Urethral Orifice Genital Herpes Caused by HSV-1 in a Female Patient:A Case Report
Jia-Yi Yang,Xiao-Hui Mo,Xiu-Li Wang,*
1Institute of Photomedicine,Shanghai Skin Disease Hospital,Tongji University School of Medicine,Shanghai 200443,China,
2Central Laboratory,Shanghai Skin Disease Hospital,Tongji University School of Medicine,Shanghai 200443,China.
Abstract Introduction:Genital herpes is one of the most common sexually transmitted infections worldwide.Most genital herpes occur on the genitalia,perineum,buttocks,upper thighs,or perianal areas.However,there were reports of rare cases of genital herpes on urethral orifice.
Keywords:Genital herpes,urethral orifice,herpes simplex virus
Introduction
Genital herpes is one of the most common sexually transmitted infections,affecting more than 400 million persons worldwide.It is caused by herpes simplex virus type 1 or 2(HSV-1 or HSV-2,respectively).1HSV-1 is the predominant cause of orolabial herpes.Genital herpes is more likely to be caused by HSV-2.However,HSV-1 is now detected more often in the genitalia,mainly in European countries,North America,and Canada.1-2
Visible genital herpes consists of single or clustered vesicles on the genitalia,perineum,buttocks,upper thighs,or perianal areas that ulcerate before resolving.This report describes the diagnosis of genital herpes of the urethral orifice in a woman who was HSV-1 DNA-positive and HSV-2 DNA-negative.
Case report
A 53-year-old woman complained with a 1-month history of vaginal pruritus.Her medical history was unremarkable.By examination,a heavy and cottage cheese-like vaginal discharge was seen,and the bilateral labia majora were thickened.The vaginal discharge was tested for Chlamydia,Neisseria,and Mycoplasma species,all of which were negative;however,a fungal culture was positive.Thus,monilial vaginitis was considered,and nystatin and bifonazole were prescribed.Two weeks later,the patient returned with new onset of a burning sensation around the urethra.Her pruritus,however,had subsided.On examination,a clustered punctate erosion was seen on the right labium majus with a small amount of vaginal discharge.Serological testing was positive for HSV-1 immunoglobulin(Ig)G and HSV-2 IgG,and negative for HSV-1 Ig M,HSV-2 Ig M,and human immunodeficiency virus.A Treponema pallidum particle agglutination test and rapid plasma regain test were also negative.Hence,genital herpes was considered.

Figure 1.Clinical presentation of the patient with Urethral Orifice Genital Herpes Caused by HSV-1 before and after treatment.(A)Before treatment.Red arrow indicates the erosion on mucosa of urethral orifice.(B)Smooth urethral orifice mucosa post treatment.
In light of this diagnosis,the patient was treated with acyclovir for 14 days at a dosage of 0.2g three times daily.However,1 month later,the patient complained of urgent urination with dysuria.She had no fever,but a urinalysis showed strong positivity for leukocytes.She was diagnosed with a secondary urinary tract infection and was administered levofloxacin.The patient’s sexual partner was advised to undergo testing for HSV-1 or HSV-2.
Approximately 1.5 months later,the patient returned to the outpatient clinic with little improvement in the dysuria but with absence of frequent micturition,vaginal pruritus,and fever.Examination revealed erosion of the urethral orifice mucosa with marked tenderness(Fig.1A).Urinalysis was positive for leukocytes and concealed blood.Viral swabs of the urethral orifice were positive for HSV-1 DNA and negative for HSV-2 DNA by PCR(Fig.2).
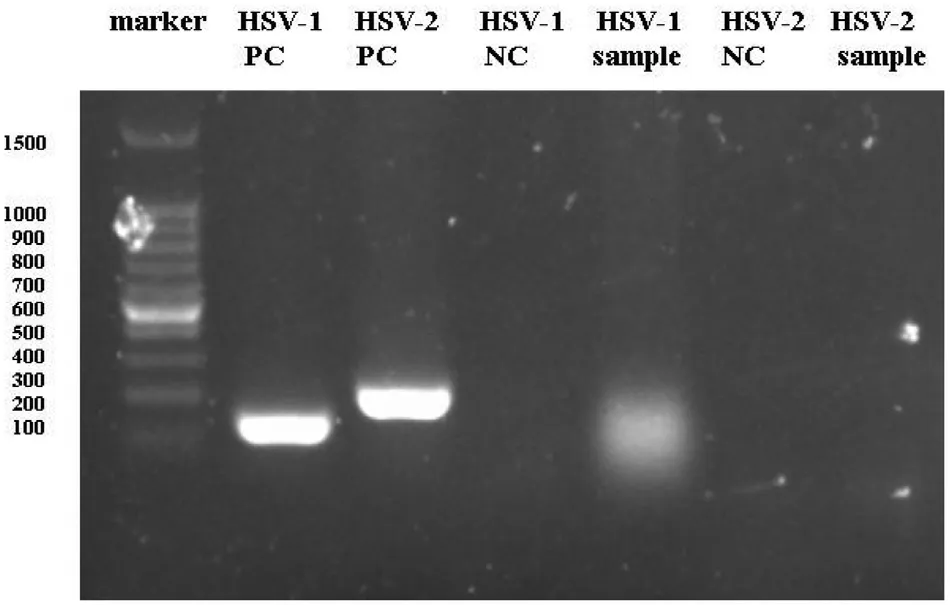
Figure 2.PCR results show HSV-1 DNA positive and HSV-2 DNA negative.HSV-1:herpes simplex virus type 1;HSV-2:herpes simplex virus type 2;NC:normal control;PC:positive control.
