Peroral endoscopic myotomy in a pregnant woman diagnosed with mitochondrial disease:A case report
Alexander A Smirnov,Maya M Kiriltseva,Mariya E Lyubchenko,Vladimir D Nazarov,Anna V Botina,Aleksandr N Burakov,Sergey V Lapin
Alexander A Smirnov,Maya M Kiriltseva,Mariya E Lyubchenko,Aleksandr N Burakov,Department of Endoscopy,Pavlov First Saint Petersburg State Medical University,Saint Petersburg 197022,Russia
Vladimir D Nazarov,Sergey V Lapin,Center for Molecular Medicine,Pavlov First Saint Petersburg State Medical University,Saint Petersburg 197022,Russia
Anna V Botina,Department of Pathology,Pavlov First Saint Petersburg State Medical University,Saint Petersburg 197022,Russia
Abstract BACKGROUND Achalasia is a primary esophageal motility disease characterized by impairment of normal esophageal peristalsis and absence of relaxation of the lower esophageal sphincter.Sometimes is can be a part of some genetic disorders.One of the causes of gastrointestinal motility disorders,including achalasia,is mitochondrial defects.CASE SUMMARY We report about a pregnant woman with a history of symptoms associated with inherited mitochondrial disease,which was confirmed by genetic tests,and who was treated via peroral endoscopic myotomy.CONCLUSION Peroral endoscopic myotomy is possible treatment option for a pregnant woman with achalasia caused by mitochondrial disease.
Key Words:Mitochondrial disease;Pregnancy;Esophagus;Peroral endoscopic myotomy;Achalasia;Biopsy;Case report
INTRODUCTION
Achalasia is a primary esophageal motility disease characterized by impairment of normal esophageal peristalsis and absence of relaxation of the lower esophageal sphincter[1].It can exist as an independent disease or part of some genetic disorders.One of the causes of gastrointestinal (GI) motility disorders,including achalasia,is mitochondrial defects[2,3].Peroral endoscopic myotomy (POEM) is the safest and most effective method for achalasia treatment[4-7].
CASE PRESENTATION
Chief complaints
A 30-year-old woman presented to our hospital complaining of swallowing difficulty.
History of present illness
A patient had a violation of physical development and constipation from an early age.At the age of 7 years,she was diagnosed with partial bilateral symmetric ptosis.At the age of 8 years,she was referred to the hospital with diagnoses of generalized viral infection of unspecified etiology,postinfectious encephalopathy,cerebro-asthenic syndrome,neurosis,urinary bladder and gut atony,chronic pyelonephritis,mydriasis,semiptosis,and dystrophy.At the age of 9 years,she had suspected high intestinal obstruction which was followed by surgery.The obstruction was not revealed during the surgery.In the postoperative period,signs of intestinal obstruction persisted,and they were managed conservatively.After the surgery,she developed meningeal signs,gaze paresis,double vision,and reduced vision.Electrocardiogram showed an incomplete type of blockade of the right branch of the bundle of His.Esophagogastroduodenoscopy (EGD) showed gastric hypotony.Computed tomography scans of the head revealed moderate diffuse cortex atrophy.Cerebrospinal fluid was clear with 0.066.The patient was seen by a neurologist,ophthalmologist,infectious diseases specialist,and neurosurgeon.However,the diagnosis remained unclear.The following pathologies were excluded:neuro infections,intestinal infections,oncohematology,and endocrine pathologies.Further generalized pathology persisted.At the age of 10 years,a second laparotomy was performed followed by a temporary ileostomy because of signs of acute intestinal obstruction.From the ages of 11 years to 14 years,the patient was annually referred to the surgery department with signs of acute intestinal obstruction,which were managed conservatively.At the age of 11 years,she was diagnosed with intestinal pseudo-obstruction.From the age of 11 years,paradontosis began.From the age of 14 years,the patient had daily dysphagia while eating solid and liquid food.She lost 5 kg and began feeling weak and fatigued.At the age of 15 years,resection of the jejunum was performed two times with an overall resection length of 90 cm because of acute intestinal obstruction which was not managed conservatively.The patient was dystrophic,which was thought to be because of malabsorption as a consequence of the resection of the jejunum.At the age of 25 years,the patient lost all her teeth because of progressive paradontosis.From the age of 26 years,she developed amenorrhea.At the age of 29 years,esophagography showed signs of achalasia,gastroptosis,and delayed gastric and duodenum emptying time.At the age of 30 years,the patient was referred to the endoscopy department of Pavlov Medical University for achalasia treatment.
