Submucosal hematoma with a wide range of lesions, severe condition and atypical clinical symptoms: A case report
Liang Liu, Xing-Jie Shen, Li-Jun Xue, Shu-Kun Yao, Jing-Yu Zhu
Liang Liu, Xing-Jie Shen, Li-Jun Xue, Jing-Yu Zhu, Department of Gastroenterology, Central Hospital Affiliated to Shandong First Medical University, Jinan 250011, Shandong Province,China
Liang Liu, Xing-Jie Shen, Li-Jun Xue, Jing-Yu Zhu, Department of Gastroenterology, Jinan Central Hospital, Cheeloo College of Medicine, Shandong University, Jinan 250011, Shandong Province, China
Shu-Kun Yao, Department of Gastroenterology, China-Japan Friendship Hospital, Beijing 100029, China
Abstract BACKGROUND Submucosal hematoma (SH) is one of the rare causes of upper gastrointestinal bleeding. As a rare and critical disease in clinical practice, it should be paid more attention to by clinicians to avoid missed diagnosis and misdiagnosis. Most of the esophageal submucosal hematomas have clear causes, including retrosternal pain,dysphagia, etc. Here, we report a rare case of SH extending from the hypopharynx to the lower esophagus caused by oral administration of hirudin and panax notoginseng powder, with atypical clinical manifestation. Such a long submucosal hematoma has rarely been reported.CASE SUMMARY The patient was a 60-year-old male with a history of gastritis, hypertension,coronary heart disease, and coronary stent implantation. The patient developed chest tiredness and heartburn after taking 10 capsules of a homemade mixture of hirudin and notoginseng powder in the previous 2 d. He did not have hematemesis or black stool. Gastroscopy and chest computed tomography confirmed the diagnosis of SH, which ranged from the pharynx to the lower esophagus and was 35-40 cm in length. After the diagnosis was confirmed, we performed active conservative treatment on the patient, and the patient recovered well and remained asymptomatic during the 26-mo follow-up.CONCLUSION SH is rare, and cases with atypical clinical symptoms may lead to misdiagnosis and missed diagnosis. Ignorance of this disease can lead to serious clinical consequences. Conservative therapy is effective and the prognosis is good.
Key Words: Submucosal hematoma; Hypopharynx; lower esophagus; hirudin and panax notoginseng powder; Gastroscopy; Computed tomography; Case report
INTRODUCTION
Submucosal hematoma (SH) of the digestive tract is an uncommon clinical condition,which can occur spontaneously or be caused by trauma such as during endoscopic surgery[1,2]. Characteristic clinical manifestations of SH comprises dysphagia or odynophagia, acute chest pain, and hematemesis[3]. Typical cases of SH have been reported by several authors[1,2,4]. However, no cases of the SH extending from the hypopharynx to the lower esophagus caused by oral administration of hirudin and panax notoginseng powder have been reported, especially cases with atypical clinical manifestations. We here report such a rare case.
CASE PRESENTATION
Chief complaints
A 60-year-old man was admitted to the Emergency Department of our hospital with chest tightness and heartburn for 2 d.
History of present illness
The patient had taken 10 capsules (containing hirudin and panax notoginseng powder) 2 d prior before and subsequently developed chest tightness and heartburn.Capsules were prepared by the patient himself. It is considered that the oral dose of the capsule was too large. The patient had a short period of shock, and we considered hemorrhagic shock.
History of past illness
The patient had a history of gastritis, hypertension, and coronary heart disease for more than 5 years. The patient's blood pressure was well controlled with oral antihypertensive drugs. Coronary artery stent implantation was performed for coronary heart disease 2 years ago. After coronary stenting, the patient selfadministered aspirin and plavix for a relatively short period of time. He is not currently taking any antiplatelet drugs.
Personal and family history
He denies any personal and family history.
Physical examination
Physical examination showed tenderness in subxiphoid, blood pressure of 80/42 mmHg (normal range: 90-140/60-90 mmHg), pulse rate of 122/min (normal range: 60-90/min), and respiratory rate of 22/min (normal range: 16-20/min). The patient had two episodes of transient loss of consciousness.
Laboratory examinations
Blood tests revealed abnormal results: A red blood cell count of 1.3 × 1012/L (4.3-5.8 ×1012/L), a platelet count of 12 × 109/L (125-360 × 109/L), a hemoglobin count of 42 g/L(130-175 g/L), and a D-dimer count of 1.65 mg/L (0-0.55 mg/L).
Imaging examinations
Chest computed tomography (CT) revealed marked narrowing of the entire esophageal lumen(Figure 1).Emergency endoscopy found a large SH extending from the hypopharynx to the lower esophagus. The lesion was a coarse mucosal protuberant lesion parallel to the longitudinal axis of the esophagus, with a length of 35-40 cm (Figure 2A and B).

Figure 1 Marked narrowing of the entire esophageal lumen under computed tomography examination.
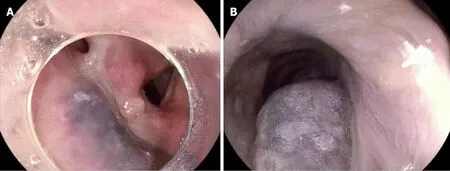
Figure 2 Endoscopic examination results of the patient. A large submucosal hematoma extending from hypopharynx to lower esophagus under emergency endoscopy. A: Submucosal hematoma of hypopharynx; B: Submucosal hematoma of lower esophagus.
