Esophageal superficial adenosquamous carcinoma resected by endoscopic submucosal dissection: A rare case report
Guan-Yi Liu, Ji-Xin Zhang, Long Rong, Wei-Dong Nian, Bi-Xiao Nian, Yuan Tian
Guan-Yi Liu, Long Rong, Wei-Dong Nian, Bi-Xiao Nian, Yuan Tian, Endoscopy Center, Peking University First Hospital, Beijing 100032, China
Ji-Xin Zhang, Department of Pathology, Peking University First Hospital, Beijing 100032,China
Abstract BACKGROUND Adenosquamous carcinoma (ASC), which is comprised of squamous cell carcinoma (SCC) and adenocarcinoma elements, is a rare histological type of esophageal carcinoma. Few reports have focused on the endoscopic findings and the effectiveness of the endoscopic treatment of early ASC.CASE SUMMARY A 77-year-old man underwent esophagogastroduodenoscopy for heartburn. A flat lesion with an uneven and slightly elevated central portion was found in the distal esophagus. Magnifying endoscopy with narrow-band imaging showed a well-demarcated brownish area with dendritically branched abnormal vessels and highly irregular intrapapillary capillary loops. A histopathological diagnosis of SCC was obtained by endoscopic biopsy. Endoscopic ultrasonography revealed a hypoechoic mass confined to the mucosa layer. The lesion was suspected to be SCC with invasion into the muscularis mucosa. The lesion was resected en bloc by endoscopic submucosal dissection and histologically diagnosed as esophageal ASC limited within the muscularis mucosa, which was completely resected without lymphovascular or neural invasion. The SCC element was the predominant element. The adenocarcinoma element formed ductal and nested structures distributed in a focal pattern. The patient underwent only endoscopic submucosal dissection and has been under annual endoscopic and radiographic surveillance for 3 years without recurrence.CONCLUSION For early ASC confined within the mucosal layer, complete endoscopic resection might also be a curative treatment.
Key Words: Adenosquamous carcinoma; Esophageal neoplasms; Endoscopy; Narrow band imaging; Endoscopic submucosal dissection; Case report
INTRODUCTION
Squamous cell carcinoma (SCC) and adenocarcinoma (AC) are the two major histological types of esophageal cancer in both eastern and western countries.Adenosquamous carcinoma (ASC), which comprises both SCC and AC elements, is a rare histological type of esophageal carcinoma throughout the world with reported incidence rates ranging from 0.37% to 1.00%[1]. The literature on ASC is scare; mostly consisting of reports about advanced ASC cases managed by surgical treatment[2,3].Few reports have focused on the endoscopic findings and the effectiveness of endoscopic treatment of early ASC. In this article, we report the endoscopic findings from a case of superficial ASC in the esophagus that was successfully treated by endoscopic submucosal dissection (ESD).
CASE PRESENTATION
Chief complaints
A 77-year-old man underwent esophagogastroduodenoscopy for heartburn and retrosternal discomfort.
History of present illness
There was no complaint of abdominal pain or weight loss.
History of past illness
His previous history included hypertension that was well controlled with medication.
Personal and family history
There was no significant personal or family history.
Physical examination
During physical examination, no specific physical signs were found.
Laboratory examinations
Laboratory assessments including the evaluation of tumor markers revealed no abnormalities.
Imaging examinations
During esophagogastroduodenoscopy, a superficial lesion was found in the distal esophagus. White light endoscopy revealed a flat lesion of approximately 2.5 cm × 1.5 cm in size at a distance of 36-38 cm from the incisors, 2 cm away from the esophagogastric junction and slight reflux esophagitis (Los Angeles classification grade A)without Barrett’s esophagus. The central part of the lesion was uneven and slightly elevated. The lesion represented slight reddening of the mucosa with a coarse surface.Most of the lesion was covered by a scattered white membranous substance and mucous that was difficult to remove with water flow, and a normal vascular network could not be seen. Narrow-band imaging (NBI) showed a well-demarcated brownish area with background coloration (Figure 1). Magnifying endoscopy with NBI (MENBI) showed that under the membranous substance there were irregularly and dendritically branched abnormal vessels without loop formations, classified as type B2 according to the classification of the Japan Esophagus Society (JES classification)[4].Additionally, intrapapillary capillary loops with morphological irregularities,including dilation, tortuous, and caliber changes, were observed in the peripheral area,classified as type B1 (Figure 2). Iodine staining (1%) allowed the visualization of the lesion as an unstained area with a comparatively clear boundary, and pink-color sign could be seen (Figure 1). A histopathological diagnosis of SCC was obtained by an endoscopic biopsy. Endoscopic ultrasonography (EUS) revealed a hypoechoic mass confined to the mucosa layer, which did not seem to completely disrupt the muscularis mucosa, and the submucosa layer was intact (Figure 2). Moreover,computed tomography (CT) scanning was performed to rule out lymph node or distant metastasis.