History of past illness
History of present illness includes the patient’s entire life.That is why we suppose that this part is irrelevant in this case.
Personal and family history
The mother,father,and sister are healthy.There was no family history of GI or autoimmune pathologies or allergic disorders.The niece (4 years of age) had sensorineural hearing loss.
Physical examination
Eckardt score was 4.Her weight was 38 kg.Her body mass index was 16.9,and she had protein energy malnutrition.During preoperative preparation,the patient was revealed to be 16 wk pregnant.She was not aware of the pregnancy.In addition,intraventricular blockage was diagnosed.High-resolution esophageal manometry showed achalasia type I (Figure 1).Hemoglobin and total blood protein levels were 106 g/L and 64 g/L,respectively.Creatine phosphokinase and lactate levels were normal.Neurologic and ophthalmologic disorders were not observed.Considering all data,we suspected mitochondrial disease:incomplete Kearns-Sayre syndrome (KSS)or mitochondrial neurogastrointestinal encephalopathy (MNGIE) disease.
Laboratory examinations
There were myocytes of different thicknesses with sites of wave-like deformation and dystrophic changes.There were also single myocytes with necrobiotic changes and small vessels with“edge standing” leukocytes (Figure 2 and 3).
It showed segment deletion in mitochondrial DNA (mDNA) which affected the genes(MTRNR1) and(MTRNR2).This aberration is considered to be pathogenic and most frequently observed in patients with KSS[8].Unfortunately,after discharge,the patient refused further genetic testing.
FINAL DIAGNOSIS
Achalasia.Mitochondrial disease.KSS? MNGIE?
TREATMENT
Considering the severe dysphagia and cachexia,a multidisciplinary team decided to perform POEM.After performing a submucosal tunnel myotomy of 8 cm in the esophageal muscular layer,a myotomy of 3 cm in the gastric muscular layer was also performed.From the region of the lower esophageal sphincter,5 mm × 5 mm specimens of the lower and middle parts of the esophageal muscle (circular and longitudinal muscles) were obtained for further histological investigation.After the procedure,the endoscope was able to freely pass the lower esophageal sphincter.
OUTCOME AND FOLLOW-UP
The postoperative period was unremarkable.On postoperative day (POD) 2,liquid intake was initiated.It was later followed by eating liquid food.On POD 6,she was discharged in a satisfactory condition with a continuing pregnancy.The first follow-up was performed 3 mo after POEM:Eckardt score was 2,weight was 39 kg (+ 1 kg),EGD was normal,and pregnancy was 29 wk without any ultrasound findings of fetal pathology.
