Low-dose clozapine-related seizure: A case report and literature review
Dan-Sheng Le, Heng Su, Zheng-Luan Liao, En-Yan Yu
Dan-Sheng Le, The Second Clinical Medical College, Zhejiang Chinese Medicine University,Hangzhou 310051, Zhejiang Province, China
Heng Su, Zheng-Luan Liao, Department of Psychiatry, Zhejiang Provincial People’s Hospital,Hangzhou 310000, Zhejiang Province, China
En-Yan Yu, Department of Psychiatry, The Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital), Institute of Basic Medicine and Cancer,Chinese Academy of Sciences, Hangzhou 310022, Zhejiang Province, China
Abstract BACKGROUND Treatment-resistant schizophrenia is a severe form of schizophrenia characterized by poor response to at least two antipsychotic drugs and is typically treated with clozapine. However, clozapine lowers the epileptic threshold, leading to seizures,which are severe side effects of antipsychotics that result in multiple complications. Clozapine-related seizures are generally considered to be dose-dependent and especially rare in the low-dose (150-300 mg/d) clozapine treated population.Due to clinical rarity, little is known about its clinical characteristics and treatment.CASE SUMMARY A 62-year-old Chinese man with a 40-year history of treatment-resistant schizophrenia presented to the Emergency Department with symptoms of myoclonus,consciousness disturbance and vomiting after taking 125 mg clozapine. Upon admission, the patient had a suddenly generalized tonic-clonic seizure lasting for about half a minute with persistent disturbance of consciousness, fever, cough and bloody sputum, which was considered to be low-dose clozapine-related seizure. After antiepileptic and multiple anti-infection treatments, the patient was discharged without epileptic or psychotic symptoms.CONCLUSION Our aim is to highlight the early prevention and optimal treatment of clozapinerelated seizure through case analysis and literature review.
Key Words: Seizure; Treatment-resistant schizophrenia; Antipsychotic; Antiepileptic;Electroconvulsive therapy; Case report
INTRODUCTION
Clozapine, the first officially marketed atypical antipsychotic, has a unique therapeutic effect on treatment-resistant schizophrenia (TRS)[1] that significantly improves patients' quality of life, reduces violent and impulsive behavior[2] and reduces suicide and mortality rates[2-4]. Notably, the incidence of clozapine-related seizure is up to 4%-6%[5,6], which is higher than that of other typical or atypical antipsychotics[7] and will lead to further complications and ultimately increased mortality.
Clozapine-related seizures are generally considered to be dose-dependent and are rare in people treated with conventional doses of clozapine (300-450 mg/d), and especially rare in the low-dose (150-300 mg/d) clozapine treated population. Due to clinical rarity, little is known about its clinical characteristics and treatment. Thus, we herein report a 62-year-old Chinese male who had schizophrenia with low-dose clozapine-related seizure followed by aspiration pneumonia. Previous clinical cases of clozapine-related seizure were identified in a database and carefully reviewed to identify the clinical features, treatment options and factors that may contribute to the development of this rare disease entity.
CASE PRESENTATION
Chief complaints
A 62-year-old Chinese male presented to the Emergency Department of our hospital with complaints of myoclonus, consciousness disturbance and vomiting for 1 h.
History of present illness
In the absence of a caregiver, the patient was found lying unconscious with myoclonic movements, surrounded by vomit. The number of remaining tablets suggested 125 mg clozapine had been taken.
History of past illness
According to medical history, the patient has had TRS for 40 years, presenting with hallucinations, delusions, splitting of thought and a weak response to olanzapine,risperidone and perphenazine. The patient has been regularly taking clozapine 62.5 mg/d and quetiapine 300 mg/d for the last 10 years, and the mental symptoms were well controlled.
Personal and family history
The patient has been regularly taking clozapine 62.5 mg/d and quetiapine 300 mg/d for the last 10 years, and the mental symptoms were well controlled. No family history of mental illness was reported.