Primary diagnosis
Based on the findings on ME-NBI, the histopathological results of biopsy and the results of EUS and CT scanning, we considered the lesion to be superficial SCC of the lower esophagus with invasion into the muscularis mucosa.
FINAL DIAGNOSIS
Histopathological examination showed that the lesion consisted of both SCC and AC components coexisting in the mucosal layer. The SCC element was the predominant element, and the AC element formed ductal and nested structures distributed in a focal pattern among the SCC elements. Part of the lesion was covered by dyskeratotic squamous cells. Dilated and tortuous vessels were observed around and within the ductal-structure-forming cancer cell nests (Figure 3). Immunohistochemically, the ductal structure was positive for CDX2, which is a marker of AC with an intestinal phenotype, and negative for P40 (Figure 4). Histologically, the lesion was confirmed as ASC, consisting of a well-differentiated SCC element (80%) and a well-differentiated AC element (20%) limited within the muscularis mucosa. It was completely resected[4].There was no lymphovascular or neural invasion of cancer cells, and both the horizontal and vertical margins were negative.
TREATMENT
The patient was then admitted to our hospital for further treatment. For a precise histological diagnosis, the lesion was resecteden blocby ESD.
OUTCOME AND FOLLOW-UP
The lesion was considered to be curatively resected and the patient has received annual esophagogastroduodenoscopy and CT scanning surveillance. To date, there has been no recurrence for 3 years.
DISCUSSION
Esophageal ASC is a rare histopathological type of esophageal carcinoma with comparatively aggressive biological behavior[5]. Early detection and diagnosis are important for improving the prognosis of ASC. However, there are few reports concerning the endoscopic findings of early ASC and the effectiveness of endoscopic resection (ER). In this report, we first describe a superficial esophageal ASC, which was confined to the muscularis mucosa and successfully treated by ESD alone. To our knowledge, this is the earliest ASC reported to date.
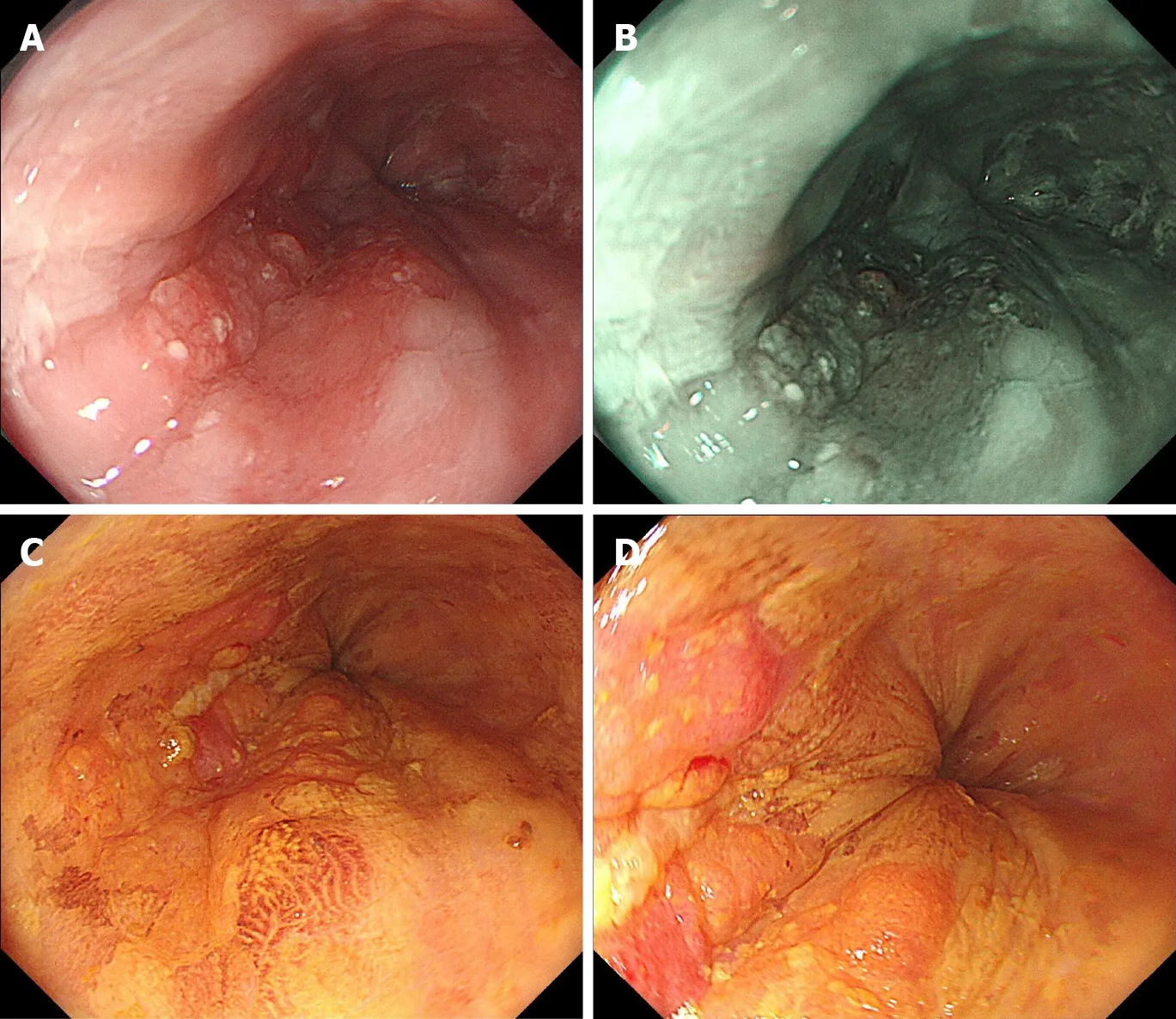
Figure 1 Esophagogastroduodenoscopy revealing a superficial lesion in the distal esophagus. A: Upon white light endoscopy, a flat lesion of approximately 2.5 cm × 1.5 cm in size was found, with the central part uneven and slightly elevated. The lesion presented slight reddening of the mucosa with a coarse surface; B: Narrow-band imaging showed a well-demarcated brownish area of background coloration; C and D: Iodine staining (1%) visualized the lesion as an unstained area with a comparatively clear boundary, and pink color sign could be seen.
