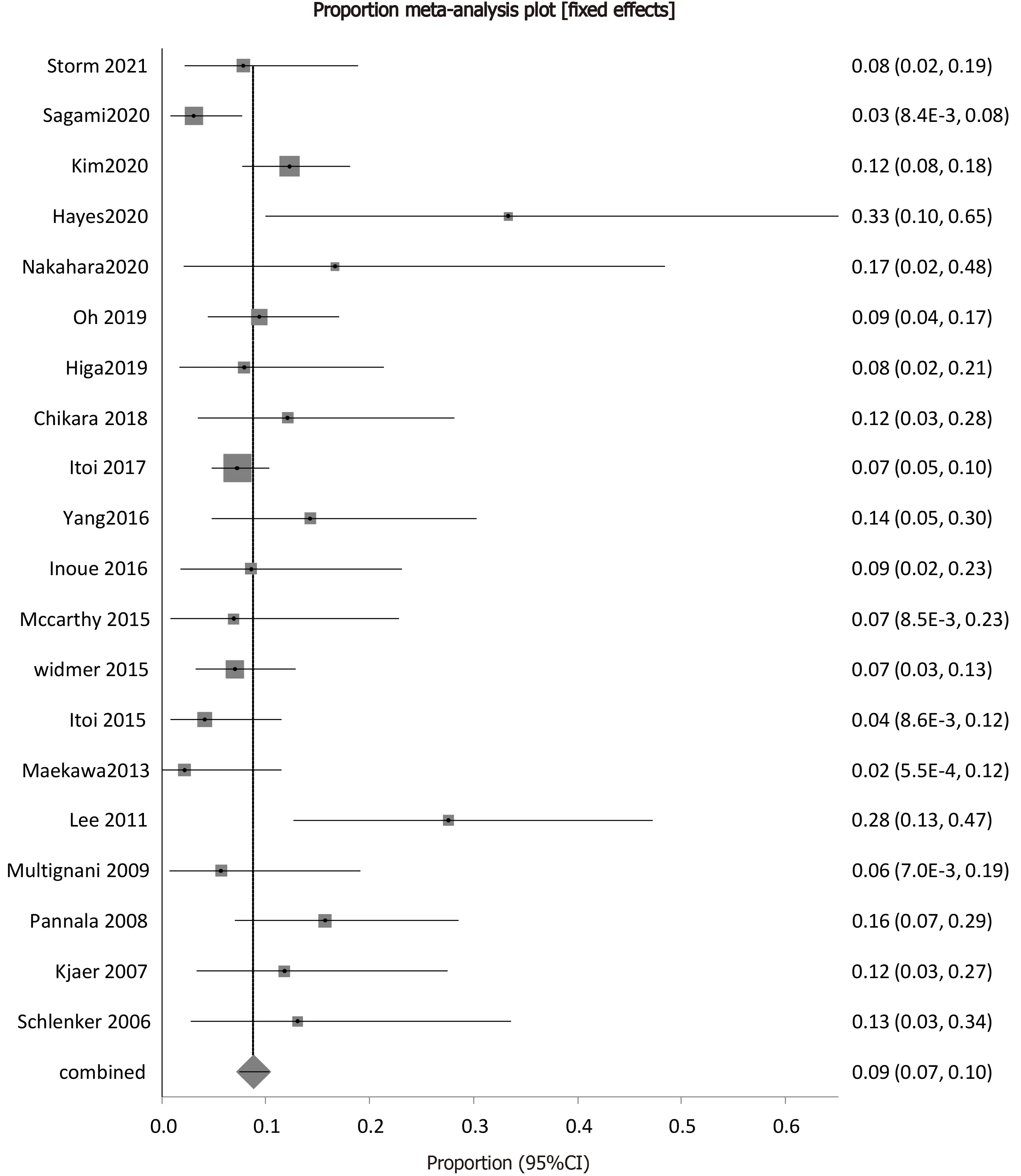
Figure 4 Forest plot showing the individual study proportions of endoscopic transpapillary gallbladder drainage related adverse events in relation to the pooled rate[7,9,22,24-39].
Stent related procedure complications were also featured in the analysis as adverse events in all the included studies.They included both stent occlusion and stent migration.The pooled proportion of patients with stent occlusion following ETGBD was 0.39% (95%CI:0.13-0.78).The pooled proportion of patients with stent migration was 1.3% (95%CI:0.75-1.99).
