Penile aseptic abscess in the cavernous body at the base of the penis: a case report
Mn-Cheng Xi, Ke-Qing Yin, Yu-Sheng Wng, Ji-Wei Chen, Xio-Dong Bin, Wei-Bing Shung*
aFirst Clinical Medical College, Shanxi Medical University, Taiyuan, Shanxi 030001, China
bDepartment of Urology, First Hospital of Shanxi Medical University, Taiyuan, Shanxi 030001, China
Abstract: We report a case of aseptic abscess in the cavernous body at the base of the penis. In our clinical observation, the patient underwent puncture and drainage of the corpus cavernosum abscess, followed by surgical resection of the abscess wall, with the incisions closed layer by layer with primary suture. In addition, we paid attention to strengthening the postoperative management by using elastic bandages to wrap the penis intermittently to prevent edema; the incision would not be covered with dressings from the third day after the operation, so as to keep the incision site dry in an open way. During the period of indwelling of the catheter after the operation, we noticed the care of the external orifice of the urethra to reduce the occurrence of catheter-related infections. Finally, the patient was diagnosed with a penile aseptic abscess in the cavernous body at the base of the penis. The patient recovered well after surgery and was discharged 1 week later. At 1.5 years after the operation, the shape of the penis returned to normal, and the erectile function was normal. It was seen that good nursing concept is of great help for prognosis, which could avoid infection and edema, and is conducive to wound healing.
Keywords: penis · aseptic abscess · puncture and drainage · primary suture · nursing
1. Introduction
Penile abscess is a rare genitourinary disease, which was first reported by Niedrach et al. in 1989.1The pathogens usually include Neisseria gonorrhoeae, Escherichia coli, Staphylococcus aureus, Streptococcus, or mixed bacteria.1-4Treatment of penile abscess mainly includes surgical incision and drainage, puncture and drainage, and antibiotic treatment.3,5-8In the present clinical observation, we report a case of aseptic abscess in the cavernous body at the base of the penis. The patient underwent puncture and drainage of the corpus cavernosum abscess, followed by surgical resection of the abscess wall, with the incisions closed layer by layer with primary suture.
2. Case report
A 65-year-old male patient was admitted to the hospital due to the appearance of a mass at the base of the penis, which was accompanied by dysuria and a thin urine stream. The patient denied any history of penile injection or trauma. Physical examination showed that the mass was located at the base of the penis. The computed tomography (CT) scan and spiral CT 3-D image revealed the presence of a cystic mass measuring 4.9 × 3.5 cm in the cavernous body at the base of the penis, which contained a few solid components. The plain CT value was about 13-30 HU (Figures 1 and 2). Both T1-weighted and T2-weighted images confirmed the presence of a round-like cystic mass in the cavernous body, which was surrounded by a clear cystic wall (Figures 3 and 4), and the mass exhibited high signal intensity in diffusion-weighted imaging (DWI) scan (Figure 5), with a clear lesion boundary and a size measuring about 4.2 cm × 4.6 cm × 4.7 cm. The patient’s HIV and syphilis tests were negative, and tumor marker levels were within the normal range.
The patient underwent puncture and drainage of the corpus cavernosum abscess, followed by surgical resection of the abscess wall. During the surgical procedure, the skin on the penis and the subcutaneous fascia were resected layer by layer, and a cystic solid mass with a size measuring about 4.9 cm × 3.5 cm was found under the white membrane. About 40 ml of reddish- brown purulent liquid was aspirated with a syringe, which was confirmed as the lesion and submitted to the laboratory for analysis of bacterial culture (Figure 6). After the abscess cavity was completely opened (Figure 7), the abscess wall was removed and sent for pathological examination. After careful washing with iodophor and saline, a 10-cm scar was found on the right side of the penis; the scar was situated opposite to the cavity in the corpus cavernosum on the opposite side of the tunica albuginea, with no obvious damage to the urethra. The scar was formed possibly due to penile trauma which may be concealed by the patient. Finally, the incisions were closed layer by layer with primary suture. In addition, we strengthened the postoperative management, using elastic bandages to wrap the penis intermittently to prevent edema; the incision would not be covered with dressings from the third day after the operation, so as to keep the incision site dry in an open way. During the period of indwelling of the catheter after the operation, we paid attention to the care of the external orifice of the urethra to reduce the occurrence of catheter-related infections.