Upon white light endoscopy, ASC is reported to be mostly visualized as submucosal tumor (SMT)-like in appearance or as a flat or slightly elevated lesion. In SMT-like cases, ASC can also mimic other non-SCC types of malignant esophageal epithelial neoplasms, such as basaloid squamous carcinoma or other benign SMTs. The SMT-like appearance results from the invasive growth pattern of ASC because the squamous cell component always dominates in the mucosa, and the AC component is mainly found in the deeper parts of the tumor[1]. In superficial cases, ASC is often indistinguishable from SCC macroscopically. In our case, the SCC and AC components coexisted in the mucosal layer, which was thought to be the cause of the flat but non-SMT-like appearance.
Upon NBI, the lesion showed a well-demarcated brownish area similar to typical SCC. However, the membranous substance and mucus on the surface partly interfered with the observation of the microvascular pattern in ME-NBI. Histopathological images demonstrated that part of the lesion was covered by dyskeratotic squamous cells, which may account for the blurring of microvascular pattern. According to the work of Takeuchiet al[6], the mixed type of type B1 and the small area of B2 vessels suggested that the lesion was SCC with invasion into the muscularis mucosa with deep invasion into the submucosa being less likely. The final pathological result confirmed the invasion depth as the muscularis mucosa, which was in perfect accordance with our presumption. In immunohistochemical testing, the area of the lesion showed a double layer of muscularis mucosa, and the tumor invaded the superficial muscularis mucosa. Considering the location in the distal esophagus and the patient’s complaint of heartburn and retrosternal discomfort as well as the endoscopic finding of mild reflux esophagitis, the double layer muscularis mucosa could possibly be explained by the anatomic closeness to the esophagogastric junction and the presence of chronic persistent inflammation. Arimaet al[7]reported type R vessels as a characteristic vascular pattern of poorly differentiated SCC or non-SCC types of malignant esophageal epithelial neoplasms due to the infiltrative growth pattern of cancer cells (INF c). In our case, no type R vessels but some type B1 and B2 vessels were observed in the lesion. This may also be explained by its histopathological character that the coexistence of predominant SCC and focal AC components in the mucosal layer and the pushing growth pattern of cancer cells (INF a),demonstrating ME-NBI features similar to SCC.

