Efficacy and safety of distal radial approach for cardiac catheterization:A systematic review and meta-analysis
Toshihide Izumida,Jun Watanabe,Ryo Yoshida,Kazuhiko Kotani
Toshihide Izumida,Division of Community Medicine,Kanazawa Medical University Himi Municipal Hospital,Himi 935-8531,Toyama,Japan
Jun Watanabe,Kazuhiko Kotani,Center for Community Medicine,Jichi Medical University,Shimotsuke-City 329-0498,Tochigi,Japan
Ryo Yoshida,Department of Internal Medicine,Iwami Hospital,Iwami-Town 681-0003,Tottori,Japan
Abstract BACKGROUND The traditional radial approach (RA) is recommended as the standard method for coronary angiography (CAG),while a distal RA (DRA) has been recently used for CAG.AIM To assess the efficacy and safety of the DRA vs RA during CAG.METHODS The following databases were searched through December 2020:MEDLINE,the Cochrane Central Register of Controlled Trials,EMBASE,the World Health Organization International Clinical Trials Platform Search Portal,and Clinical-Trials.gov.Individual randomized-controlled trials for adult patients undergoing cardiac catheterization were included.The primary outcomes were the successful cannulation rate and the incidence of radial artery spasm (RAS) and radial artery occlusion (RAO).Study selection,data abstraction and quality assessment were independently performed using the Grading of Recommendations,Assessment,Development,and Evaluation approach.RESULTS Three randomized control trials and 13 registered trials were identified.The two approaches showed similar successful cannulation rates [risk ratio (RR) 0.90,95%confidence interval (CI):0.72-1.13].The DRA did not decrease RAS (RR 0.43,95%CI:0.08-2.49) and RAO (RR 0.48,95%CI:0.18-1.29).Patients with the DRA had a shorter hemostasis time in comparison to those with the RA (mean difference -6.64,95%CI:-10.37 to -2.90).The evidence of certainty was low.CONCLUSION For CAG,the DRA would be safer than the RA with comparable cannulation rates.Given the limited data,additional research,including studies with standard protocols,is necessary.
Key Words:Radial artery;Cardiac catheterization;Coronary angiography;Snuff box;Systematic review;Meta-analysis
INTRODUCTION
Coronary angiography (CAG) is an invasive but essential part of the diagnosis and treatment for coronary artery disease (CAD).Annually,it is estimated that 1016000 inpatient diagnostic CAG and 480000 inpatient percutaneous coronary intervention(PCI) procedures are performed in the United States[1].In European countries,it is estimated that 4500 diagnostic coronary angiograms per million people and 2000 PCI procedures per million people are performed each year[2].Interventional cardiologists gain accessviaa peripheral artery,and the latest guidelines from the European Society of Cardiology,National Institute for Health and Care Excellence,and American College of Cardiology/American Heart Association recommended the radial approach(RA) over the transfemoral,transbrachial,and transulnar approaches,because it is associated with a reduced risk of cardiac death,all-cause mortality,bleeding,and access site complications[3-5].
The distal RA (DRA) was recently introduced,as this approach may have some potential advantages in comparison to the RA[6,7].Previous observational studies showed that the two approaches were associated with similar successful cannulation rates[8],while the rates of vascular complications in the DRA,including radial artery occlusion (RAO) and radial artery spasm (RAS),were less frequent than the RA[9-16].The DRA is assumed to be an alternative approach to the RA,but the efficacy of the two approaches has never been systematically reviewed and analyzed.
Therefore,the present study aimed to evaluate the efficacy and safety of the DRA in comparison to the RA.To achieve this aim,a systematic review and meta-analysis of only randomized-controlled trials (RCTs) were conducted to produce high-quality evidence that would inform clinical practice decisions for guidance of the cardiac catheterization procedures concerning these two approaches.
MATERIALS AND METHODS
Literature search
Our review protocol was registered in protocol.io (dx.doi.org/10.17504/protocols.io.bramm2c6).Our study was performed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) Statement[17].