Physical examination
Upon admission, the patient had a generalized tonic-clonic seizure (GTCS) lasting for about half a minute with persistent consciousness disturbance, fever, cough and bloody sputum.
Laboratory examinations
Emergency laboratory tests revealed a white cell count of 10.11 × 109/L, 89.3% of which were neutrophils, and a high-sensitivity C-reactive protein content of 4.8 mg/L;the sputum culture indicated the presence of gram-negative bacilli. The blood concentration of clozapine was higher than 1500 ng/mL (reference: 350-600 ng/mL) at the 24thh and the 48thh after last administration. No other obvious abnormalities were found upon cerebrospinal fluid examination.
On the 10thday of hospitalization, the blood concentration of clozapine was 153 ng/mL (reference = 350-600 ng/mL).
Imaging examinations
Emergency chest computed tomography indicated bilateral pneumonia with bilateral pleural effusion (Figure 1), and no other obvious abnormalities were found upon cranial computed tomography.
On the 3rdday of hospitalization, electroencephalogram (EEG) showed slow-wave and no epileptiform discharges (Figure 2).
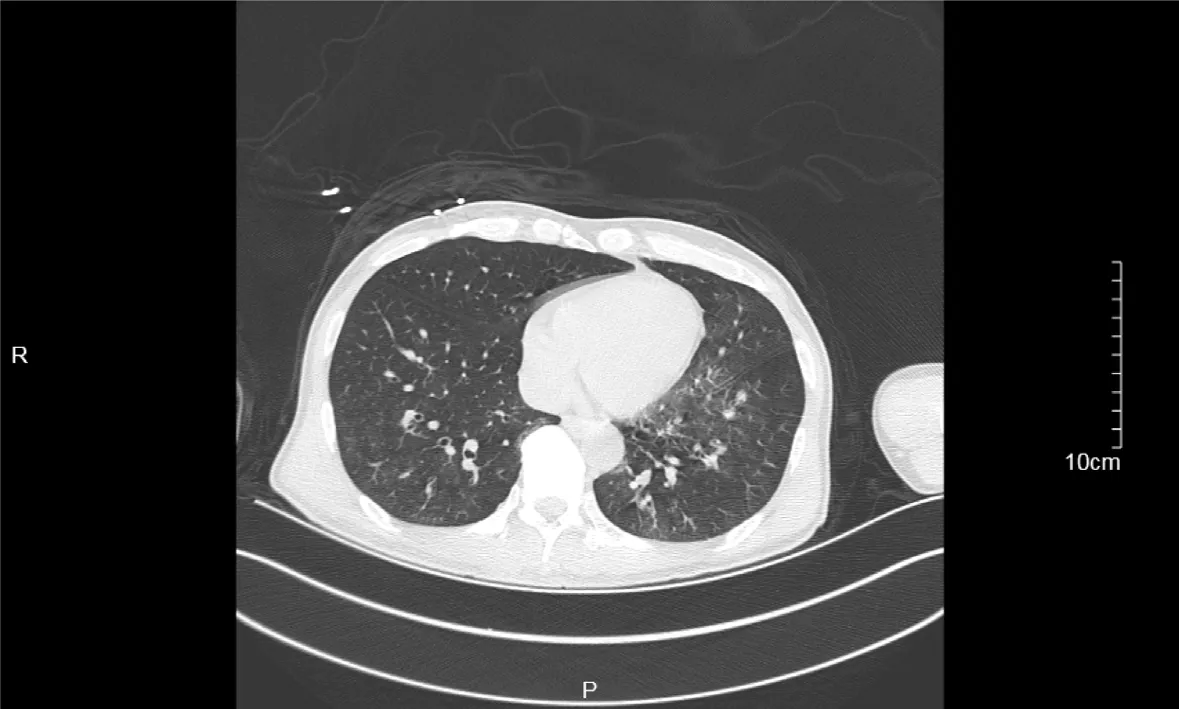
Figure 1 Emergency chest computed tomography. Emergency chest computed tomography indicated bilateral pneumonia with bilateral pleural effusion.