Recurrent cholecystitis was also included as a secondary outcome measure.There were 6 studies which reported a recurrence of cholecystitis following ETGBD.The pooled proportion of patients with recurrent cholecystitis following ETGBD was 1.48%(95%CI:0.92-2.16).
Publication bias calculation using the Harbord-Egger bias indicator gave a value of-1.61 (95%CI:-4.70-1.49) (P=0.29),indicating that there was no publication bias.The funnel plot in Figure 5 shows no publication bias for ETGBD clinical success.
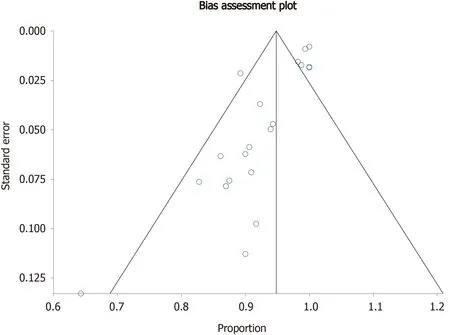
Figure 5 Funnel plot evaluating the effect of publication bias on individual studies rates of endoscopic transpapillary gallbladder drainage success.
DISCUSSION
Cholecystectomy is the standard of care for the treatment of acute cholecystitis,however a subset of patients exists with co-morbidities or poor clinical status that are not candidates for surgery.Based on Tokyo guidelines from 2018,the standard nonsurgical approach recommendation for high-risk patients has been percutaneous guided gallbladder drainage[19].It has remained the most frequently used intervention for inoperable patients due to the vast procedural expertise that exists as well as its significant representation within the literature.The management of cholecystitis has evolved to include endoscopic methods of treatment,and choosing the appropriate intervention requires consideration of multiple factors including patient co-morbidities and preferences,technical factors,and local expertise.Endoscopic therapies have been advantageous over percutaneous drainage when tolerability of externalized drainage is an issue due to patient discomfort and given the potential for these drains to migrate,occlude or become secondarily infected.Other patient factors such as ascites or coagulopathy also need to be considered.Technical factors such as suspected biliary obstruction due to choledocholithiasis and biliary stricture,also support the preferential use of transpapillary gallbladder drainage.
Transpapillary drainage can be technically challenging,specifically due to the difficult nature of cannulation of the bile duct and traversal of the cystic duct.Our pooled rates of technical and clinical success were 83% and 95% respectively.Rates of initial failure are not negligible,however if successfully performed the vast majority of patients found clinical success.Studies have shown that centers with high volume and expertise have benefited from their increased experience,with improved technical success rates.Kjaeret al[20] demonstrated an improvement in technical success from 50% in the first 4 years of the study to 89% in the final 5 years of the study,indicating that there is a learning curve that could be overcome with experience.Prior studies have demonstrated similar results when evaluating efficacy of endoscopic drainage in regards to technical and clinical success compared to percutaneous methods[21],though further comparison trials are required.
Lyuet al[23] demonstrated that the adverse event and mortality rates amongst EUS guided gallbladder drainage,transpapillary gallbladder drainage and percutaneous gallbladder drainage were comparable.Nonetheless,post-operative complications related to endoscopic interventions such as EUSGBD and ETGBD tended to have higher risk adverse events that had a higher propensity to lead to death,such as perforation,bleeding,and pancreatitis.Our overall pooled complication rate was about 9%,with the highest being pooled rates of pancreatitis.ERCP related complications have been an increased concern,given the need for cannulation of the bile duct for successful transpapillary gallbladder drainage and stenting to occur.Given the burden of potentially severe adverse events,ETGBD should be reserved for patients who are otherwise not candidates for standard percutaneous drainage.Such therapies should also be performed in centers with high expertise and specifically when other biliary interventions are called for,such as in the case of concomitant choledocholithiasis.
Based on our results,recurrent cholecystitis occurred in about 1% of patients undergoing transpapillary drainage and stenting.These patients with recurrence may require repeat transpapillary drainage,or other methods of gallbladder drainage.A subset of patients can eventually undergo definitive cholecystectomy when clinically stabilized.A particular benefit of ETGBD over other endoscopic interventions such as EUS guided stenting is the avoidance of creating a chole-duodenal or gastric fistula,which can make eventual surgical intervention difficult.Stents placed during ETGBD may be removed just prior to planned cholecystectomy.