The final diagnosis was genital herpes of the urethral orifice,and the patient was treated with acyclovir.She was followed up 2 weeks later,and her clinical symptoms had significantly improved.The lesion had resolved and the urethral orifice mucosa was smooth(Fig.1B).The patient gave her agreement for the case publication.
Discussion
Genital herpes is common in Western countries,with a prevalence rate of approximately 13% to 25%.This infection is readily transmitted from one partner to another,possibly because of the atypical symptoms.1The infection may involve a prodromal state involving pain,itching,or burning at the site of exposure.3The patient described herein because of vaginal pruritus,which was followed by a burning sensation.In this case,the pruritus might have been a prodrome.During the initial infection,viral DNA travels via the axon to the spinal cord sensory ganglion.Reactivation of HSV causes migration back through the axon to the skin and mucosa.
Most cases of genital herpes occur on the genitalia,perineum,buttocks,upper thighs,or perianal areas.Few cases of genital herpes of the urethral orifice have been reported.Based on this case,we advise clinicians to consider genital herpes of the urethral orifice in patients who have no typical symptoms but show HSV-1 or HSV-2 positivity in serological testing.
Serological testing showed that our patient was HSV-1 IgG-positive and HSV-2 IgG-positive.However,serological testing is not routinely recommended in asymptomatic patients.4There is a window of 2 weeks to 6 months after HSV exposure for the formation of detectable antibodies.When the likelihood of infection is low,false-positive test results are more common.How to counsel patients with a positive serologic test result and atypical symptoms is unclear.5In this case,although serological testing was positive for both HSV-1 and HSV-2,the PCR results were positive for HSV-1 DNA and negative for HSV-2 DNA.HSV DNA detection is currently considered the gold standard for diagnosis of genital herpes.4HSV-1 infection cannot be identified by positive HSV-1 serology results alone.HSV-1 antibody is present in 54% of the United States population;it is primarily acquired orolabially in childhood and is often asymptomatic whether in the orolabial or genital region.6Considering the increased incidence of new genital HSV-1 infections and changing sexual practices,it is necessary to educate patients to be aware of the risk of transmitting HSV to uninfected partners through oral or genital sex.Studies have shown that crossprotection against HSV-1 by HSV-2 antibodies is incomplete.As a consequence of the decreasing incidence of HSV-1 infection in young adults in the West,it is anticipated that more people will develop HSV-2 infection in the future.2,6
The patient in this report fully recovered after treatment with acyclovir at 400mg three times a day.In addition to acyclovir,valacyclovir and famciclovir are effective in reducing the severity and duration of the infection.Topical agents are not recommended because they are less effective than oral agents and can generate resistance.4
In conclusion,most cases of genital herpes affect the genitalia,perineum,buttocks,upper thighs,or perianal areas.Few reports to date have described genital herpes of the urethral orifice.If a patient presents without typical symptoms but serological testing shows HSV-1 or HSV-2 positivity,genital herpes of the urethral orifice should be considered.
Acknowledgments
This work was supported by the National Natural Science Foundation of China(No.81872212)and the Shanghai Science and Technology Committee(No.17411952500).
- 国际皮肤性病学杂志的其它文章
- The Power of Molecular Genetics in Understanding Heritable Skin Disorders:Introduction to the Special Theme on Genodermatosis
- Piloleiomyoma
- Eruptive Cutaneous Collagenoma:Report of Two Cases
- Clinical Manifestations of Adult Langerhans Cell Histiocytosis with Multisystem Involvement Successfully Treated Using Chemotherapy
- The Association of Psoriasis and Obesity:Focusing on IL-17A-Related Immunological Mechanisms
- Resveratrol Inhibits Secretion of Interleukin 8 by Regulation of Autophagic Flux in Ultraviolet B-stimulated Keratinocytes