Figure 2 Electroencephalogram on the 3rd day. Electroencephalogram showed slow-wave and no epileptiform discharges.
FINAL DIAGNOSIS
Schizophrenia with low-dose clozapine-related seizure followed by aspiration pneumonia.
TREATMENT
Treatment mainly included antiepileptic therapy, multiple anti-infection therapies,and psychotolytic therapy under the premise of the patency of airway.
After admission, clozapine was discontinued immediately, and sodium valproate 1000 mg/d, diazepam 2.5 mg/d, quetiapine 300 mg/d, acyclovir 500 mg/d and cefoperazone 2000 mg/d were administrated.
On the 5thday of hospitalization, the patient developed dyspnea with an oxygen saturation of 60%-70% and no significant improvement after sputum aspiration, which was considered as respiratory failure. Thus, immediate tracheal intubation and mechanical ventilatory support were performed, and the treatment regimens were adjusted as meropenem 2000 mg/d, capophenine 50 mg/d and levetiracetam 1000 mg/d in addition to atomization, phlegm reduction and enteral nutrition.
On the 11thday of hospitalization, psychotic symptoms were observed after extubation, hallucinations, and splitting of thought. Therefore, clozapine 25 mg/d(slowly increased to 62.5 mg over 2 wk) and quetiapine 300 mg/d were administered.
OUTCOME AND FOLLOW-UP
Eventually, the patient was discharged with no obvious seizures or psychotic symptoms and was satisfied with his treatment. After discharge, the patient took clozapine 62.5 mg/d and quetiapine 300 mg/d regularly under the supervision of a caregiver. During 3 mo of follow-up, the patient recovered well, and no exacerbations were detected.
DISCUSSION
Schizophrenia is a debilitating and heterogeneous mental disorder characterized by discordance between mental activity and the environment and manifests as a complex blend of positive and negative symptoms and cognitive impairment[8,9]. The lifetime suicide risk of patients with schizophrenia is 2 to 3 times higher than that in the general population[10], estimated to be about 5%[11], and life expectancy is about 20%less than that of the general population[12]. TRS, which is characterized by poor response to at least two antipsychotic drugs, is a severe form of schizophrenia that accounts for approximately one-third of all schizophrenia cases[13].
Clozapine not only has better effects on positive and negative symptoms and cognitive impairment than typical antipsychotics but also is associated with fewer adverse reactions[1,2]. Moreover, clozapine has unique therapeutic effects against TRS[1] that can significantly improve patients’ quality of life, reduce violence and impulsive behaviors[2] and decrease the suicide rate and mortality[2-4]. However, the incidence of clozapine-related seizure is 4%-6%[5,6], which is higher than that of seizures related to typical antipsychotics[7]. Moreover, the uncertainty and unpredictability of epileptic seizures are closely related to negative emotions[14], which may result in the generation, maintenance or exacerbation of mental disorders[15].
In this case, EEG examinations were not performed in a timely manner, and no significant abnormalities were found in subsequent EEG reports. No psychometric scale results were reported, and the evaluation of therapeutic efficacy for schizo-phrenia was based primarily on clinical presentation. This case does not prove a link between low-dose clozapine, seizure and pneumonia nor does it reflect the wider population. Therefore, a review of the previous literature and a summary of the published case reports is necessary.
The mechanism of clozapine-related seizure may be caused by the combined action of multiple receptors. Dopamine has been shown to reduce the excitability of the primary sensorimotor cortex in adult rats[16]. Clozapine may increase cortical excitability by reducing dopamine neurotransmission[16].Serotonin receptors are expressed in almost all neural networks associated with seizure. Consumption of serotonin in the brain can enhance the excitability of neurons, reduce the seizure threshold and increase seizure frequency[17]. The antiepileptic effects of selective serotonin reuptake inhibitors have been demonstrated in controlled trials[18].