Individual RCTs were included to evaluate the efficacy and safety of the RAvsDRA for cardiac catheterization.All papers,including published and unpublished articles,abstracts of conferences,and letters,were included,regardless of language,country restrictions,or publication year.Non-RCTs were excluded.The inclusion criteria were adult patients (≥ 18 years of age) undergoing diagnostic CAG and PCI for CAD.Patients for whom a >7-Fr sheath was used were excluded (available on a commercial basis)[18].The DRA is a method of puncturing distal radial arteries at the proximal part of the anatomical snuffbox or the first intermetacarpal space.After successful artery puncture,a guidewire is smoothly passed through the needle and used to guide the sheath through the artery.After introduction of the sheath,interventional cardiologists perform diagnostic CA and PCI with the coronary catheters through the sheath[19].The RA is a method of puncturing radial artery at the forearm,a few centimeters above the wrist joint[20].The primary outcomes were the successful cannulation rate and the incidence of RAS and RAO.The successful cannulation rate was defined as completion of the procedure without cross-over to another access site or as defined by practitioners.RAS was diagnosed by angiographic evaluation of the radial artery.RAO was diagnosed based on the absence of flow on color Doppler ultrasound.The secondary outcomes were the mean number of punctures per patient and the mean time for hemostasis.The success of hemostasis was defined as no bleeding or hematoma formation after release.The total time was defined as the time from when the sheath was removed to when successful hemostasis was confirmed.All outcomes included the definitions of the authors of original studies.
The following databases were searched through December 2020:MEDLINE,the Cochrane Central Register of Controlled Trials,and EMBASE (Supplementary material,Appendix 1).The World Health Organization International Clinical Trials Platform Search Portal and ClinicalTrials.gov databases were also searched for ongoing or unpublished trials (Supplementary material,Appendix 2).The original authors were asked for unpublished or additional data if necessary.The reference lists of studies,including international guidelines published by the European Society of Cardiology,National Institute for Health and Care Excellence,and American College of Cardiology/American Heart Association[3-5],as well as the reference lists of eligible studies and articles citing eligible studies,were checked.
Study selection
Two independent reviewers (Izumida T and Yoshida R) screened the titles and abstracts,then assessed the eligibility based on the full text.We contacted the original authors when relevant data were missing.Disagreements between the two reviewers were resolved by discussion,and when this failed,a third reviewer acted as an arbiter(Watanabe J).
Data extraction
Two reviewers (Izumida T and Yoshida R) performed independent data extraction of the included studies using a standardized data collection form.The form included information on the study design,study population,interventions,and outcomes.Any disagreements were resolved by discussion,and when this failed,a third reviewer acted as an arbiter (Watanabe J).
Risk of bias
Two reviewers (Izumida T and Yoshida R) evaluated the risk of bias independently using the Risk of Bias 2[21].Disagreements between the two reviewers were resolved by discussion,and when this failed,a third reviewer acted as an arbiter (Watanabe J).
Statistical analysis
We pooled the relative risk ratios (RRs) and 95% confidence intervals (CIs) for the following binary variables:Cannulation success,RAS,and RAO.We pooled the mean differences and the 95%CIs for the following continuous variables:Mean time for hemostasis.An intention-to-treat analysis was performed for all dichotomous data (to the extent that was possible).For continuous data,missing data were not imputed based on the recommendation of the Cochrane handbook[22].A meta-analysis was performed using the available data in the original study.The Review Manager software program (RevMan 5.4.1) was used to perform the meta-analysis.A randomeffects model was used.The statistical heterogeneity was evaluated by a visual inspection of forest plots and calculation of theI2statistic (I2values of 0%-40%:Might not be important;30%-60%:May represent moderate heterogeneity;50%-90%:May represent substantial heterogeneity;75%-100%:May represent considerable heterogeneity)[22].When there was substantial heterogeneity (I2>50%),the reason for heterogeneity was assessed.The Cochrane chi-squared test (Q-test) was performed for theI2statistic,andPvalues of <0.10 were considered statistically significant.A funnel plot was not created and the Egger test was not performed because <10 trials were included in our analysis[22].The following subgroup analyses of the primary outcomes were performed when sufficient data were available:For participants,the young- to middle-age group (<65 years of age)vsthe elderly group (≥ 65 years of age)and for intervention,right-side approachvsleft-side approach[23,24] and diagnostic CAvsPCI.For the sensitivity analyses of the primary outcomes,studies using imputed statistics were excluded and participants were only included if they completed the study and their data were complete.