Pathological examination showed that suppurative inflammation was accompanied by necrosis and abscess formation. A few inflammatory cells which were not cancer cells were observed on the abscess wall (Figure 8). In addition, no bacteria were found in the pus culture. Finally, the patient was diagnosed with a penile aseptic abscess in the cavernous body at the base of the penis. Ten months after the operation, the patient recovered well without erectile dysfunction. The patient recovered well after surgery and was discharged 1 week later. At 1.5 years after the operation, the shape of the penis returned to normal, and the erectile function was normal.

Figure 1. CT scan of a mass of 4.9 × 3.5 cm found in the cavernous body of the penis root.
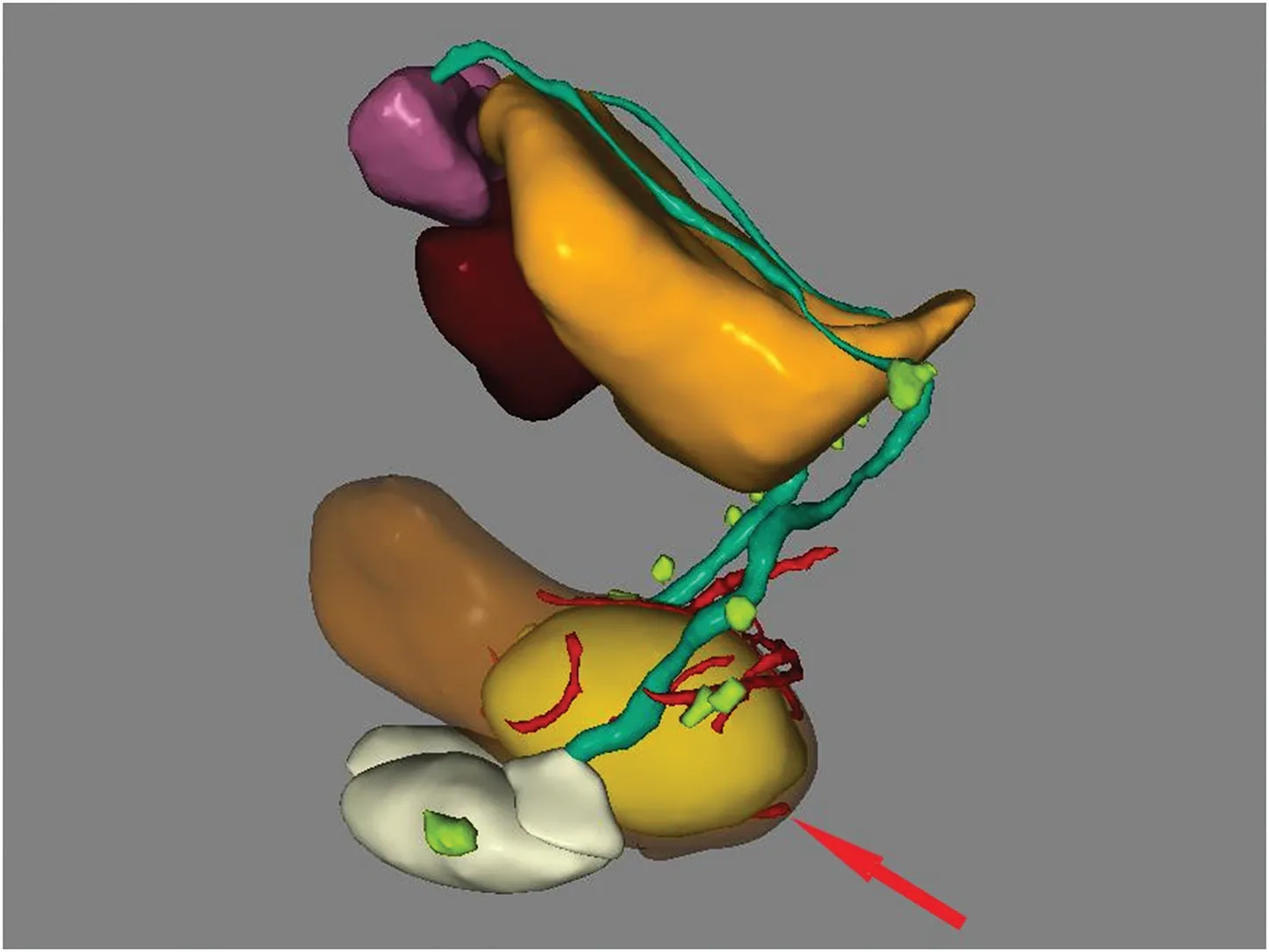
Figure 2. Spiral CT 3-D image of a mass of 4.9 × 3.5 cm found in the cavernous body of the penis root.
