The effect of digital health technologies on managing symptoms across pediatric cancer continuum:A systematic review
Li Chng ,Mingxia Duan ,Xiaorong Mao ,Youhong G ,Yanqing Wang ,Haiying Huang
a School of Nursing,Fudan University,Shanghai,China
b Anhui Provincial Children’s Hospital,Hefei,Anhui,China
c Sichuan Academy of Medical Science & Sichuan Provincial People’s Hospital,Chengdu,Sichuan,China
d Children’s Hospital of Fudan University,Shanghai,China
e Children’s Hospital of Zhejiang University School of Medicine,Hangzhou,Zhejiang,China
f Guangzhou Women and Children’s Medical Center,Guangzhou,Guangdong,China
Keywords:Child Neoplasms Palliative care Symptom assessment Telemedicine Wearable electronic devices
ABSTRACT Objective:Pediatric cancer patients endure multiple symptoms during treatment and also in survivorship.Digital health technologies provide an innovative way to support their symptom management.This review aimed to examine the effect of digital health technologies on managing symptoms among across pediatric cancer continuum.Methods:A systematic literature search of six English and three Chinese electronic databases was combined with hand searching,to identify eligible research studies from database establishment to November 30,2019.Two reviewers carried out data selection,data extraction,and quality appraisal independently.A narrative approach was taken to summarize data.Results:Four randomized control trials,two quasi-experiments,and five one group pre-posttest designed studies,were included in the review with a total of 425 participants.The methodological quality of the studies was generally fair.Seven symptoms (anxiety,depression,pain,anger,fatigue,fear,distress) and seven digital health technologies (visual reality,website,humanoid robot,app,wearable devices,short messages and videoconference) were reported in the included studies.Conclusions:Current evidence supports the effect of digital health technologies is generally mixed and inconclusive.There is a trend of positive effects found in the interventions that feature digital health technologies’interactive function.This review highlights the need for further investigation with rigorous research designs and the consideration of influencing factors from the symptoms,participants,and context levels to inform a better digital health implementation.
What is known?
·Pediatric cancer patients endure multiple symptoms during treatment and also in survivorship.Recent evidence has demonstrated the feasibility and acceptability of some digital health interventions.
What is new?
·Current evidence supports the effect of digital health technologies is generally mixed and inconclusive.There is a trend of positive effects found in the interventions that feature digital health technologies’ interactive function.
·When examining the effect,there is a need to take into consideration about the factors from the symptoms,participants,and context levels.
1.Introduction
Each year,approximately 300,000 children were diagnosed with cancer worldwide [1].The advancement of treatments for childhood cancers has significantly improved the survival rate.However,these aggressive treatments for childhood cancers have also induced symptom burdens and suffering for pediatric cancer patients.Studies has proved that pediatric cancer patients can report up to 15 distressing and disruptive symptoms,with anxiety,depression,pain,and fatigue the most frequently cited[2,3].These multiple interrelated occurring symptoms directly affect patients’ability to function in multiple domains and their overall quality of life.It is noted that some of the symptoms may prolong to survivorship.For instance,fatigue is not only a distressing symptom frequently reported by children undergoing cancer treatment; but also is one of the most common complaints of survivors of childhood cancer[4].In the meantime,those childhood cancer survivors are also faced with an increased risk of late effects from treatment(e.g.accumulated toxicity from previous chemotherapy),along with cancer-or-treatment related long-term multisystem health conditions [5].Moreover,for pediatric cancer patients who grow into adolescents or young adults,immerging autonomy may influence their health behaviors,which may bring new physical or psychological symptoms that impact the quality of life [6].In light of the disease,treatment and developmental influencing factors discussed above,it will be difficult to separate the multiple impacts and complex healthcare needs across the pediatric cancer continuum [7].Evidence on managing symptoms across the pediatric cancer continuum is therefore warranted.
Among all the symptom management interventions,digital health technology has become an emerging hot topic.Digital health technology is broadly defined as the use of technology in the promotion,prevention,treatment,and maintenance of health and health care [8].It includes mobile health (mHealth),health information technology (IT),text messaging,apps,wearable devices,telehealth and telemedicine,digital gaming,virtual reality,robotics,online support groups and social networks [8-10].In the past decade,digital health technologies have risen in prominence[10,11]and become a promising and innovative facilitator that expands the scope of health care [12,13].Substantial evidence has proved that digital health technologies can overcome the barriers of geographical and time-related constraints and exemplified their strength in various ways,e.g.,assisting health information delivery,patient-clinician communications,social networking,real-time health indicator monitoring,and automated clinical intervention[14,15].
