The effectiveness of dalethyne dressings for reducing bacteria in diabetic foot ulcers
Suriadi Jais, Djoko Priyono
aDepartment of Medical-Surgical Nursing, The Institute of Nursing Muhammadiyah Pontianak, Pontianak, West Kalimantan 78124, Indonesia
bDepartment of Medical-Surgical Nursing, School of Nursing, Faculty of Medicine, Tanjungpura University, Pontianak, Kalimantan Barat 78124,Indonesia
Abstract: Objective: This study evaluates the effectiveness of a dalethyne dressing for decreasing bacteria in diabetic patients with infected foot ulcers.
Keywords: diabetic ulcer • dalethyne • infection • Staphylococcus aureus
1. Introduction
In 1983, the prevalence of diabetes mellitus (DM) in Indonesia was 1.63%. This percentage increased to 5.7% in 2007 and is predicted to reach 6.0% by 2030. Furthermore, DM affected 8.5 million patients in Indonesia in 2013, a number that is expected to reach 14.1 million by 2035.1Diabetic foot ulcers (DFUs) are a common and serious DM complication that significantly increase the DM treatment costs.2The most common cause of morbidity and mortality in DFU is an infection, which occurs in 40–80% of cases.2The primary causative pathogen,Staphylococcus aureus, may be resistant to multiple drugs.3–5Therefore, managing DFU infections with antimicrobial agents without increasing antibiotic resistance is an important goal requiring the exploration of alternative treatments. Dalethyne, a herbal product that promotes wound healing, has been shown to be effective against antibiotic-resistant ofS. aureusandPseudomonas aeruginosa.6,7This new active compound, extracted by ozonization, consists of a combination of compounds: essential oil (aldehyde),fatty acids (stearic, oleic, linoleic, and palmitic acids),iodine, and peroxide.7When applied to a dressing,dalethyne serves as an antimicrobial agent that can kill bacteria and help to promote new tissue formation on wounded skin.7While dalethyne has been used to treat acute and chronic wounds in Indonesia in all clinical settings, no previous study has examined its use to treat DFU infections. Therefore, the present study evaluated the hypothesis that using a dalethyne in wound dressing would reduce the bacterial counts in infected DFU.
2. Methods
This study was conducted in the outpatient Kitamura Wound Clinic in Pontianak, Indonesia, using a quasiexperimental, non-equivalent, and pretest–posttest control group design. Using non-probability purposive sampling, 30 patients with DFU were selected, enrolled,and distributed into two groups (15 each in the control and experimental groups). The inclusion criteria were patients aged 30–70 years with a DFU who had one or more local infection signs or symptoms, a Wagner wound classification of 2–4 without spreading tissue damage, no complications, a regular wound size, without digit amputation, and complied with follow-up care.
Two registered nurses certified in diabetic wound care at the Kitamura Wound Clinic were trained to collect samples using the study protocols. The intervention group was treated with a dalethyne dressing, whereas the control group was treated with a standard dressing according to Kitamura Wound Clinic’s wound care management guidelines. The following data were collected for each patient: demographic characteristics (age and sex), HbA1c level, ankle-brachial index (ABI), Wagner ulcer classification, wound duration, DM duration, and blood pressure reading.
The two trained nurses performed bacterial count assessments for patients in both groups. To collect the samples, the research assistants swabbed the longest axis of the ulcer once, using a cotton-tipped sterilized swab. The swab was then placed in a normal saline bottle that was inserted into the bacteria counter. The per swab bacterial count was measured at the bedside within 60 s.
The bacterial culture samples were investigated twice at intervals of 4 weeks (on the first week at the first treatment and again on the fourth week after treatments). Bacterial counts were measured after wound cleansing to evaluate the bacterial bioburden on the wound surface. The swabs were transported immediately to the Department of Microbiology at the Faculty of Medicine, Tanjungpura University, where the bacterial culture was analyzed by a microbiologist. The rapid bacteria quantification system (Bacteria Counter,DU-AA01NP-H; Panasonic Healthcare Co. Ltd., Tokyo,Japan) was used to measure the bacterial counts.8This device can quantify data ranging from 1.0 × 105colonyforming units (CFU)/mL to 1.0 × 108CFU/mL. Bacterial counts >1.0 × 107CFU/mL were considered high.