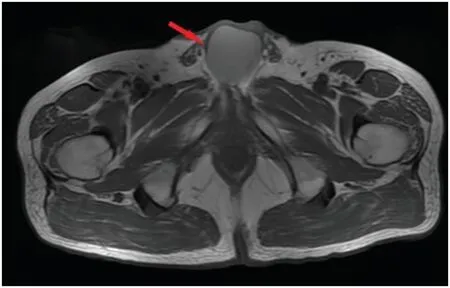
Figure 3. T1-weighted images showing a round-like abscess in the cavernous body of the penis root.
3. Discussion
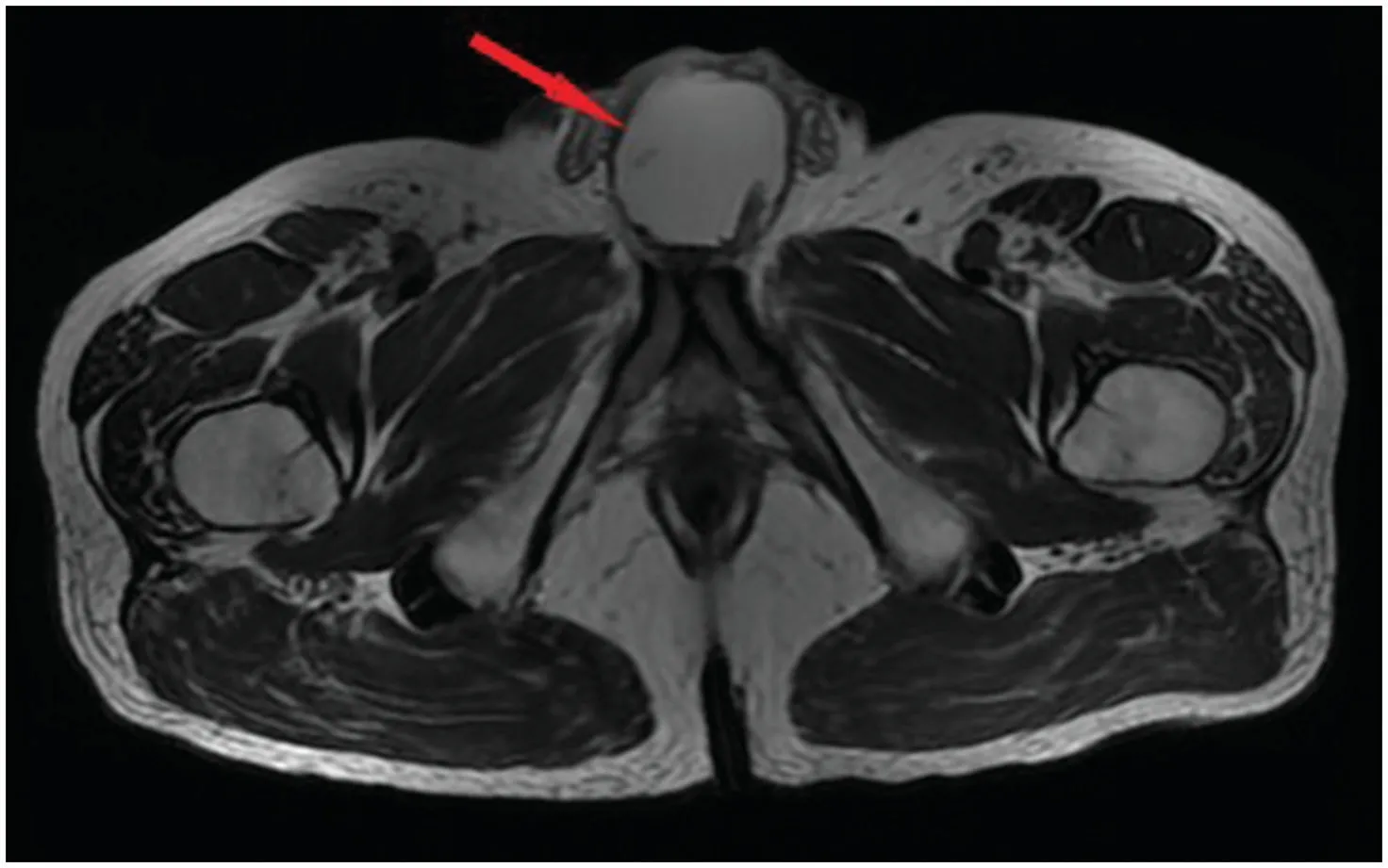
Figure 4. T2-weighted images showing a round-like abscess in the cavernous body of the penis root.
