Semen Analysis and Fecundity Association Among Women with Polycystic Ovary Syndrome Experiencing Ovulatory Dysfunction Treated by Ovulation Induction
Jingshu Gao, Yu Wang, Muai Li, Mengyi Zhu, Xuekui Liu, Hongli Ma, Yijuan Cao,Lu Li, Xinming Yang,*, Xiaoke Wu,h,*
a College of Pharmacy, The Department of Medicine, Hangzhou Normal University, Hangzhou 311121, China
b First Affiliated Hospital, Heilongjiang University of Chinese Medicine, Harbin 150040, China
c Clinical Medical College, Heilongjiang University of Chinese Medicine, Harbin 150040, China
d Department of Endocrinology, Xuzhou Central Hospital, Xuzhou 221009, China
e College of Pharmaceutical Sciences, Zhejiang University, Hangzhou 310058, China
f Department of Obstetrics and Gynecology, The Chinese University of Hong Kong, Hong Kong 999077, China
g Institute of Chinese Medicine, The Chinese University of Hong Kong, Hong Kong 999077, China
h Heilongjiang Provincial Hospital, Harbin 150030, China
Keywords:Semen analysis Fecundity Ovulatory dysfunction Predictive capacity
ABSTRACT In this study, normal values of semen analysis were set for a general infertile population of couples among which most women had normal ovulation. The predictive capacity values of sperm quality,including concentration,motile count,progressive motile count,and morphology,are unclear for women with polycystic ovary syndrome(PCOS).A secondary analysis was conducted based on a randomized controlled trial investigating infertility among women with PCOS experiencing ovulatory disorder between 2011 and 2016 in China. A total of 1000 women received ovulation induction (acupuncture and clomiphene). We randomized the women with PCOS in 27 hospitals in China who received one of four interventions (acupuncture plus clomiphene, sham acupuncture plus clomiphene, acupuncture plus placebo,or sham acupuncture plus placebo). Semen analysis was performed for every male partner according to the World Health Organization (WHO) criteria. The outcomes included conception, clinical pregnancy,and live birth.Logistic regression was used to evaluate the predictive value of semen analysis among ovulatory women for conception,clinical pregnancy,and live birth.Among the 1000 couples, the number of couples who attained ovulation, conception, clinical pregnancy, and live birth were 780, 320, 235, and 205, respectively. Semen volume and motility were applied and used as prediction parameters for conception(area under the curve(AUC)of 0.62(95%confidence interval(CI),0.55-0.69)),clinical pregnancy(AUC of 0.67(95%CI:0.61-0.73)),and live birth(AUC of 0.57(95%CI:0.50-0.64)).No poor calibration was shown for these models in Hosmer-Lemeshow tests.The predictive capacity of semen analysis for treatment outcome in PCOS women with PCOS experiencing with ovulatory dysfunction is limited.
1. Introduction
A major reason of infertility in women is the inability to ovulate.Within this category, polycystic ovary syndrome (PCOS) is the most prevalent cause[1].PCOS is clinically characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology.Researchers have found that aberration of theca cells,defective apoptosis in mature follicles, and disorder related to the insulin signaling pathway are risk factors of PCOS [2]. As a metabolic and polygenetic disorder, PCOS is considered to be relevant to cytochrome P450 family 11 subfamily A (CYP11A), CYP21, sex hormone binding globulin (SHBG), insulin (INS), and especially anti-Mullerian hormone (AMH) and AMH receptor II (AMHRII),which are closely related to ovarian functions [3]. Due to the downstream processing of biotechnology, metabolomics studies reflect a PCOS phenotype more realistically than genomics and proteomics studies. It has been reported that the metabolic pathways of oleic and palmitic acid are intensified in PCOS patients with normal androgen levels [4]. The first-line treatment for PCOS as a cause of infertility is ovulation induction by means of drugs such as clomiphene citrate or letrozole.Assisted reproductive technology (ART) such as in vitro fertilization (IVF), which carries high risk and cost, is another option for women with poor response to ovulation induction [5].
Semen analysis, with parameters that include volume, concentration,motility,morphology,and motile sperm count,is an important laboratory workup to evaluate male fertility [6,7]. However,its normal values are set up for a general infertile population in which most women are ovulatory. Predictive models of sperm quality exist for spontaneous pregnancy among a population without ovulation disorders[8,9].Previous studies have suggested that contact with human sperm could change the function of the fallopian tube [10,11]. The released oocytes of women with PCOS have relatively poor quality, which is probably due to intrinsic genetic defects along with an androgen excess state [12]. Therefore, we hypothesize that the role of semen parameters in predictive models for women with PCOS is different from that in predictive models for normal women. However, few articles focus on the association between the reproductive outcomes of females with ovulatory dysfunction and sperm parameters involving concentration, motile count, progressive motile count, and morphology.