Institutional ethical clearance was obtained from the Institute of Nursing Muhammadiyah (Board no. 76/II.I.AU/Ket.ETIK/S-1/III/2019), and informed consent was obtained from all the subjects. The participants were followed and observed for 4 weeks. After discharge, all participants were continued to receive care from the staff nurses at the Kitamura Wound Clinic.
Descriptive statistics were calculated for each group(mean and standard deviation values) before the mean bacteria count scores were analyzed. Statistical analyses were performed using a Mann–Whitney-Wilcoxon test andt-test, with a value of <0.05 considered statistically significant. SPSS version 20.0 (SPSS Inc.,Chicago, IL) was used to analyze all data.
3. Results
Data were collected from 30 participants recruited from among the Kitamura Wound Clinic outpatients treated for local DFU infections from March to September 2018(Figure 1). Half of the study participants were male and half were female. At the first assessment, 40% of the participants had wounds that had lasted for 2 weeks and 36.7% had wounds that had lasted for 1 week. More than half the participants (53.3%) had suffered from DM from 4 years to 7 years (Table 1). The control and intervention groups did not differ significantly in the HbA1c level, age,blood pressure level, or ABI (P> 0.05; Table 2). The Wilcoxon sign rank test (P< 0.05) indicated that both groups had statistically significant bacteria count reductions from pretest to posttest (Table 3). The Mann– Whitney test showed that the intervention group’s bacteria count reduction was significantly greater than that of the control group (P= 0.018; Table 4).
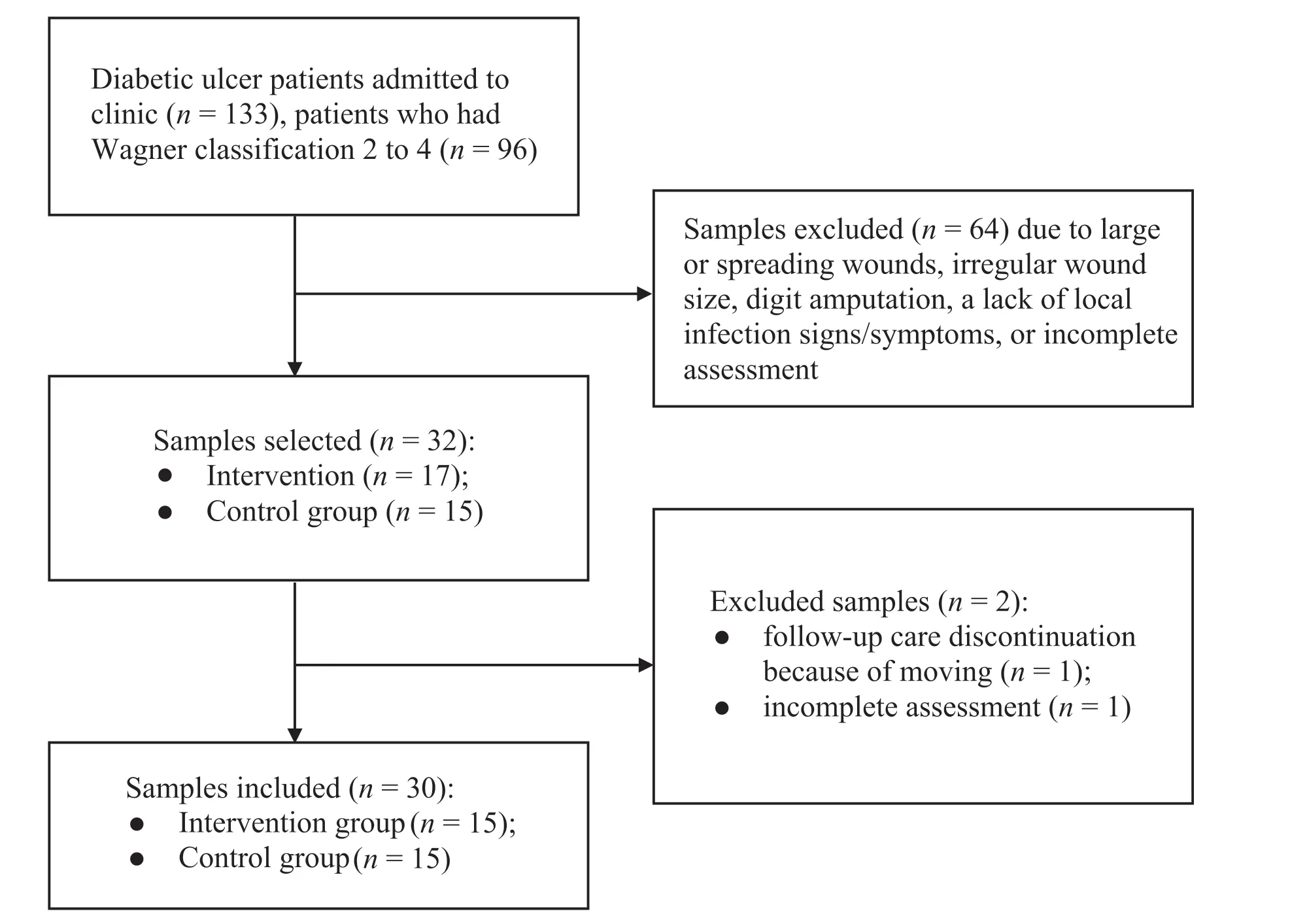
Figure 1. Flowchart of study participants.