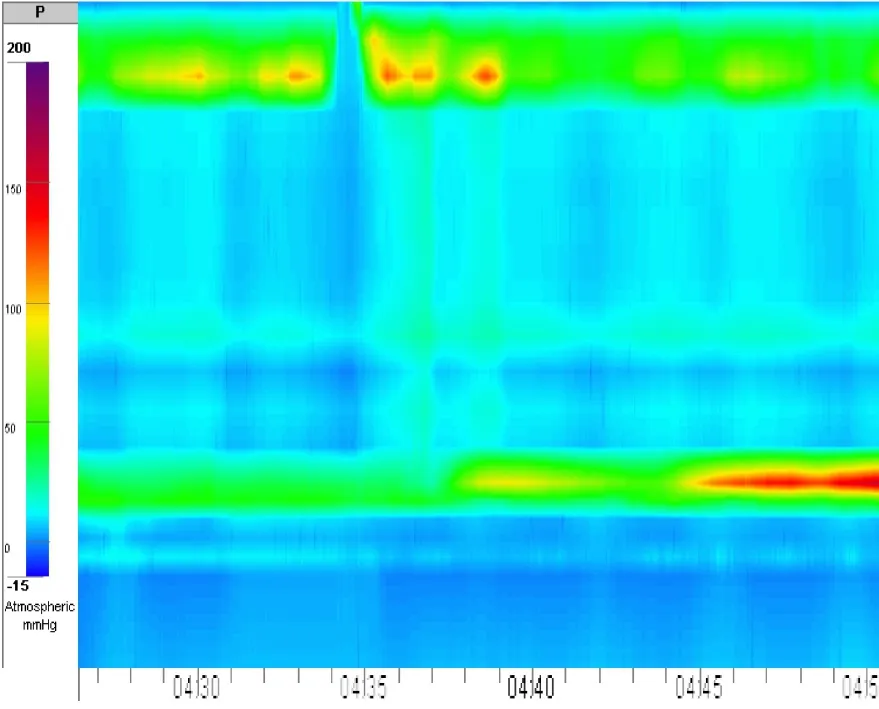
Figure 1 High-resolution esophageal manometry,manometric signs of achalasia type I.

Figure 2 Muscle specimen of the upper part of the esophagus.
DISCUSSION
There are no guidelines on achalasia management in pregnant women.In the literature,achalasia cases in pregnant women were treated in different ways based on the duration of gestation,severity of the disease,and maternal and fetal risk.The most common are botulotoxin injections[9],balloon dilatation[10],Heller myotomy,or in some cases,treatment was delayed until childbirth,and patients received parenteral or enteral nutrition.Concerning nasojejunal feeding tube,the patient was in the beginning of second trimestr of pregnancy.Thus we decided that enteral nutrition is impractical for that long period because it can cause erosions and ulcers in stomach and esophagus.In addition to,long-term usage of nasojejunal feeding tube can also be a source of psychological stress to the patient.As far as dilatation concerned,the first course of dilatation with the use of 30 mm balloon has an efficacy of no more than 80%over the next 6 mo after surgery,resulting in an esophageal perforation rate of 1.1%[11,12].The patient had not undergone Balloon Dilatation before,and we know from the literature that initiating dilatation is 10 times more likely to result in perforation,with a rate of up to 9.7%[13].At the same time,the immediate clinical efficacy of POEM in some studies is more than 1.5 times higher than the efficacy of Balloon Dilatation (94% and 52%,respectively),and POEM is less likely to cause significant complications[14].
To the best of our knowledge,there are no cases of POEM in pregnant women published in the literature.A study by Vogel[15] showed a significant deterioration of the disease when achalasia developed and was not treated before pregnancy.