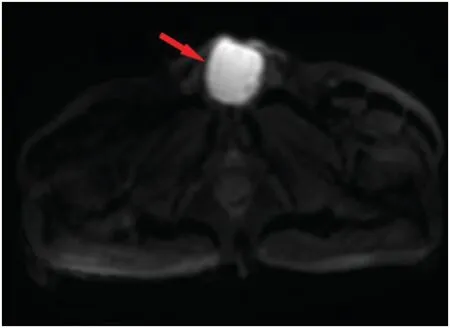
Figure 5. DWI scan showing a round-like cystic mass with high signal intensity in the cavernous body of the penis root.
The most common symptom of penile abscess is localized penile swelling and painful erections,4but the symptoms in this case included poor urination and a thin urine stream. Penile abscess often occurs in the cavernous body, its head, and subcutaneous fascia of the penis, and it is usually caused by a variety of pathogenic bacteria, including N. gonorrhoeae, E. coli, S. aureus, Streptococcus, or mixed bacteria.1-4The formation of a penile abscess may be related to penile trauma, history of urological operation, injection, and disseminated infection.9-11In this case, penile aseptic abscess may be caused by localized bleeding and hematoma from incomplete rupture of the penile tunica albuginea.
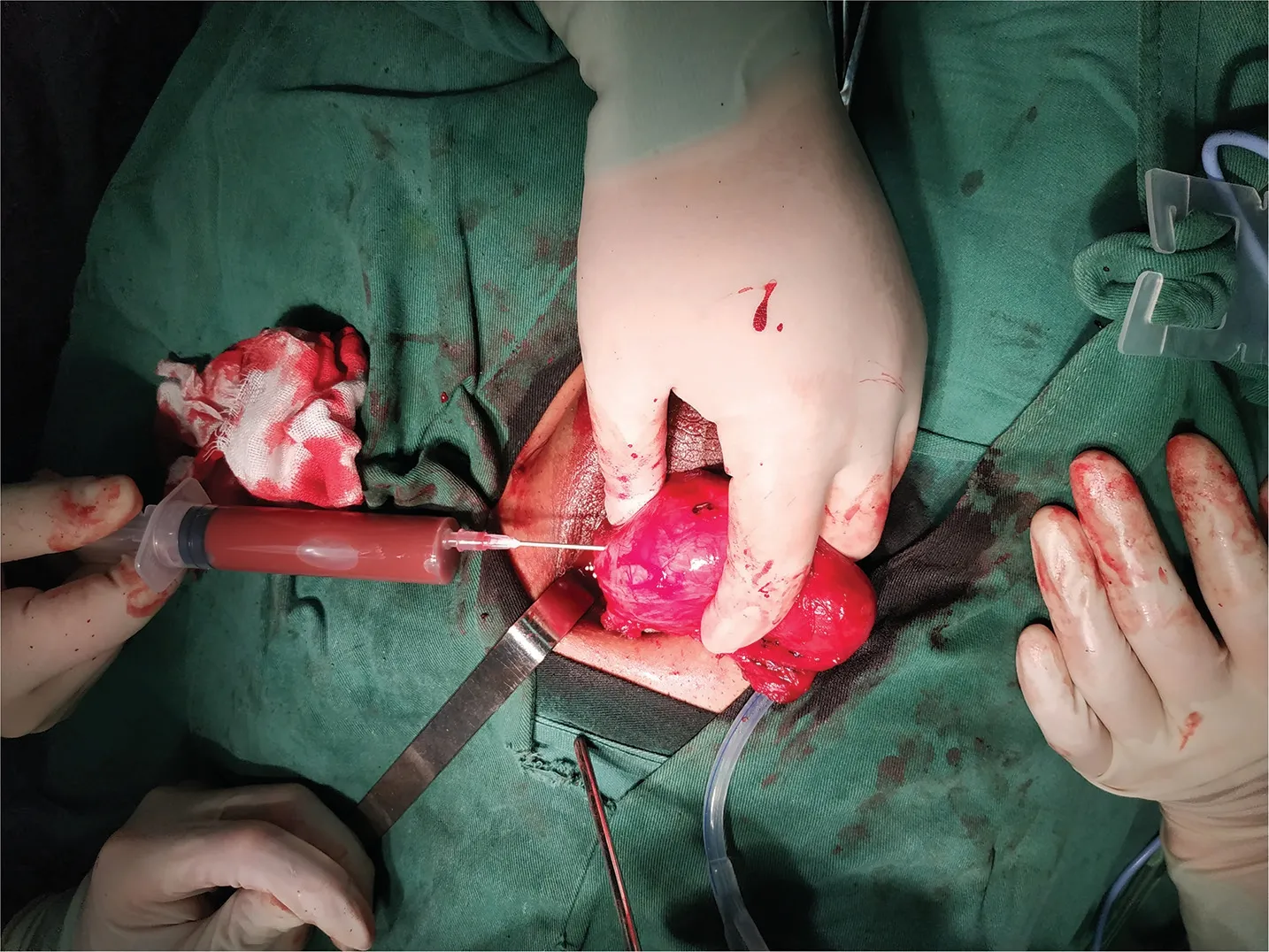
Figure 6. Aspiration of about 40ml of reddish brown purulent fluid with a syringe.

Figure 7. Abscess cavity completely opened during surgery.
Although ultrasound examination is an economical, convenient, and effective method for the diagnosis of penile abscess,6,12CT and magnetic resonance imaging (MRI) can easily identify cavernous abscess around the root of penile tissue and better reflect its range and relationship with adjacent tissues.4,11MRI, especially DWI, has been considered as a powerful tool for the diagnosis of penile abscess.11Nevertheless, the final diagnosis has to be made based on pathological observation and bacterial culture.

Figure 8. Histopathological examination showing the presence of a few inflammatory cells on the abscess wall.
Treatment of penile abscess mainly includes incision and drainage, puncture and drainage, and antibiotic treatment.3,5-8If the patients experience severe postoperative erectile dysfunction, they need to be further treated with penile prosthesis implantation.13,14Some patients with recurrent penile abscess or pain may have to undergo penectomy.15-17In the present case, not only was the patient treated with puncture drainage, but also the abscess wall was removed and then the gap was closed layer by layer with primary suture. In addition, we took care to strengthen the postoperative management, using elastic bandages to wrap