The pretest and posttest levels of the four types of bacteria are shown in Table 5. In both groups,Proteus mirabilisandCitrobacter freundiibacteria were found in the pretest and posttest samples (Table 5).S. aureusbacteria were found in both group’s pretest samples and the control group’s posttest sample, but not in the intervention group’s posttest sample.Bacillus subtiliswas found in the intervention group’s pretest and posttest samples, but not in either of the control group’s samples. Finally,Bacillus megateriumwas found only in thecontrol group’s pretest sample, not in the intervention group’s pretest sample, or either groups’ posttest samples.

Table 1. Participant characteristics.
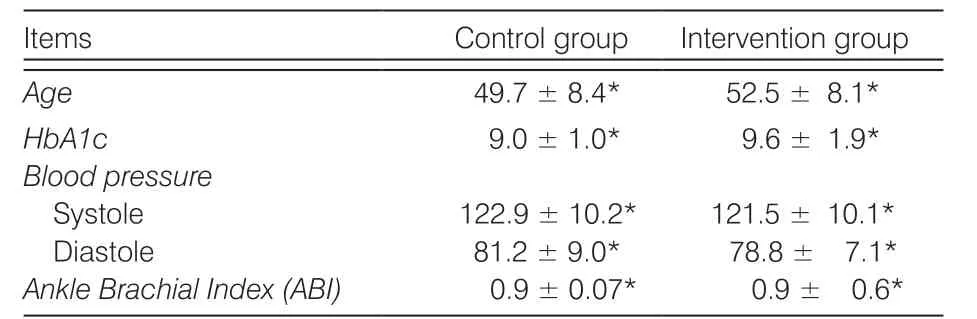
Table 2. Differences between control group and intervention group(M±SD).
4. Discussion
The findings of this study support the hypothesis that using a dalethyne dressing reduces the bacterial counts in infected DFUs. In accordance with previousfindings,S. aureuswas the most frequently isolated pathogen in this study.3,9,10In contrast to previous reports, the present study does not support the contention thatEscherichia coliandP. aeruginosaare common pathogens in DFU infections.11In this study,the number of bacteria decreased in the intervention group after treatment with a dalethyne dressing. As in previous studies, dalethyne eliminatedS. aureus,a common infection in DFU ulcers in the present study’s intervention group.6,7S. aureusis dangerous because it secretes toxins that can lead to tissue necrosis.These toxins play an important role in deepening and spreading DFU infections.12However,B. subtiliswas found in the intervention group at pretest and posttest, indicating that dalethyne is not effective in killing these bacteria. Fortunately, most types ofB. subtilisare non-pathogenic.13The findings of the present study also showed that dalethyne was not effective for killingP. mirabilisorC. freundii. While previously recognized as an environmental contaminant or colonizer with low virulence,C. freundiiis now known to cause a wide spectrum of infections involving the urinary tract,peritoneum, respiratory tract, wounds, soft tissues,urinary tract, liver, biliary tract, peritoneum, intestines,bone, respiratory tract, endocardium, meninges, and the bloodstream.14BothP. mirabilisandC. freundiiare frequently isolated in infected wounds.15Confirming this fact, the present study also found that both bacteria are virulent and frequently found in DFU infections.14–16

Table 3. Pretest and posttest independent bacteria counts.

Table 4. Posttest bacteria count differences.