The purpose of this study is to expound on the association between semen analysis and fecundity-related outcomes including conception,clinical pregnancy,and live birth for women with PCOS with ovulatory dysfunction. We performed the analysis based on data extracted from a large sample size: a randomized controlled trial in which PCOS women had induced ovulation for live birth.
2. Methods
2.1. Participants
The study data were extracted from a randomized controlled trial known as PCOSAct from 21 local sites in the mainland of China[13]. All female subjects were diagnosed with PCOS by modified Rotterdam criteria; that is, all female subjects were anovulatory and exhibited hyperandrogenism and/or polycystic ovaries [14].The age range of these anovulating women with PCOS was from 19 to 40 years old, and the mean age was (28.06 ± 3.31) years old. All the subjects signed informed consent for participation in this study.This trial aimed to determine the efficacy of clomiphene and acupuncture for achieving the primary outcome of live birth.All the male partners had semen analysis performed before enrolment and signed informed consent for participation in this study.
PCOSAct was carried out according to the principles of the Declaration of Helsinki.The trial was commenced after having obtained the approval of the Ethic Committee of First Affiliated Hospital,Heilongjiang University of Chinese Medicine. Participants were informed about the risks and benefits of the study, and they were allowed to voluntarily cease their participation in the study at any time for any reasons.
2.2. Semen analysis
At local sites,the male partners were required to provide semen analysis that had been performed within one year in order to confirm eligibility for this study.The mean age of the male partners in the randomized controlled study was (29.94 ± 4.16) years old. If the male partners had had no semen analysis within one year,trained technicians at local laboratories performed a semen analysis. The sperm parameters were evaluated following the World Health Organization (WHO) criteria [7]. The main parameters included volume,concentration,total motility(a+b+c)†† a,b,and c mean sperm motility.Grade a:sperms that fall in this category are the ones with progressive motility,they move fast in a straight line and are the strongest;Grade b:these sperms move in a non-linear direction,they do move forward but in a curved or crooked motion; Grade c: these move in a non-progressive manner, which means they do move their tails but do not progress forward.,and normal morphology. The inclusion criteria for semen analysis are: ①a sperm concentration ≥15 × 106mL-1and progressive motility(a+ b) ≥32% or total motility(a + b + c) ≥40%; or ②a total motile sperm count ≥9 million per single ejaculation.
2.3. Ovulation induction and follow-up
The female participants received one of four interventions(acupuncture plus clomiphene, sham acupuncture plus clomiphene, acupuncture plus placebo, or sham acupuncture plus placebo) for four months. All couples were required to have regular intercourse(2-3 times per week).Serum progesterone and human chorionic gonadotropin (HCG) were tested to determine ovulation and conception. If the female subject conceived, she would be followed up with until postpartum.
2.4. Data analysis
For each sperm parameter, we calculated the median, 5th percentile, and 95th percentile. An assessment was done for the predictive value of semen analysis for the male partner among ovulatory women for conception,clinical pregnancy,and live birth.All 780 ovulatory women were divided into two groups (with a ratio of 6:4); the data from 60% of the participants were used to develop prediction models for conception, clinical pregnancy, and live birth(training sample).The data from the remaining individuals were used to verify those prediction models (verification sample).First,univariate logistic regression was used to determine the value of each independent variable, including volume, concentration, morphology, and motility. Crude odd ratios (ORs) with a 95% confidence interval (CI) were calculated.Subsequently,multivariate logistic regression was used to assess the values of all parameters together and to establish the model using the training samples. All parameters were treated as continuous variables. The discriminative capacity of the models was evaluated by calculating the area under the curve(AUC)with 95%CI in the verification sample.A model with perfect discrimination has an AUC of 1,while an AUC of 0.5 refers to a model with no discrimination.The calibration of the models was also evaluated by the Hosmer-Lemeshow test.This test assesses whether the observed rates match the probabilities in the study group or not. Models with similar calculated probabilities and observed rates are deemed to be well calibrated.
3. Results
3.1. Participants and semen analyses
Data were extracted from all 780 ovulatory couples.There were 775 semen routine reports obtained from 780 ovulatory couples,and only 408 reports showed normal sperm morphology. Among the 780 ovulatory couples,the number of couples who achieved conception, clinical pregnancy, and live birth was 320, 235, and 205,respectively[15].In regard to the semen analyses,the concentration had a median of 70.10 × 106mL-1(5th-95th percentile:17.57 × 106-305.36 × 106mL-1). The volume had a median of 3.00 mL (5th-95th percentile: 1.50-5.90 mL). The total motility had a median of 70% (5th-95th percentile: 42%-95%). The morphology had a median of 64.05% (5th-95th percentile: 5.00%-92.40%)(Table 1).