the penis intermittently to prevent edema; the incision would not be covered with dressings from the third day after the operation, so as to keep the incision site dry in an open way. During the period of indwelling of the catheter after the operation, we paid attention to the care of the external orifice of the urethra to reduce the occurrence of catheterrelated infections. Although it was reported that patients who received open surgical drainage are more likely to have complications, including poor erectile function, impaired sexual activity, and secondary fibrosis,6,14,18,19this patient recovered well from surgery and had a normal erectile function and appearance of the penis, which may be related to a good nursing concept.
4. Conclusions
As a rare disease, the penile aseptic abscess can be diagnosed by a combination of ultrasound, CT, MRI, pathological examination, and bacterial culture. This disease can be effectively treated with surgery for the aspiration of purulent substances using a syringe, followed by surgical resection of the abscess wall. The incisions can also be closed layer by layer with primary suture. During the surgical procedure, rapid discharge of purulent substances is the main therapeutic target. In addition, good nursing concept is of great help for prognosis; this can avoid infection and edema, and is conducive to wound healing. The prognosis of the patient was satisfactory.
Ethical approval
Ethical issues are not involved in this report.
Conflicts of interest
All the contributing authors declare that no conflicts of interest exist.
- Frontiers of Nursing的其它文章
- Factors affecting repositioning policy compliance: an integrative review
- Development of student simulated patient training and evaluation indicators in a high-fidelity nursing simulation: a Delphi consensus study†
- Effects of mother–child interaction on school adaptation of children according to maternal depression
- Correlation among academic self-efficacy, professional identity, and professional attitude of higher vocational nursing students†
- Gender and managerial competence: a comparison of male and female first-line nurse managers in Indonesia
- Attitude and practice toward physical restraint among psychiatric nurses in Guangdong, China: a cross-sectional survey†