RESULTS
Study selection
Figure 1 shows the flow of the study selection of studies comparing the DRAvsRA for cardiac catheterization.We identified a total 752 records (MEDLINE 63 records,EMBASE 150 records,CENTRAL 36 records,ClinicalTrials.gov 132 records,and ICTRP 371 records) published prior to December 7,2020.After the initial screening,16 trials met the inclusion criteria.Among these trials,we identified eight ongoing trials(NCT03611725,NCT03986151,NCT04171570,NCT04194606,NCT04211584,NCT04232488,NCT04318990,KCT0004537),five protocols without results(NCT03373565,NCT04001764,NCT04023838,NCT04125992,NCT04238026),and three clinical trials.
Table 1 summarizes the characteristics of eligible studies.Three studies included 519 participants[16,25,26].Table 2 and Supplementary Tables 1-4 show the risk of bias in each study.The overall risk of bias for the successful cannulation rate was similar in the three studies.
Primary outcomes
Successful cannulation rate:Three studies were eligible for the evaluation of the successful cannulation rate[16,25,26].In one study,the operators were specialists,and in the other two studies,the operators’ skills were unknown.The DRA resulted in little to no difference in the successful cannulation rate in comparison to the RA (RR 0.90,95%CI:0.72-1.13;I2= 93%) (Figure 2A).
Incidence of RAS:The incidence of RAS was measured in two of three studies[16,25].The two studies used verapamil and nitrate,respectively[16,25].The DRA did not reduce the incidence of RAS (RR 0.43,95%CI:0.08-2.49;I2= 29%) (Figure 2B).
Incidence rate of RAO:Two of the three studies were eligible for the evaluation of incidence of RAO[25,26].The DRA did not reduce the incidence of RAO (RR 0.48,95%CI:0.18-1.29;I2= 0%) (Figure 2C).
We could not perform a pre-specified subgroup analysis or sensitivity analyses for the successful cannulation rate,the incidence of RAS,or the incidence of RAO.
Secondary outcomes
Mean number of punctures:We included one RCT for the evaluation of mean number of punctures[25].In the study,the mean number of punctures per patient was 2.4 with the DRA and 1.6 with the RA.
Mean time for hemostasis:Two of the three studies were eligible for the evaluation of the mean time for hemostasis[16,26].In one study,hemostasis was performed only by manual compression without using a device[16],and in the other study,it was unclear whether a device was used[26].The DRA reduced the mean time for hemostasis in comparison to the RA (mean difference -6.64,95%CI:-10.37 to -2.90;I2= 88%)(Figure 3).