Clozapine-related seizure is widely considered as dose-dependent[6]. Standard titration of clozapine refers to starting at a dosage of 12.5-25 mg/d and increasing the dosage by 25-50 mg/d to reach a maintenance dosage of 300-400 mg/d after 2 wk[19].This slow titration method can reduce the risk of seizure, but it may extend the treatment time or require the combination of clozapine with other drugs to control mental symptoms over time[19,20]. In contrast, the rapid increase regimen can quickly control psychiatric symptoms and reduce medical costs[19,21] but may lead to unnecessarily high drug doses that cause adverse drug reactions such as seizure.However, in some clinical trials, the rapid titration of clozapine was reported to be safe and effective and to be beneficial for aggressive or suicidal patients[19,22].
The dosage regimen of clozapine directly affects blood concentration. A study showed that the risk of seizure is 3% when the dose of clozapine does not exceed 300 mg/d, that the risk increases to 8% when the dose is 325 to 500 mg/d and that the risk is as high as 38% when the dose exceeds 500 mg/d[6]. The lower limit of the therapeutic range for clozapine serum levels is between 250 and 420 ng/mL, and the risk of seizure increases when the serum level is > 750 ng/mL[23] and increases significantly when the serum level exceeds 1300 ng/mL[24]. Moreover, for every 100 mg/d increase in daily dose of clozapine, the abnormal rate of EEG increases by 8%,and for every 100 mg/L increase in plasma level of clozapine, the rate increases by 12%[25]. However, the serum level is affected by age[23], gender[26], smoking status[23], caffeine use[27] and other factors, hence, neither the serum level nor the dose of clozapine could accurately predict the occurrence of seizure. In