FINAL DIAGNOSIS
We considered the patient to be in hemorrhagic shock. Due to excessive blood loss and reduced effective circulating blood volume, the shock type was hypovolemic shock.Based on the CT and emergency endoscopy findings, the final diagnosis was SH extending from the hypopharynx to the lower esophagus.
TREATMENT
The patient was successfully managed with conservative therapy. During the period,the patient was given intravenous fluid infusion, intermittent infusion of red blood cells and fibrinogen, intravenous infusion of esomeprazole, oral thrombin, and general conservative treatments.
OUTCOME AND FOLLOW-UP
By timely fluid replacement, component blood transfusion, the patient soon regained consciousness, the condition did not continue to deteriorate. After 15 d, the gastroscopy showed the absorption of the submucosal hematoma of the esophagus(Figure 3). The patient's general condition improved well. The patient remained asymptomatic during a 26-mo follow-up.

Figure 3 Gastroscopy reexamination showed absorption of the hematoma 15 d later.
DISCUSSION
SH of digestive tract is rare, and it primarily occurs in the esophagus or duodenum[5].In the present case, SH was found extending from the hypopharynx to the lower esophagus. The patient had no bleeding of the skin and mucosa. To the best of our knowledge, no such cases had been reported in the literature. The patient was informed from someone else that hirudin and notoginseng powder have the therapeutic effect of promoting blood circulation and removing blood stasis, so he took 10 self-made capsules containing hirudin and panax notoginseng powder 2 d prior,which is a unique feature of this case. The hirudin is a direct inhibitor of thrombin and it can affect blood coagulation and promote fibrinolysis in many ways[6]. In addition,the hirudin has a strong efficacy in anti-thrombus and inhibition of platelet aggregation[6]. The effective component of panax notoginseng is the total saponin of panax notoginseng, which can shorten bleeding and clotting time[7]. It also has a pharmacodynamics effect in anti-platelet aggregation and thrombolysis[8]. In this case,the patient had a history of hypertension, coronary heart disease, and coronary stent implantation, we therefore speculate that pathophysiological changes may have occurred in the blood vessels of in many organs of the body. These potential changes together with the use of capsules containing hirudin and panax notoginseng powder eventually resulted in SH. After oral administration of the mixture of hirudin and panax notoginseng capsule, blood coagulation function in the body was impaired, as lowering platelets aggravates tendency of bleeding. At the same time, hirudin can directly act on the body cavity mucosa. According to the CT findings, we initially diagnosed a SH in this patient. The patient had a short period of shock, and we considered hemorrhagic shock. By timely fluid replacement, component blood transfusion, the patient soon regained consciousness, and the condition did not continue to deteriorate. Gastroscopy is the gold standard for defining SH. The patient was in a compositional transfusion, his shock had improved and he was conscious, so we did an emergency gastroscope. Emergency endoscopy confirmed the diagnosis of a SH. The patient's condition improved after 6 d in the intensive care unit, and he was transferred to the general digestive ward for 9 d of conservative treatments.
Clinical manifestations of the patient were not typical, and it was difficult to make a correct diagnosis quickly. The patient's bleeding was in the submucosa and did not enter the gastrointestinal tract, so there was no evidence of hematemesis or bloody stool. Chief complaints of the patient were chest tightness and heartburn, which need to be distinguished from ischemic heart disease, pulmonary embolism, and reflux esophagitis. In this case, the absence of significant abnormalities in troponin T and electrocardiogram results can rule out myocardial infarction. Detailed and accurate acquisition of clinical data of patients, comprehensive physical examination combined with endoscopy, and CT are useful for accurate diagnosis. Risk factors for SH include female sex, hypertension, increased esophageal pressure, coagulopathy, and use of an anticoagulant[2,4]. It has been reported that elderly patients who are taking anticoagulant or antiplatelet medication are at higher risk for SH[4]. This case report has confirmed these findings. The esophageal submucosal hematoma was one of the rare causes of upper gastrointestinal bleeding. As a rare and critical disease in clinic, it should be paid more attention to by the clinicians, especially the doctors in the emergency department, in order to avoid misdiagnosis. The necessary condition for the onset of this disease is the sudden increase of pressure in the esophageal lumen,most of which have clear causes. Esophageal submucosal hematoma generally does not involve the muscular layer, so the treatment is mainly conservative medical treatment. Treatment methods include water fasting, acid suppression, hemostasis,esophagus and gastric mucosa protection, and symptomatic supportive treatment.Hematoma usually absorbs itself within 2 to 3 wk and has a good prognosis.
CONCLUSION
SH of digestive tract is an uncommon condition. Our case shows that the SH extending from the hypopharynx to the lower esophagus can occur due to ingestion of hirudin and panax notoginseng powder. Conservative therapy is effective, and prognosis is excellent. Clinical symptoms of atypical cases can mimic cardiothoracic emergencies,and ignorance of the disease may cause serious clinical consequences. Physicians should be aware of this rare condition even when clinical symptoms are atypical.
 World Journal of Clinical Cases2021年20期
World Journal of Clinical Cases2021年20期
- World Journal of Clinical Cases的其它文章
- Obesity in people with diabetes in COVID-19 times: Important considerations and precautions to be taken
- Revisiting delayed appendectomy in patients with acute appendicitis
- Detection of short stature homeobox 2 and RAS-associated domain family 1 subtype A DNA methylation in interventional pulmonology
- Borderline resectable pancreatic cancer and vascular resections in the era of neoadjuvant therapy
- Esophageal manifestation in patients with scleroderma
- Exploration of transmission chain and prevention of the recurrence of coronavirus disease 2019 in Heilongjiang Province due to inhospital transmission