Regarded as“digital native”,the young generations are exposed every day to a technology-driven environment with digital devices[16].Age-appropriate co-design and cognitive interviews have been widely used to develop digital health technologies for children of all ages [17,18].In the field of pediatric oncology,digital health technology is pointed out as one of the promising strategies that support patients and survivors to manage the challenges associated with their disease and treatment [15].Currently,synthesized evidence has demonstrated the feasibility and acceptability of digital health interventions on this particular population[8,10].McCann’s systematic review of 38 studies assessed the quality,feasibility,and efficacy of existing digital health interventions that support adolescents and young adults with cancer.The authors summarized the function of most frequently used healthcare technologies and pointed out that symptom management was a major focus.However,they concluded that the technologies “have yet to be evaluated at scale”.In another systematic review led by Ramsey,the authors appraised the current scientific evidence on electronic health (eHealth) and mobile health(mHealth) interventions in study participants from child to young adult.The authors concluded from the twenty-one studies met the inclusion criteria that although feasibility and acceptability were established for digital health technologies.Evidence of efficacy for interventions targeting emotional distress,health behaviors,health outcomes,and neurocognitive functioning was still mixed.Both of the systematic reviews mentioned the important role of digital health technologies in symptom management.However,neither of them further analyzed the evidence from the symptom perspectives.There is a lack of synthesized evidence specifically on the effect of digital health technologies on managing symptoms across the continuum of childhood cancer treatment and survivorship.This gap will prevent the understanding of symptom management function and further develop digital health intervention strategies that support these pediatric cancer patients and survivors to cope with their symptoms.
2.Methods
The purpose of this review was to examine the effect of digital health technologies on managing symptoms among across pediatric cancer continuum.This review followed the PRISMA(Preferred Reporting Items for Systematic Reviews and Meta-Analyses) recommendation [19].
2.1.Eligibility criteria
Participants included children,adolescents and young adults with cancer (0-39 years old),and young adult survivors of childhood cancer were defined as mean age 21 years or younger at the time of diagnosis; mean age 39 years or younger at the time of intervention [11].
The intervention incorporated using digital health technology as the component.In this study,“digital health technology” included but not limited to mobile health (mHealth),health information technology(IT),text messaging,apps,wearable devices,telehealth and telemedicine,digital gaming,virtual reality,robotics,online support groups and social networks [8-10].The comparator comprised of studies in which the comparison group did not receive intervention from using digital health technology.
The studies must include at least one outcome related to the patients’ symptoms.“Symptoms” were defined as clinical manifestations that can be either objective when observed by a physician,or subjective when perceived by the pediatric cancer patients or survivors.
The designs included randomized controlled trials(RCTs),quasiexperimental studies,pre-posttests,interrupted time series designed studies.
Exclusion criteria are studies that 1) had insufficient detail on the target population,2) had a vague description of the digital health technology of intervention,and 3)did not examine patients’symptoms.
2.2.Literature search
The first two authors performed a thorough database searching in six English databases (Cochrane Library,Joanna Briggs Institute Library,PubMed,CINAHL,EMBASE,and Web of Science)and three Chinese databases (Wanfang Database,National Knowledge Infrastructure (CNKI) and SinoMed) from the databases’ inception to November 30,2019.Additional records were identified through hand searching.A combination of both keywords and indexed terms (e.g.,MeSH) was applied in each database using BOOLEAN terms.Search strategies for each database were listed in Appendix A.This literature search was conducted from December 15,2019 to July 1,2020.
2.3.Study selection
Two reviewers independently identified the titles and abstracts of studies by the search strategies.Potentially eligible studies were evaluated at full text according to the inclusion and exclusion criteria,and the final inclusion of studies into the systematic review was by agreement of all the authors.
2.4.Data extraction
Data were extracted with a report table,including first author,year,country,study design,sample,symptom and measurement,intervention,and symptom(s) related outcomes (Table 1).Two reviewers independently verified all of the extracted content.
2.5.Quality assessment of included studies
The first two authors assessed the included studies’ quality independently according to a 27-item Checklist for Both Randomized and Nonrandomized Studies [19].This checklist includes five subscales:reporting,external validity,bias,internal validity,and statistical power.The maximum total score in this assessment was 28.Studies scoring 9 or less(<33%)were considered of low quality.