Table 1 Sperm quality among the male partners of all ovulated women.

Table 2 Results of multivariable logistic regression analysis of semen parameters for the prediction of conception among all ovulated women.
3.2. Model performance: Model for conception among ovulatory women

Fig. 1. Model for conception among ovulatory women by AUC test. The results of the test are as follows:AUC=0.62(95%CI:0.55-0.69);Youden index=0.23;model sensitivity = 56.41%; model specificity = 66.92%.
The results of the logistic multivariable regression modeling are presented in Table 2 and Fig. 1. Volume and motility were significant predictors for conception among ovulatory women in the univariate analysis. The prognostic effects of volume and motility were also significant in the multivariate analysis when other semen parameters were included. Concentration and morphology had no significant effect on conception. The ORs of the volume and motility for conception were 1.23 (95%CI: 1.01-1.51) and 33.26(95%CI:4.80-230.67),respectively.The model for conception had an AUC of 0.62 (95%CI: 0.55-0.69). The Hosmer-Lemeshow test statistic showed no poor calibration (p = 0.35).
3.3. Model performance: Model for clinical pregnancy among ovulatory women
The results of the logistic multivariable regression modeling are presented in Table 3 and Fig.2.Volume and motility were significant predictors for clinical pregnancy among ovulatory women in the univariate analysis. The prognostic effects of volume and motility were also significant in the multivariate analysis when other semen parameters were included. Concentration and morphology had no significant effect on clinical pregnancy.The ORs of the volume and motility for clinical pregnancy were 1.23 (95%CI: 1.01-1.51) and 32.98 (95%CI: 4.76-228.76), respectively. The model for clinical pregnancy had an AUC of 0.67 (95%CI: 0.61-0.73). The Hosmer-Lemeshow test statistic showed no poor calibration(p=0.15).
3.4.Model performance:Model for live birth among ovulatory women
The results of the logistic multivariable regression modeling are presented in Table 4 and Fig. 3. Volume and motility weresignificant predictors for live birth among ovulatory women in the univariate analysis. The prognostic effects of volume and motility were also significant in a multivariate analysis when other semen parameters were included. Concentration and morphology had no significant effect on live birth.The ORs of the volume and motility for live birth were 1.52(95%CI:1.22-1.91)and 22.97(95%CI:2.65-199.18), respectively. The model for live birth had an AUC of 0.57(95%CI: 0.50-0.64). The Hosmer-Lemeshow test statistic showed no poor calibration (p = 0.43).

Table 3 Results of multivariable logistic regression analysis of semen parameters for the prediction of clinical pregnancy among all ovulation women.

Fig. 2. Model for clinical pregnancy among ovulatory women by AUC test. The results of the test are as follows: AUC = 0.67 (95%CI: 0.61-0.73); Youden index = 0.28; model sensitivity = 73.96%; model specificity = 54.33%.
4. Discussion
Infertility is related to both members of a couple, so male and female factors should be considered equally. Semen analysis is usually performed in order to rule out male factors in couples with PCOS. There is limited knowledge about the predictive values of semen analysis for reproductive outcomes in women with PCOS who ovulate after ovulation induction. In this research, we evaluated the prognostic effect of semen analysis on the female partners for obstetric outcomes, through a secondary analysis based on PCOSAct. All semen analyses had been routinely accomplished before the enrolment in this study.Our study specifically evaluated the prognostic values of common sperm parameters including concentration, volume, motility, and morphology to predict conception,clinical pregnancy,and live birth for women with PCOS who ovulated after ovulation induction through clomiphene and acupuncture. We found that volume and motility did have predictive capacities for conception, clinical pregnancy, and live birth among women with PCOS who ovulated.
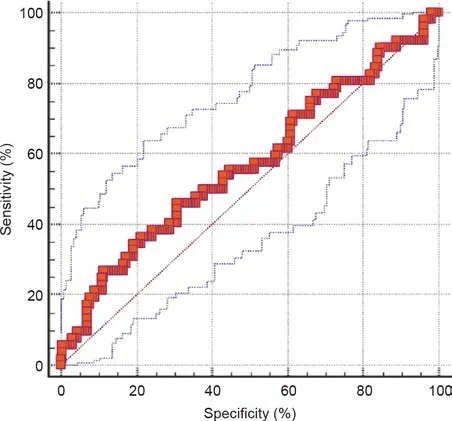
Fig.3. Model for live birth among ovulatory women by AUC test.The results of the test are as follows: AUC = 0.57 (95%CI: 0.50-0.64); Youden index = 0.15; model sensitivity = 46.15%; model specificity = 69.23%.