Table 1 Summary of the characteristics of the eligible studies
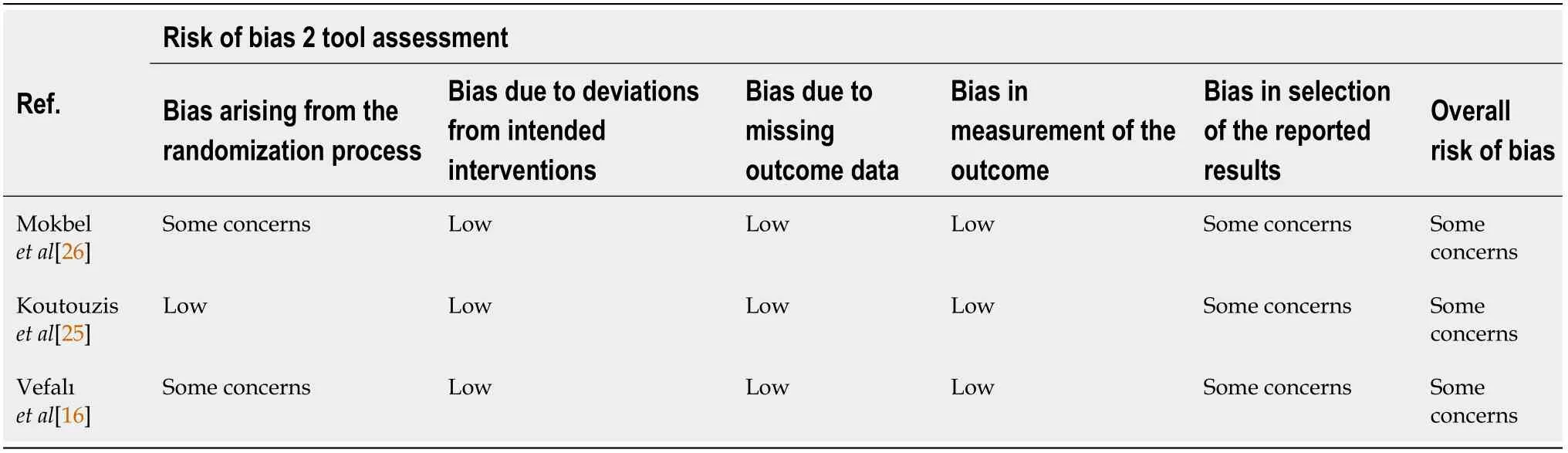
Table 2 Quality scores for the studies eligible for the evaluation of the successful cannulation rate
Certainty of evidence
The certainty of the evidence was low for the successful cannulation rate because of inconsistency due to substantial heterogeneity and imprecision due to the small sample size.The certainty of evidence was low for RAS,RAO,and the mean number of punctures because of imprecision due to small sample size and the small number of participants.The certainty of the evidence was very low for the mean time for hemostasis because of substantial heterogeneity,imprecision,and a high risk of bias(Table 3).
DISCUSSION
In the present review,the rate of cannulation failure with the DRA was suggested to be similar to that with the RA.Furthermore,the DRA might reduce the incidence of RAS and RAO in comparison to the RA.Additionally,the DRA had a shorter hemostasis time.These findings indicate the safe clinical practice analyses of the DRA to guide cardiac catheterization procedures.
The puncture of the distal radial artery has some caveats because of anatomical features such as the superficial position of the artery and the bone basement.The puncture site in the DRA is either the distal radial artery of the anatomic snuffbox or the more distal radial artery,which is located on the vertex of the angle between the tendon of the extensor pollicis longus and the second metacarpal bone[7].Some studies showed that the diameter of distal radial artery was smaller and might have the increased tortuosity and angulations in comparison to forearm radial artery[25,27,28].However,considering the similar results of successful cannulation rates and puncture counts for DRA and RA arms in our review,these anatomical factors might have little effect on the efficacy of the procedure.