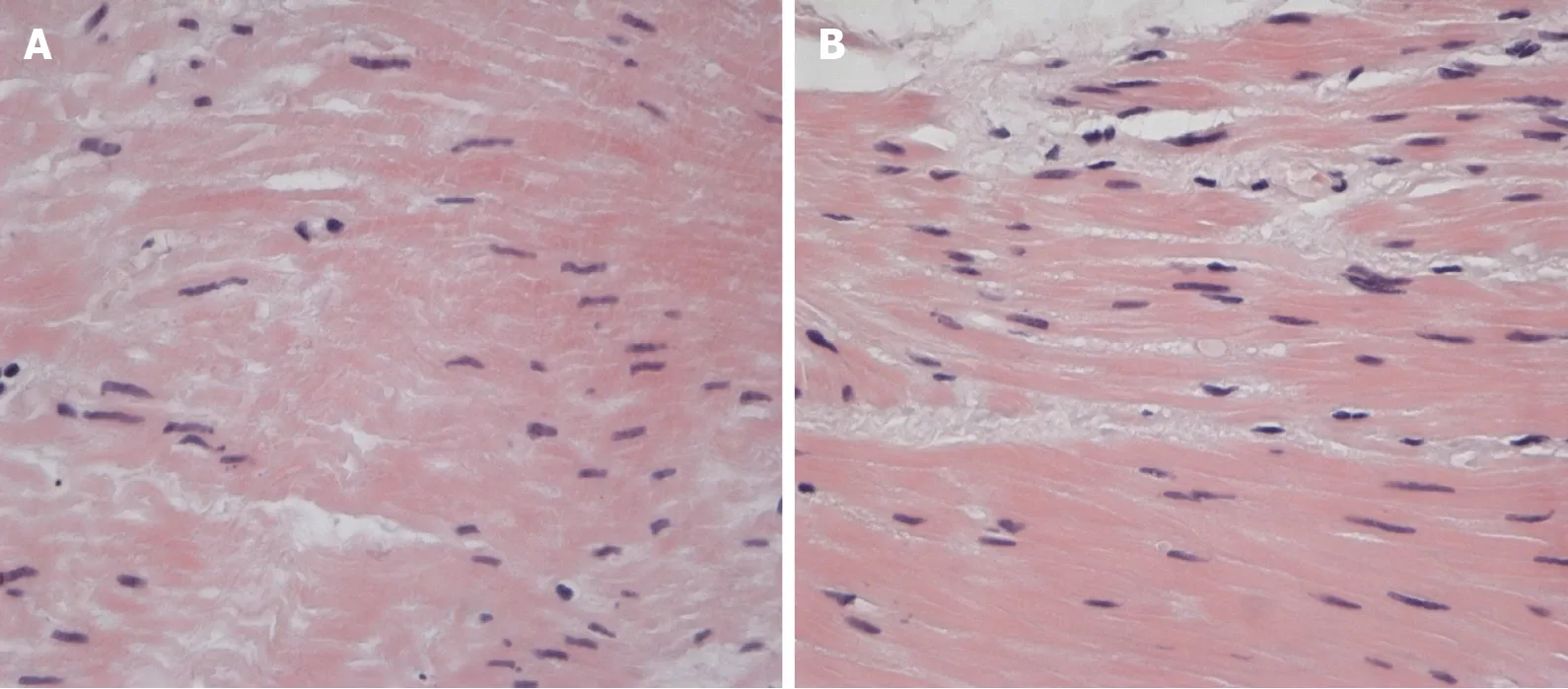
Figure 3 Muscle specimen of the esophagus.
In our case,we chose POEM as the treatment method because we have extensive experience in such endoscopic procedures (more than 150 POEMs).In addition,we have a multidisciplinary team taking care of patients with achalasia.
We revealed a deletion in mDNA;however,this phenotype can as well be observed when mDNA damage is caused by a primary mutation in nuclear DNA (nDNA).These genetic disorders,unlike sporadic isolated mDNA mutations,usually have autosomal recessive inheritance,are less frequently autosomal dominant,and steadily progress[16].Mutations in(MNGIE syndrome) and gene(MNGIE-like syndrome) are the most common mutations of nDNA,which cause impairment of mDNA replication,resulting in severe GI motility disorders,cachexia,polyneuropathy,leukoencephalopathy,ptosis,ophthalmoplegia,and sensorineural hearing loss.In addition,mutations in thegene[17-20].In all aberrations listed above according to the literature,the most common symptom is severe GI motility disorders.
CONCLUSION
To the best of our knowledge,this is the first case of a pregnant woman with a mitochondrial disorder treated successfully with POEM and the first histology of the esophageal muscle layer of a patient with achalasia caused by mitochondrial disease.
 World Journal of Gastrointestinal Endoscopy2021年5期
World Journal of Gastrointestinal Endoscopy2021年5期
- World Journal of Gastrointestinal Endoscopy的其它文章
- Meta-analysis and trial sequential analysis of randomized evidence comparing general anesthesia vs regional anesthesia for laparoscopic cholecystectomy
- Impact of intragastric balloon on blood pressure reduction:A retrospective study in Eastern North Carolina
- Comparison of endoscopic gastritis based on Kyoto classification between diffuse and intestinal gastric cancer