Prediction of obstetric outcomes through semen motility and sperm volume is controversial. Evgeni et al. [16] compared semen parameters between men with different fertility statuses and found that semen volume and motility differed significantly.Semen parameters are considered to be associated with the time to pregnancy and fecundity. Better semen motility has been positively related to a shorter time to pregnancy [17]. The threshold value of semen motility has been reported as being used as one of the predictors for fertility in couples[18].Guan et al.[19]found that there was a strong correlation between sperm motility and pregnancy, under the premise of normal reproductive functions of both men and women. Kasman et al. [20] also concluded that sperm motility was associated with pregnancy rates. These findings are consistent with our analysis that sperm motility has a positive effect on obstetric outcome.In addition,we found that sperm volume had a similar promoting effect.Liu et al. [21] found that,among infertile men receiving assisted reproduction, the semen concentration had an impact on the reproductive outcome, rather than the semen volume. We also analyzed sperm morphology and semen concentration,but neither of these parameters had significant predictive ability.

Table 4 Results of multivariable logistic regression analysis of semen parameters for the prediction of live birth among all ovulation women.
The overall rates of conception and live birth reported in similar randomized controlled trials of infertile women with PCOS[22,23]are rather low compared with those in PCOSAct.Although first-line treatment for ovulation induction is effective for PCOS,methods to improve oocyte quality might be a good point in ovulation induction for women with PCOS in the future. Our study indicates that better sperm quality (e.g., more motile sperm) could increase the chance of conception and live birth for women PCOS who has poor oocyte quality. Poor oocyte quality might cause difficulty in fertilization and implantation,even with relatively good semen quality.However, our results also showed that these prognostic values were limited. The models we built were based only on semen parameters,not on other female factors or treatment factors.When predicting conception, clinical pregnancy, and live birth, a typical model might be mainly based on female factors [24]. The limited predictive value of semen analysis indicates that the reason for the low chance of conception and live birth in such cases might be due to poor oocyte quality.
This is the first study to discuss the effect of the male partner’s semen parameters on obstetric outcomes including conception,clinical pregnancy, and live birth in women with PCOS who has a history of infertility for two years. For PCOS patients who ovulate after ovulation has been induced by clomiphene and acupuncture,we found that semen volume and sperm motility had a certain predictive power for obstetric outcome. In this secondary analysis with a large sample size,there was a high level of compliance from all the female subjects and their male partners.All couples agreed to have regular intercourse during the study period with the intent to conceive, and the subjects were in good health, without major medical disorders. The limitation of our study is that clear exclusion criteria existed for lower semen parameter references due to the design of the randomized controlled trial. The semen parameters had to meet one of these two standards: ① sperm concentration ≥15 × 106mL-1and total motility (a + b + c)≥40% or progressive motility (a + b) ≥32%; or ②total motile sperm count ≥9 million for one ejaculation. Since our population excluded some couples with semen parameters under the lower reference values, this might hamper the external validity of our model in a wider population.
5. Conclusions
This study shows that semen analysis parameters including volume and motility have potential prediction power for conception,clinical pregnancy, and live birth in women with PCOS experiencing ovulatory dysfunction,although the predictive capacity is limited. It is not recommended to use semen parameters to predict treatment outcomes for anovulatory women undergoing ovulation induction.
Acknowledgments
We are deeply grateful to the PCOSAct Steering Committee members for the recruitment work in all research sites; we also thank Wangyu Cai for the initial statistical work. This study was supported by the National Public Welfare Projects for Chinese Medicine (201107005); the National Key Research and Development Program of China (2019YFC1709500); the Project of Heilongjiang University of Chinese Medicine (2018RCQ12 and 2019BS09); the Projects of Heilongjiang Provincial Administration of Traditional Chinese medicine(ZHY2020-102);and Xuzhou Clinical Medical Team Talent Introduction Project—Academician Yixun Liu Integrated Chinese and Western medicine, Maternity and Reproductive Technology Innovation Team, and Academician Yixun Liu Workstation Project.
Compliance with ethics guidelines
Jingshu Gao, Yu Wang, Mubai Li, Mengyi Zhu, Xuekui Liu, Xinming Yang, Hongli Ma, Yijuan Cao, Lu Li, and Xiaoke Wu declare that they have no conflict of interest or financial conflicts to disclose.
- Engineering的其它文章
- PVC Formulation of Anastrepha suspensa Pheromones Suitable for Field Studies
- Handheld Ultrasound Advances Diagnosis
- Nuclear Energy Seeks Revival with Advanced Fuel Options
- Mars Helicopter Exceeds Expectations
- Toward Systemic Thinking in Managing Environmental Risks
- The Experimental Advanced Superconducting Tokamak