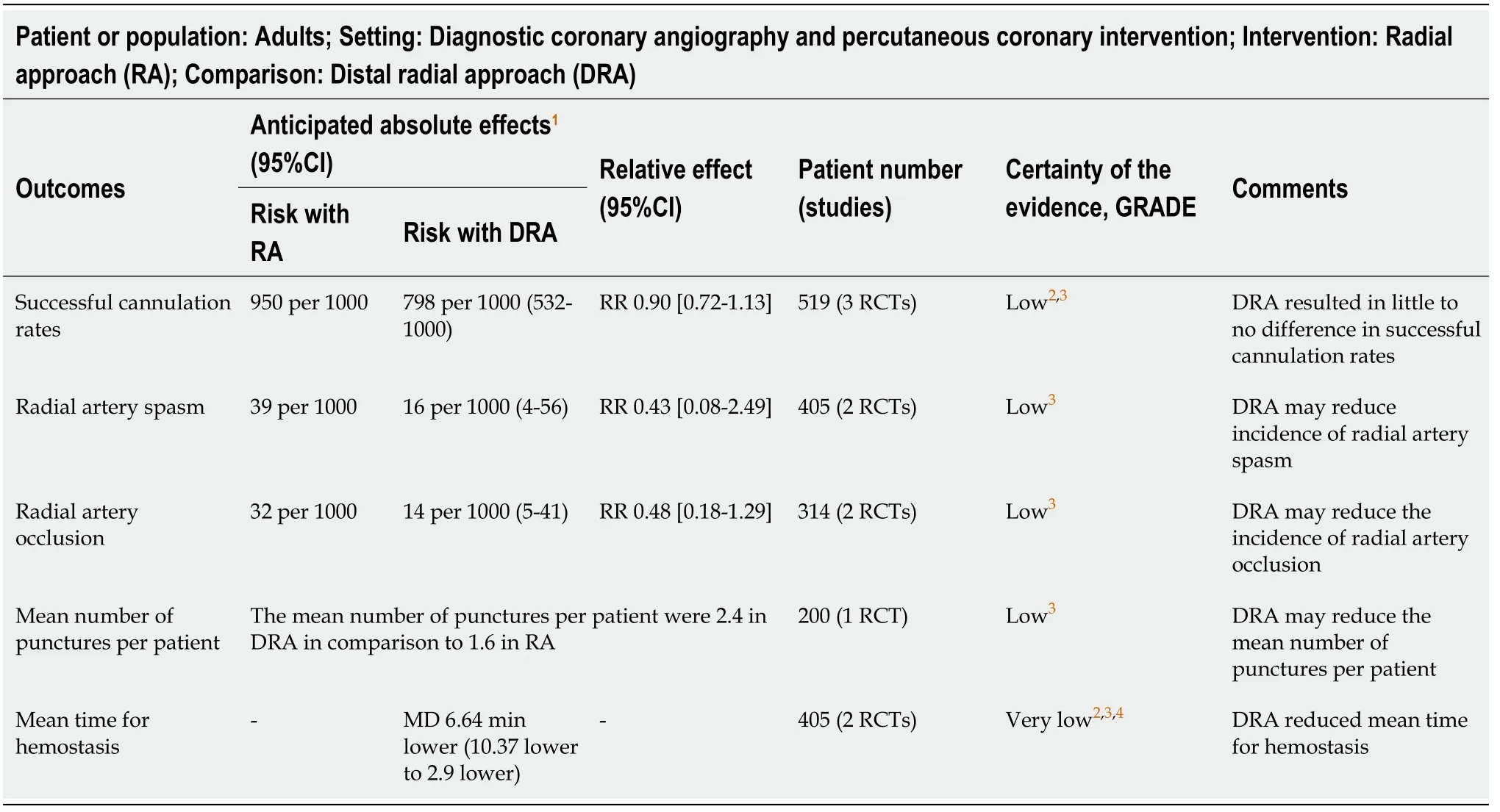
Table 3 Summary of findings (the efficacy and safety of the radial approach vs the distal radial approach for diagnostic coronary angiography and percutaneous coronary intervention)
RAS is one of the most frequent complications in cardiac catheterization[29,30] and can be caused by mechanical stimulation by guide wires or catheters and increasing catecholamine levels,which are induced by pain and discomfort[28].In previous systematic reviews,additional drugs,such as local anesthetics and vasodilatory medications,reduced RAS[31,32].In the present review,the DRA arm was likely to reduce the incidence of RAS,despite the use of additional medications.Although the detailed mechanism remains unknown,a previous study reported that the DRA might be associated with more advantages in terms of patient satisfaction and the analgesic effect[16,33].
RAO is relatively common,with an incidence ranging from 0.6% to 2.2%;it occurs through the inflammation and endothelial dysfunction of the radial artery[34,35].Regarding possible explanations for the lower incidence of RAO in the DRA arm,the first possibility seemed to be the anatomical features of the distal radial artery.The antegrade flow through the superficial palmar arch can be maintained during compression of the distal radial artery,resulting in a low risk of retrograde thrombus formation[6].The second possibility was the shorter duration of hemostasis with the DRA[7],which appeared to be related to the structure of the anatomic snuffbox with a bony basement surrounded by tendons.