clinical practice, most practitioners take 600 mg/d as the safety threshold[5], but cases of clozapine-related seizure have also been reported in the low-dose (150-300 mg/d)[28] treatment group[29,30]. Literature was systematically retrieved from electronic databases (PubMed andWeb of Science) to review cases of clozapine-related seizure published between 2000 and 2019. A total of 18 studies were included (Table 1)[6,29-35], eight of which reported 14 cases of low-dose clozapine-related seizure.
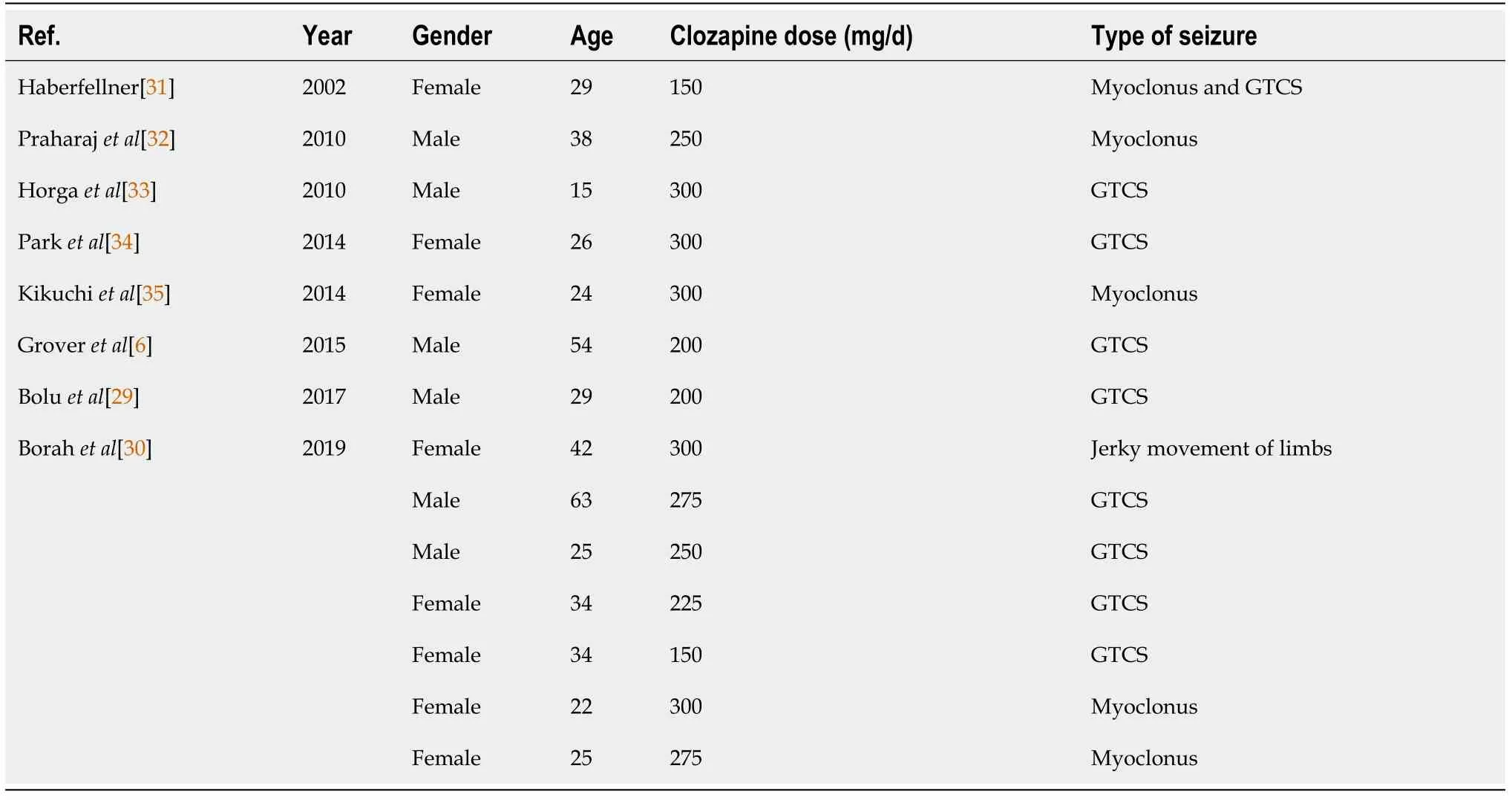
Table 1 Case reports of low-dose clozapine-related seizure
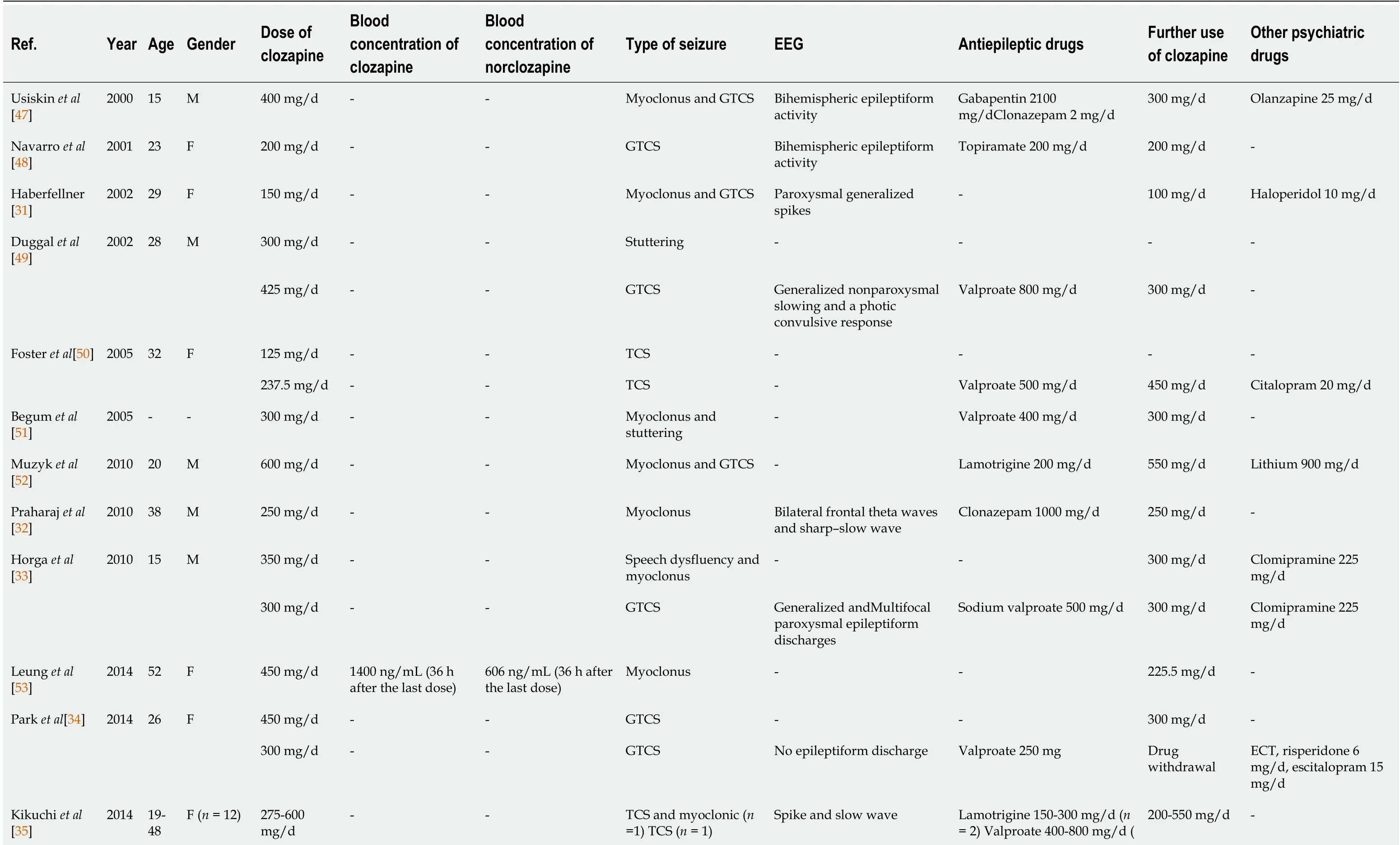
Table 2 Case reports of clozapine-related seizure published in last 20 years
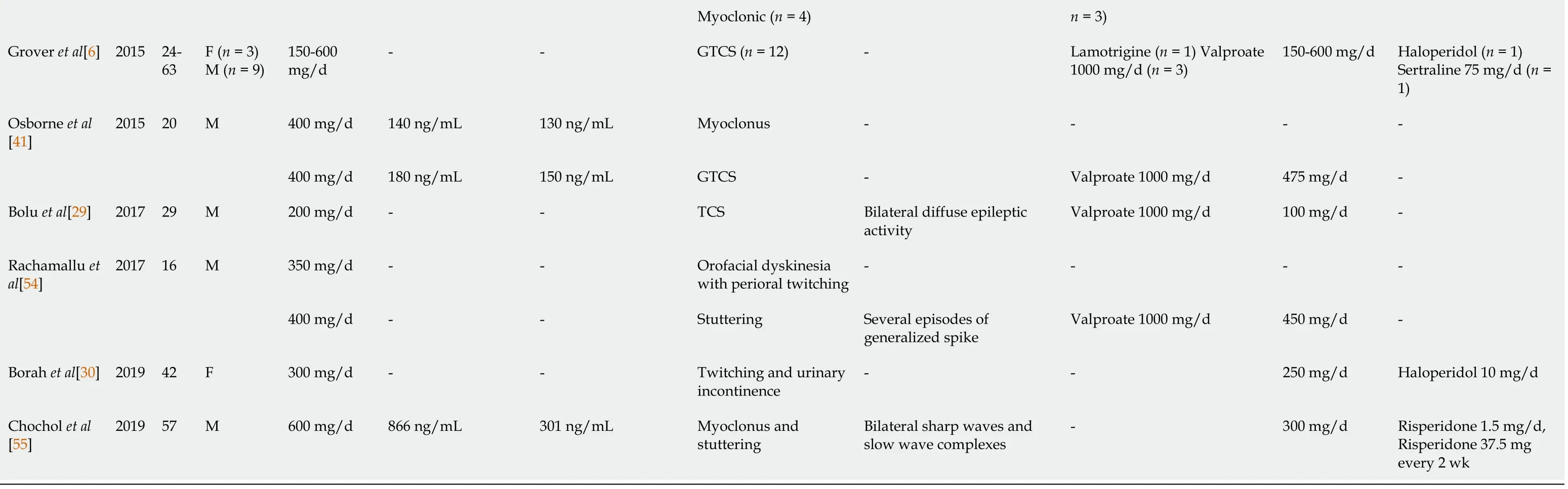
EEG: Electroencephalogram; M: Male; F: Female; GTCS: Generalized tonic-clonic seizure; TCS: Tonic-clonic seizure; ECT: Electroconvulsive therapy.