2.6.Data analysis
A narrative synthesis was performed given the heterogeneous nature of the interventions involved and the outcome measures investigated across selected studies.For each symptom,its relevant digital health technology interventions,mode of delivery,and effects were also summarized.
3.Results
3.1.Study characteristics
The search strategy identified a total of 1,190 articles.After removing duplicates,the remaining 1,103 articles were screened by titles and abstracts,resulting in 67 articles remaining.Of the retrieved full-text publications,56 were excluded,leaving 11 papers included in this review.Fig.1 illustrates the flow diagram of studies identification and selection.Table 1 shows the characteristics of the included publications.Appendix B displays all the studies that were excluded from the full-text assessment and why each was excluded.
Most of the studies were conducted in the United States(n=8),one in Canada,one in Germany,and one in China.Of the eleven included studies,four were randomized control trials[20-23],two quasi-experiment designs[24,25],and five one group pre-posttests[26-30].The time intervals for measurement varied from 1 week to 12 months.
In terms of the participants’characteristics,their ages,diagnosis and treatment stages varied across the studies.Specifically,our studies included both children and adolescents (6-20 years old)[20,21,24,25,27],three studies enrolled only adolescents (10-20 years old)[ 23,28,29],two studies recruited both adolescents and young adults (15-39 years old)[ 22,26],the rest one study only included young adults (18-35 years old) [30].Most studies had participants with all types of cancer,except for two studies recruited children with acute lymphoblastic leukemia [21,27].Five studies recruited children undergoing active treatment[23-26,29].The other six studies focused on participants in survivorship[20-22,27,28,30].
3.2.Symptoms used as outcome indicator(s)
Symptom(s) were used as the primary outcome indicator(s) in ten studies,and secondary outcome in one study [21].Among the symptoms,anxiety was the main indicator (n=7),following by depression(n=4),pain(n=3),anger(n=1),fatigue(n=1),fear(n=1),and general symptom distress(n=1).Most studies(n=10)collected participants’ self-reported symptoms with ageappropriate instruments.One study measured different symptom reports by children,parents,and nurses [20].
3.3.Digital health technology-assisted intervention
The digital health technology-assisted interventions mainly incorporated visual reality,website,humanoid robot,app,wearable devices,short messages and videoconference.Specifically,four studies used visual reality as a distraction to reduce the anxiety and pain associated with invasive port device access procedures [20],minimize the anxiety and depressive symptoms during hospitalization [25],alleviate the pain during a lumbar puncture [23],and mitigate chemotherapy-related symptom distress[29].Three studies developed their interventions online,which respectively incorporated a mindful self-compassion videoconference for anxiety and depression alleviation [26],a web-based resource with individually tailored information [22],an internet-based cognitive-behavioral intervention [30].For the rest four studies,one study used a social humanoid robot as a therapy-assistive tool in dealing with pediatric distress [24].Another study developed a Pain Squad+smartphone app to alleviate pain[28].The third study employed a fitness tracker as wearable technology to promote physical activity and diminish fatigue[27].One study combined web,phone,and text messages to deliver a tailored weight management intervention to relieve the negative mood in cancer survivorship[21].
3.4.Effect of interventions on managing symptoms (Table 2)
Seven studies investigated the effect of digital health technology on anxiety.The interventions involved included visual reality[20,25,29],web-based technology [22,26,30],and a humanoid robot [24].Alemi et al.found a significant between-group difference in reductions in anxiety (P < 0.05) for children who received social humanoid robot-assisted therapy[24].However,none of the three studies on visual reality using detected a significant positive effect on reducing anxiety,either by visual reality virtual reality immersive distraction technique [20],or virtual reality computer games [25]or virtual reality scenarios [29].Meanwhile,the three studies involving online interventions released mixed results.Two studies reported a significant reduction in anxiety (Cohen’s d=1.24,P<0.001 and t=3.44,P=0.003,respectively)[26,30].A third study did not find any significant difference (P >0.05) [22].
Four studies reported the effect of the interventions on depression.The involved interventions were a humanoid robot[24],web-based technology [26],visual reality [25],and a combined web,phone,and text messages delivery [21].Their results were consistently positive.In Alemi’s study,children expressed less depression when receiving the social humanoid robot-assisted therapy significantly (M=0.012,F (1,8)=8.66,P < 0.05) [24].Campo’s study suggested a significant decrease in depression level after a mindful self-compassion videoconference intervention(Cohen’s d 0.99,P < 0.001) [26].In the virtual reality computer games led by Li,children in the experimental group reported fewer depressive symptoms compared to those in the control group(P=0.02)[25].Likewise,in Huang’s study,depression was reduced in participants receiving web,phone,and text message delivery(P=0.02) [21].