Figure 2 The lesion upon narrow-band imaging. A: The lesion upon narrow-band imaging; B: Magnified view with magnifying endoscopy with narrow-band imaging of the yellow square in (A) revealing that under the membranous substance and mucous there were intrapapillary capillary loops with morphological irregularity, classified as type B1; C: Magnified view with magnifying endoscopy with narrow-band imaging of the blue square in (A), revealing that in the slightly elevated central part of lesion, irregularly and dendritically branched abnormal vessels without loop formation were observed, classified as type B2; D: Endoscopic ultrasonography revealing a hypoechoic mass (white arrows) confined to the mucosa layer, which did not seem to disrupt the muscularis mucosa completely, and the submucosa layer was intact.
ASC has been shown to be subject to low preoperative diagnostic accuracy with a reported misdiagnosis rate of 61.1%-100%, mostly being misdiagnosed as SCC[1]. ASC is often diagnosed after resected specimens from surgery are examined[1], as in the present case. One reason for this discrepancy may be that the SCC component is located in the mucosa while the AC component is mainly found in deeper areas of the tumor, which are difficult to reachviacommon biopsy. On the other hand, the AC component located in the superficial layer may be distributed in a focal pattern,meaning that the collection of a precise specimen for diagnosis is not always possible.A combination of ME-NBI findings, EUS and deeper biopsies with greater tissue sampling might improve the diagnostic accuracy.
The treatment strategy for ASC is still controversial. Most advanced ASC cases are managed with surgical treatment and/or radiation therapy and chemotherapy[1]. The effectiveness of ER for ASC is yet unknown. In an ASC case presented by Endoet al[8]with an invasion depth of SM2 (1100 μm), additional chemoradiotherapy was administered after ER, and the patient survived 9 years without recurrence. The patient in our case received only ESD treatment and has been under annual endoscopic surveillance and CT for 3 years with no recurrence found to date. This suggests that for very early ASC confined within the mucosal layer, complete ER might also be a curative and sufficient treatment, as in SCC. The patient has been grateful for the avoidance of esophagectomy and the maintenance of life quality.
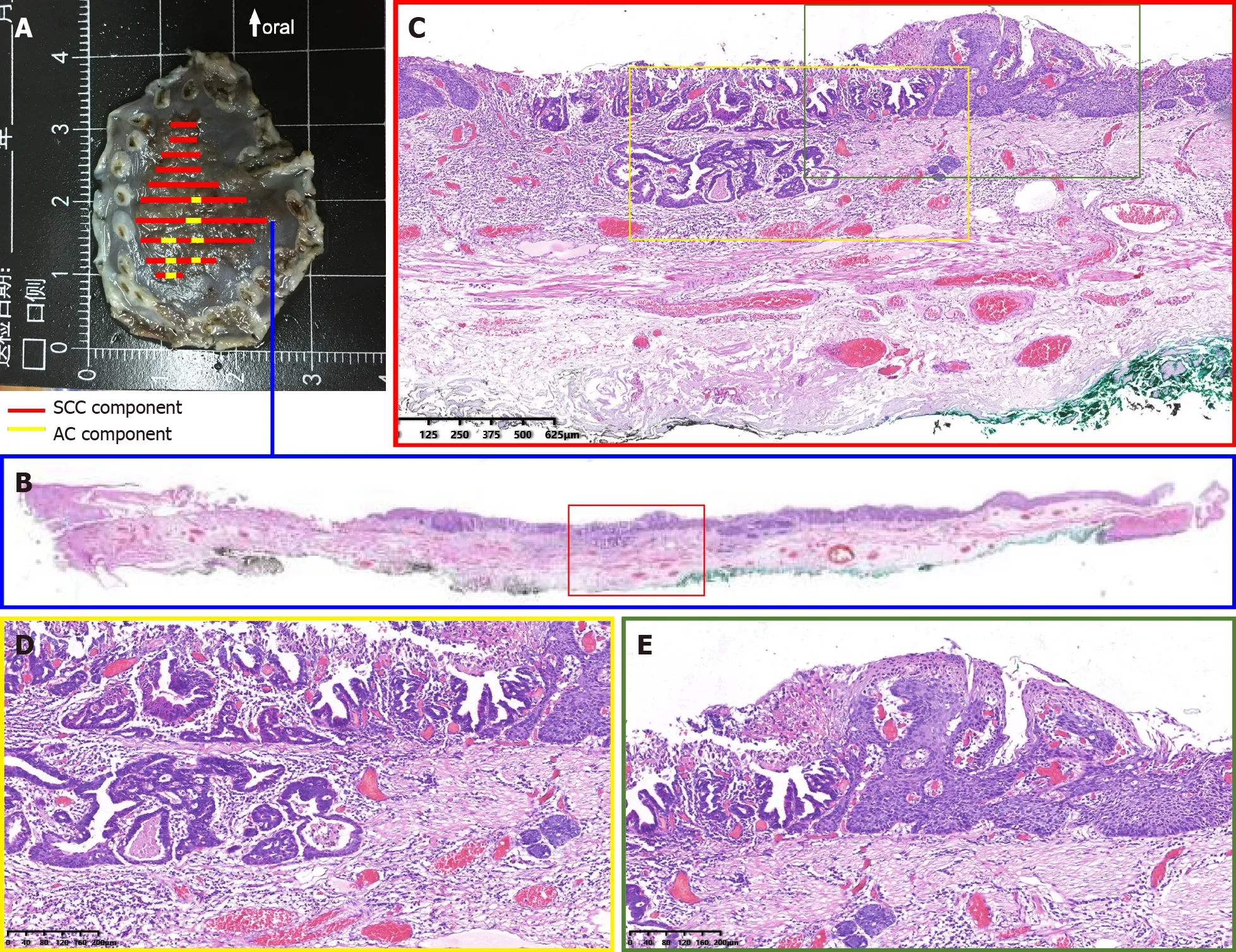