The mean number of punctures in the DRA could be mostly comparable to that in the RA.The operators were mainly specialists in the study setting;however,in the clinical setting,the DRA is associated with a learning curve because it involves the puncture of small and weak arteries[36].Ultrasound is useful for increasing the rate of successful puncture and for reducing adverse events.The measurement of the diameter of the distal radial artery helps to select a suitable sheath,leading to reduced damage of the endothelium and reduced development of RAS and RAO[28].The use of ultrasound may alter the results of similar studies in the future.Research is needed to evaluate the usefulness of ultrasound in the DRA.

Figure 1 Study selection.

Figure 2 Forest plot.
The shorter time of hemostasis in the DRA,as found in the present review,is a useful aspect of this approach for the prevention of vascular damage.Due to the anatomical features of the distal radial artery,the DRA can reduce the hemostasis time.A new compression hemostasis device for the puncture site of the distal radial artery was also developed,and the safety and efficacy of the device were validated[37].Mechanical compression is more convenient and requires fewer human resources in comparison to manual compression[38].In the present review,hemostasis was performed by manual compression.Further research is needed to evaluate the DRA using mechanical compression hemostasis.
The present review had some limitations.First,our review included a relatively small number of studies.Second,various definitions may have been applied for RAS,RAO,and hemostasis,because the protocols were not described.To improve the quality of evidence and draw convincing conclusions,it will be necessary to perform large cohort studies with standard protocols.

Figure 3 Forest plot of the mean time for hemostasis.
CONCLUSION
This first systematic review and meta-analysis to compare clinical data using the DRA and RA indicated that the DRA would be safer than the RA,with comparable procedure rates.Given the limited data,accumulating more knowledge by further research,including studies with standard protocols,is required to establish clinical practice using the DRA.
ARTICLE HIGHLIGHTS
Research background
While the traditional radial approach (RA) is the gold standard method for cardiac catheterization,a distal RA (DRA) has been recently introduced.
Research motivation
The DRA may have some advantages compared to RA;however,it is not fully understood as to which technique for coronary angiography—DRA or RA—is more beneficial to the patients.
Research objectives
Via the systematic review and meta-analysis,we compared clinical data using the DRA and RA.
Research methods
The databases MEDLINE,the Cochrane Central Register of Controlled Trials,EMBASE,the World Health Organization International Clinical Trials Platform Search Portal and ClinicalTrials.gov were searched.All randomized-controlled trials for adult patients undergoing cardiac catheterization until December 2020 were included.The primary outcomes were the successful cannulation rate and the incidence of radial artery spasm (RAS) and radial artery occlusion (RAO).The statistical analysis was performed on a random-effect model to pool the relative risk ratios (RRs) and 95%confidence intervals (CIs) for the binary variables,such as cannulation success,RAS,and RAO.
Research results
Three randomized-control trials including 519 participants and 13 registered trials were identified.The two approaches showed similar successful cannulation rates (RR 0.90,95%CI:0.72-1.13).The DRA did not decrease RAS (RR 0.43,95%CI:0.08-2.49) and RAO (RR 0.48,95%CI:0.18-1.29).The evidence of certainty was low.
Research conclusions
The present study indicated the DRA to be safer than the RA,with comparable procedure rates.Importantly,there are limitations,including the limited study numbers and no studies with standard protocols,that prevent definitive conclusions.
Research perspectives
Further research,including studies with standard protocols,is required to establish clinical practice using the DRA.
ACKNOWLEDGEMENTS
The authors would like to thank Dr.Babunashvili A,Dr.Lee JW,and Dr.Park JC for providing us with unpublished details of studies for the review.We thank Ms.Fujiwara C for providing us with International Clinical Trials Registry Platform search data.