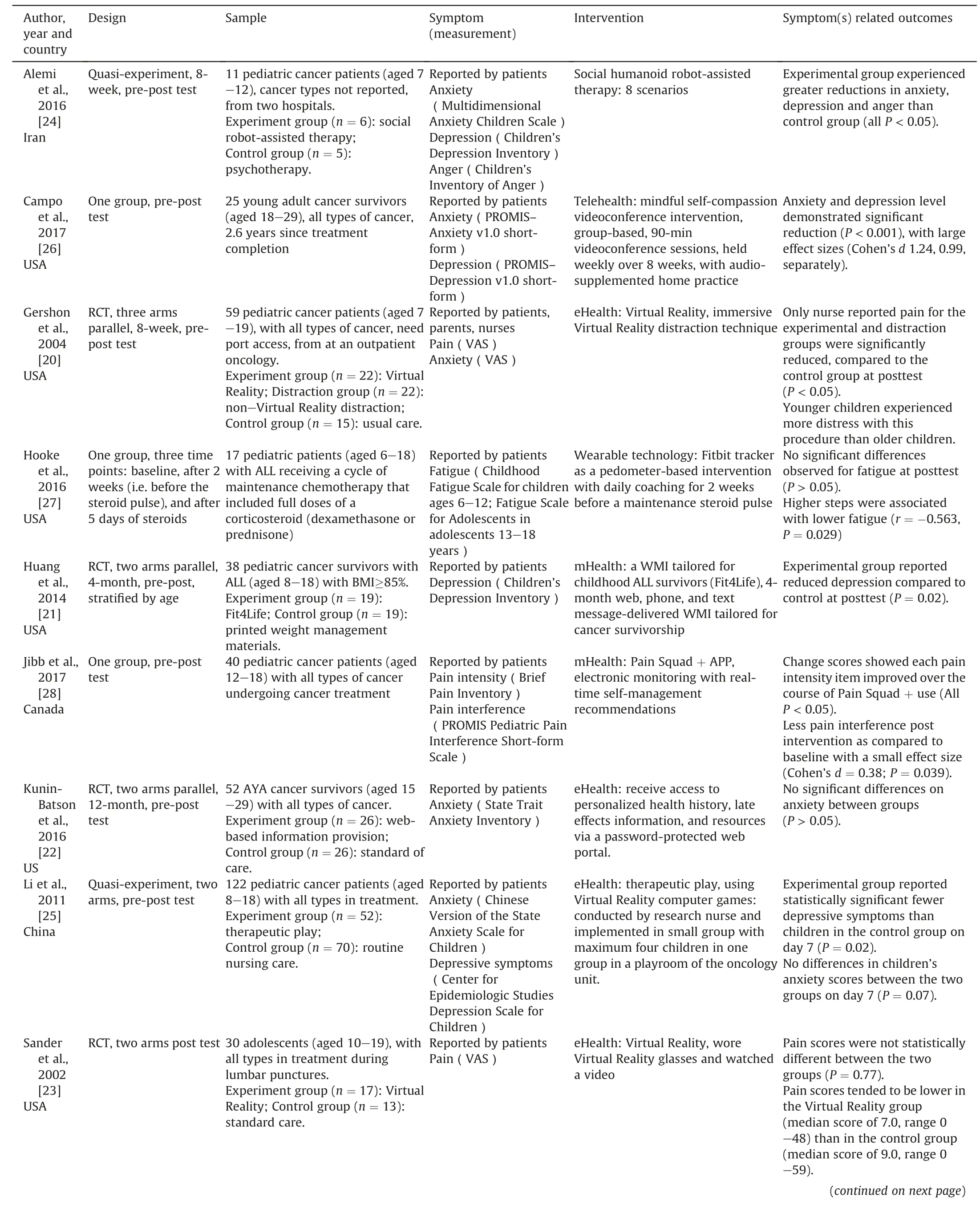
Table 1 A summary of research studies included in the review.