Figure 3 Dilated and tortuous vessels were observed around and within the ductal-structure-forming cancer cell nests. A: Specimen resected by endoscopic submucosal dissection; B: Histological view of the resected lesion revealed that the squamous cell carcinoma element was the predominant element,and the adenocarcinoma element was distributed in a focal pattern among the squamous cell carcinoma element; C-E: High-power view revealed invasive carcinoma forming ductal structures distributed among squamous cell carcinoma. Part of the lesion was covered by dyskeratotic squamous cells.
CONCLUSION
In conclusion, we report a case of very early esophageal ASC confined to the muscularis mucosa, which was successfully treated by ESD alone. The endoscopic findings of early ASC can be indistinguishable from those of early SSC, especially when the SCC element and AC element coexist and are distributed separately in the mucosal layer. A combination of ME-NBI, EUS and deeper biopsy might improve preoperative diagnostic accuracy. For ASC confined within the mucosal layer without lymph node and distant metastasis, complete ER alone might also be a sufficient treatment.Additional studies and cases are needed to further assess the efficacy of ER therapy for superficial esophageal ASC.

Figure 4 Immunohistological findings of the lesion. A and B: The ductal structures were positive for CDX2 and negative for P40; C: The muscularis mucosa was positive for desmin, confirming that the deepest part of the carcinoma was limited within the muscularis mucosa; D: CD31 staining revealed the distribution of vessels, showing dilated and tortuous vessels around and within the ductal-structure-forming cancer cell nests.
ACKNOWLEDGEMENTS
We gratefully acknowledge the great support from the Department of Pathology of Peking University First Hospital in the cooperative effort aimed at the continuous improvement of diagnostic accuracy in early gastrointestinal cancer.
 World Journal of Clinical Cases2021年6期
World Journal of Clinical Cases2021年6期
- World Journal of Clinical Cases的其它文章
- Interactive platform for peer review: A proposal to improve the current peer review system
- Animal models of cathartic colon
- New indicators in evaluation of hemolysis, elevated liver enzymes,and low platelet syndrome: A case-control study
- Analysis of hospitalization costs related to fall injuries in elderly patients
- Effect of alprostadil in the treatment of intensive care unit patients with acute renal injury
- Etomidate vs propofol in coronary heart disease patients undergoing major noncardiac surgery: A randomized clinical trial