Our study had several limitations.Most of the studies included were retrospective analysis,with only one randomized controlled trial.This could have led to selection and time bias.The exclusion of non-English studies could have also led to bias.Inclusion of these studies could have led to more randomized control trials in our analysis.Many of the studies included in the pooled analysis,included the use of nasobiliary drainage.Over the past several years,this method that has been utilized less frequently,in favor of double pigtail stents making the application of our data to everyday practice more difficult.Though based on prior subgroup analysis,double pigtail stenting was compared to nasobiliary drainage with similar rates of technical(85%vs81%),and clinical success (95%vs93%)[21].Outcome definitions,including technical success and clinical success varied among the included studies.This may have confounded the pooled results,though publication bias was not significant based on indicators that were used.
CONCLUSION
In conclusion,our study supports that ETGBD is a safe and efficacious procedure for inoperable patients with cholecystitis.Given its relative technical difficulty,which is inherent to ERCP,it should be performed in high volume centers and when patients are unfit for percutaneous drainage.Its clinical success rates were comparable to prior analyses,and rates of adverse events were acceptable.At this time further data and prospective trials would be beneficial in evaluating the long-term outcomes of ETGBD.
ARTICLE HIGHLIGHTS
Research background
Percutaneous gallbladder drainage has been the standard treatment of acute cholecystitis in patients who are not surgical candidates.Our study sought to evaluate the efficacy and safety of transpapillary drainage for acute cholecystitis in this subset of patients.
Research motivation
The key topics of interest include non-surgical,less-invasive techniques to treat acute cholecystitis.The evolution of safe and effective treatments in acute cholecystitis can lead to improved patient outcomes and quality of life following treatment.Future research can also have a positive effect on cost effectiveness and health care utilization.
Research objectives
The main objectives were to evaluate feasibility,efficacy and safety of transpapillary gallbladder drainage in inoperable patients for the treatment of acute cholecystitis.This can positively affect further research and direct comparison trials.
Research methods
A systematic review was performed followed by updated meta-analysis.
Research results
The pooled technical success rate of endoscopic transpapillary gallbladder drainage(ETGBD) was 82.62% [95% confidence interval (CI):80.63-84.52].The pooled clinical success rate was found to be 94.87% (95%CI:93.54-96.05).The pooled overall complication rate was 8.83% (95%CI:7.42-10.34).Pooled rates of post procedure adverse events were bleeding 1.03% (95%CI:0.58-1.62),perforation 0.78% (95%CI:0.39-1.29),peritonitis/bile leak 0.45% (95%CI:0.17-0.87),and pancreatitis 1.98% (95%CI:1.33-2.76).The pooled rates of stent occlusion and migration were 0.39% (95%CI:0.13-0.78) and 1.3% (95%CI:0.75-1.99) respectively.The pooled rate of cholecystitis recurrence following ETGBD was 1.48% (95%CI:0.92-2.16).
Research conclusions
Our results demonstrated that transpapillary gallbladder drainage for treatment of acute cholecystitis is both an efficacious and safe procedure in patients that are inoperable.This particular method of gallbladder drainage may offer an alternative to a certain subset of inoperable patients who are otherwise not candidates for percutaneous drainage.Patients who demonstrate signs of concomitant choledocholithiasis or cholangitis also benefit.Comparison between percutaneous drainage,and endoscopic drainage methods with endoscopic ultrasound or a transpapillary approach has been explored however results remain inconclusive.
Research perspectives
Future research should involve randomized controlled trials to compare the different non-surgical techniques used in treatment of acute cholecystitis.In regards to ETGBD,emphasis should be placed on different stenting methods,along with assessment of long term outcomes.
 World Journal of Gastrointestinal Endoscopy2021年8期
World Journal of Gastrointestinal Endoscopy2021年8期
- World Journal of Gastrointestinal Endoscopy的其它文章
- Endo-hepatology:An emerging field
- Prospective evaluation of the hemorrhoid energy treatment for the management of bleeding internal hemorrhoids
- Effect of pancreatic endotherapy on quality of life in chronic pancreatitis patients:A systematic review
- Thoracoscopic esophagectomy is related to better outcomes in early adenocarcinoma of esophagogastric junction tumors
- Endoscopic ultrasound-guided biliary drainage:Are we there yet?
- Indications and outcomes of endoscopic resection for nonpedunculated colorectal lesions:A narrative review