Table 1 (continued)
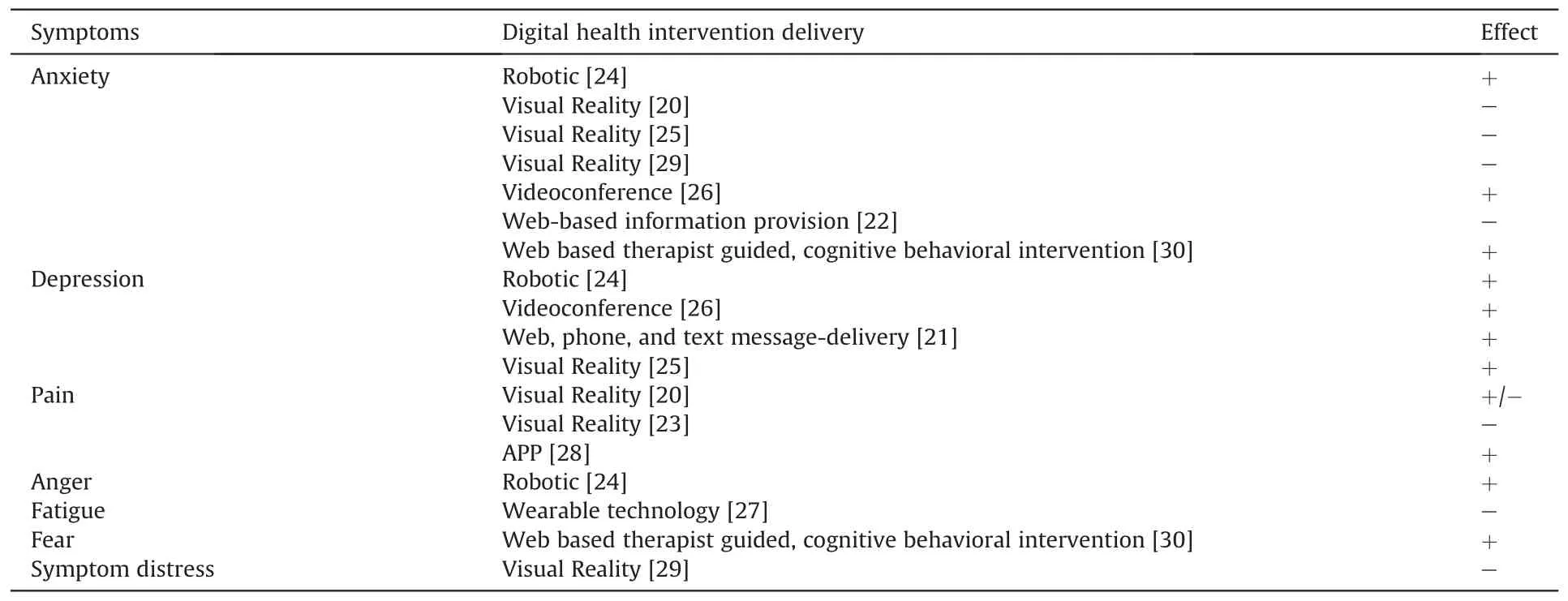
Table 2 Symptoms and effects of digital health technology.
Three studies investigated the effect of digital health technology interventions on pain.The interventions involved included visual reality [20,23]and a smartphone app [28].The results were inconsistent.Neither of the two studies on visual reality interventions detected a statistical difference in patient-reported VAS pain scores between the experiment and control groups.However,a significant posttest decrease in nurse-reported pain scores was noted in one of two studies [20].A Pain Squad+APP was used in Jibb’s study,which revealed a significantly lower pain intensity(P < 0.05) and less pain interference post-intervention (Cohen’s d=0.38,P=0.039) [28].
One study assessed the effect of humanoid robot interventions on anger.In Alemi 2016’s study,social humanoid robot-assisted therapy demonstrated its strength in releasing the participants’anger level(M=0.216,F (1,8)=10.28,P <0.05).
One study reported the effect of wearable technology interventions on fatigue.In the study led by Hooke,Fitbit tracker was used as a pedometer-based intervention with daily coaching for children with acute lymphoblastic leukemia prior to a maintenance steroid pulse.Although higher steps were associated with lower fatigue (r=-0.563,P=0.029),no significant differences were noted in fatigue at a two-week posttest (P=0.42)[27].
One study assessed the effect of web-based therapist guided,cognitive-behavioral intervention on fear.In Seitz’s study,significant decreases in fear of relapse/progression in the 3-month posttest(t=2.14,P=0.046) [30].
One study reported the effect of virtual reality interventions on symptom distress.In Schneider’s study,the participants’symptom distress score decreased during subsequent treatments compared to the initial chemotherapy treatment (P=0.02) [29].