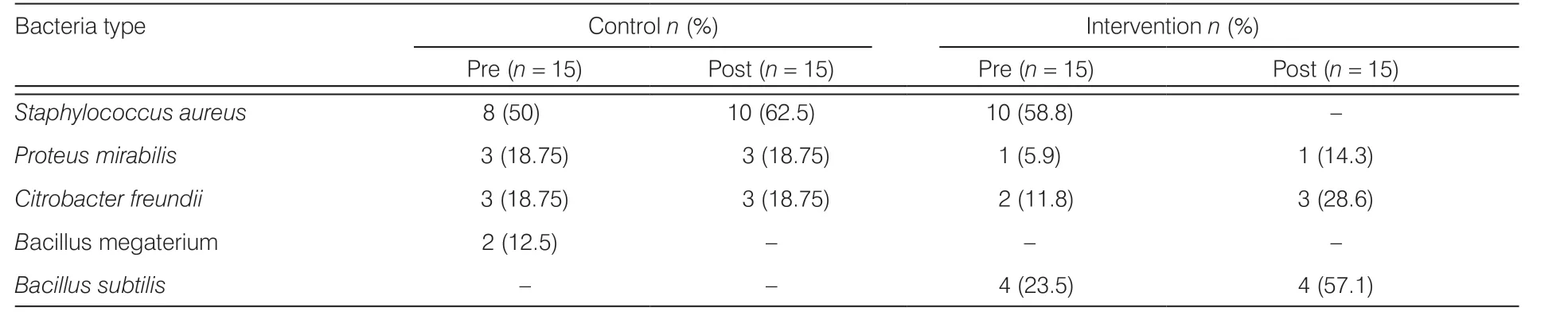
Table 5. Type of bacteria present in pretest and posttest samples.
The findings from this study show a greater decrease in the number of bacteria in the intervention group compared with the control group and confirm that dalethyne has some benefits for wound treatment. Bacterial bioburden has two aspects: bacterial count and pathogenicity. The culture method, which is widely used in clinical settings, quantifies the bacterial count.8Having a decreased number of bacteria in a wound is associated with reduced inflammation.8However, pathogenicity also plays an important role in clinical outcomes.In this study, both groups had bioburdens; all cultures were pathogenic and had more than one microbe.Furthermore, the number of bacteria decreased in both groups. The key fact here is that all chronic wounds are colonized by bacteria. Therefore, the most important goal in wound care management is to reduce the number of bacteria to accelerate the wound healing process.17Both groups experienced a significant reduction in the number of bacteria, which can facilitate the wound healing process. The desired result in wound care management is to attain the greatest possible bacteria-level reduction without introducing other complications. In the present study, the key finding was that, compared with the control group, the intervention group experienced a greater reduction in the number of bacteria as well as a complete elimination ofS. aureus, the virulent bacteria that causes most DFU infections. These results suggest that treating infected wounds with dalethyne can effectively killS. aureus.
The results of this study suggest the benefits of using dalethyne dressings in the management of chronic infectious wounds in diabetic patients. In addition to reducing the virulent bacteria ofS. aureusand promoting wound healing, dalethyne offers the additional advantage of not having negative effects on wounds.
5. Conclusions
The results of this study indicate that dalethyne is effective in killingS. aureusand can reduce the bioburden in DFU infections.
Limitations
The limitations of this study include the small sample size,which limits the statistical power and generalizability of these findings. Furthermore, because this study did not continue documenting follow-up care until all the wounds had healed completely, any between-group differences in long-term healing acceleration remain unknown. Future studies should include larger samples at multiple centers to identify other factors that affect wound progression and healing and detect biofilm in wounds.
Acknowledgment
The authors thank Dermozone and the Soho Company, which supported the study, and the staff nurses at Kitamura Wound Clinic, who participated in this study.
Ethical approval
Ethical issues are not involved in this paper.
Conflicts of interest
All contributing authors declare no conflicts of interest.
- Frontiers of Nursing的其它文章
- Evaluation of the intervention of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease
- Relationship between decreased visual acuity and physical activity time in school age children
- Study on the quality of life and its related factors for older adults in communities in Beijing, China†
- Study and promotion of safety culture using mixed methods research
- Development of a questionnaire assessing nursing staff’s knowledge, attitude, and practice on the prevention of the nosocomial infection in elderly patients:testing reliability and validity†
- Evaluation of undergraduate students’ nursing assessment and communication skills through an objective structured clinical examination within a high-fidelity simulation using a student-simulated patient†