Antiepileptic drugs (AEDs) are widely used in the treatment of clozapine-related seizures. Some authors believe that the dose of clozapine should be reduced by 40%-50% when a seizure occurs for the first time and that AEDs should not be started until the second seizure is observed[36]. In clinical cases, dose reduction may lead to recurrence of psychiatric symptoms[37]. There are also studies suggesting that the continued use of clozapine is beneficial for patients and that AEDs starting at a dosage of 500 mg/d should be used[5]. However, the use of AEDs such as lamotrigine[38],levetiracetam[38] and topiramate[39] may increase the risk of mental illness through increasing central dopamine activity[40], and drug interactions may lead to other adverse reactions[24]. Thus, AEDs are not recommended as the main preventive agents before the occurrence of clozapine-related seizure[24].
Valproate, a broad-spectrum AED, is currently widely regarded as the first choice for the treatment of clozapine-related seizure and has a significant therapeutic effect on GTCS[5] and myoclonus[33,41]. Valproate is especially suitable for patients with affective disorders because of its emotional stabilization and antimania effects[42].Interestingly, valproic acid can reduce clozapine plasma concentrations[5,25,41],allowing patients to continue to use it safely. It also allows clozapine-treated patients to remain seizure-free.
Electroconvulsive therapy involves stimulation of the brain through electric currents and has been reported to increase the levels of dopamine and its metabolites[43].Electroconvulsive therapy has been regarded as an effective treatment[44] for mental illness since the 1930s, and it can effectively reduce the frequency of seizures in patients that show insufficient responses to AEDs[45]. In addition, intracranial electroencephalographic monitoring has been found to have important clinical value in human experimental reports, and it may be used in the monitoring of drug-related seizures in the future[46]. Monitoring still has some potential safety risks that need to be further studied and reduced[46].
CONCLUSION
This case demonstrates the clinical presentation of and effective treatments for lowdose clozapine-related seizure followed by aspiration pneumonia. We reviewed the associated literature to identify the influencing factors and summarized the research progress of clozapine-related seizure to potential provide ideas for early clinical prevention and treatment (Table 2)[6,29-35,41,47-55]. Given the limited nature of case reports and the urgent clinical need, this field should be taken seriously and further studied.
 World Journal of Clinical Cases2021年20期
World Journal of Clinical Cases2021年20期
- World Journal of Clinical Cases的其它文章
- Obesity in people with diabetes in COVID-19 times: Important considerations and precautions to be taken
- Revisiting delayed appendectomy in patients with acute appendicitis
- Detection of short stature homeobox 2 and RAS-associated domain family 1 subtype A DNA methylation in interventional pulmonology
- Borderline resectable pancreatic cancer and vascular resections in the era of neoadjuvant therapy
- Esophageal manifestation in patients with scleroderma
- Exploration of transmission chain and prevention of the recurrence of coronavirus disease 2019 in Heilongjiang Province due to inhospital transmission