3.5.Level of methodological quality
The studies’quality ranged from moderate to high,with overall scores ranging between 16 and 21 out of 28.All the 11 articles attained a score of 8 or above for the reporting subscale.None of them explicitly described the occurrence of adverse events.The external validity score of the 11 studies was generally fair,from 1 to 3 out of 3.All studies achieved 5 out of 7 for the bias subscale,as blinding was not feasible considering the intervention’s nature.The studies achieved a medium score (2-4 out of 6) on the internal validity subscale,as it was not feasible for assignment concealment.Power analysis was only carried out in 2 studies for sample size estimation (Table 3).
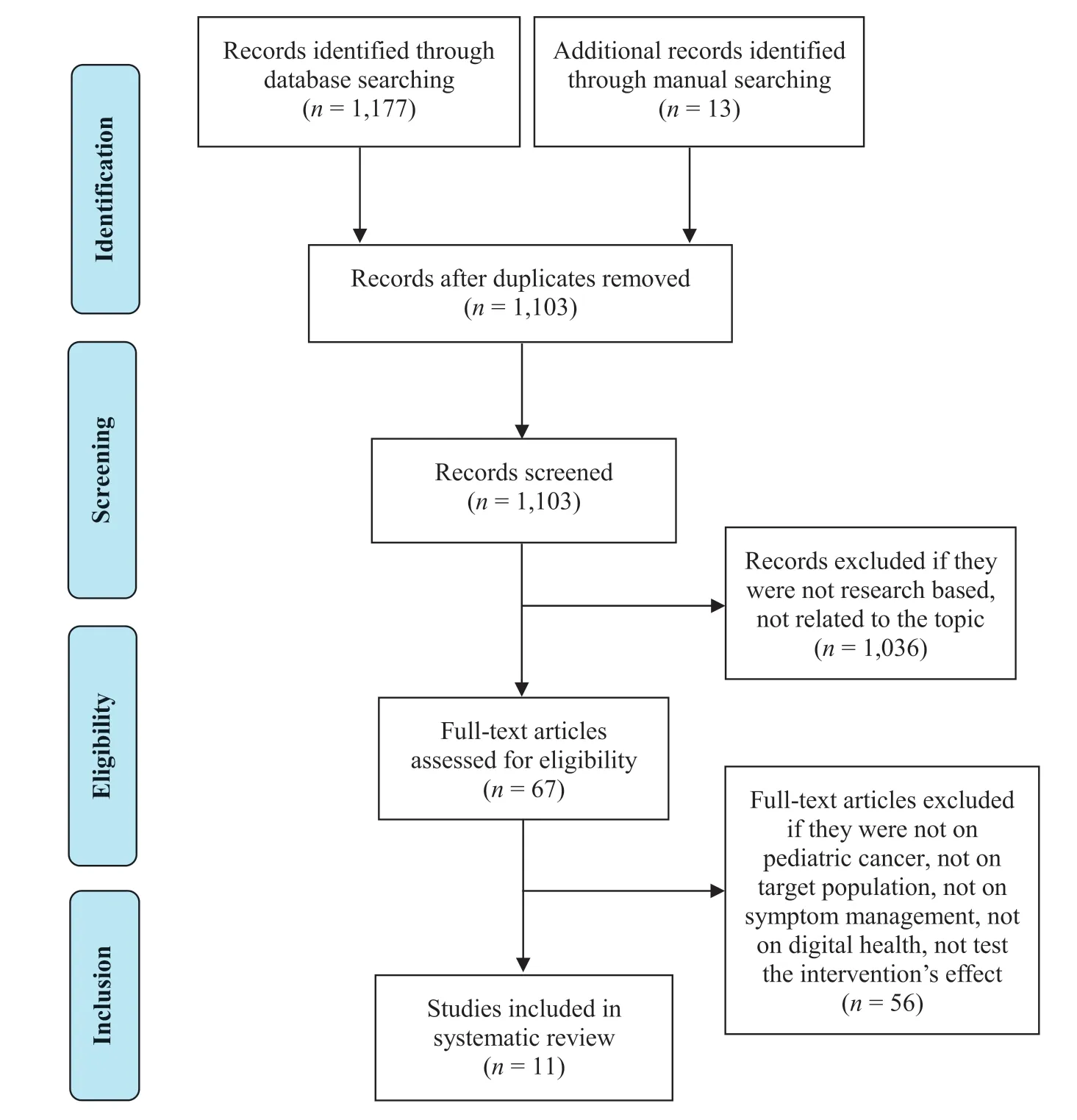
Fig.1.Prisma flow diagram.
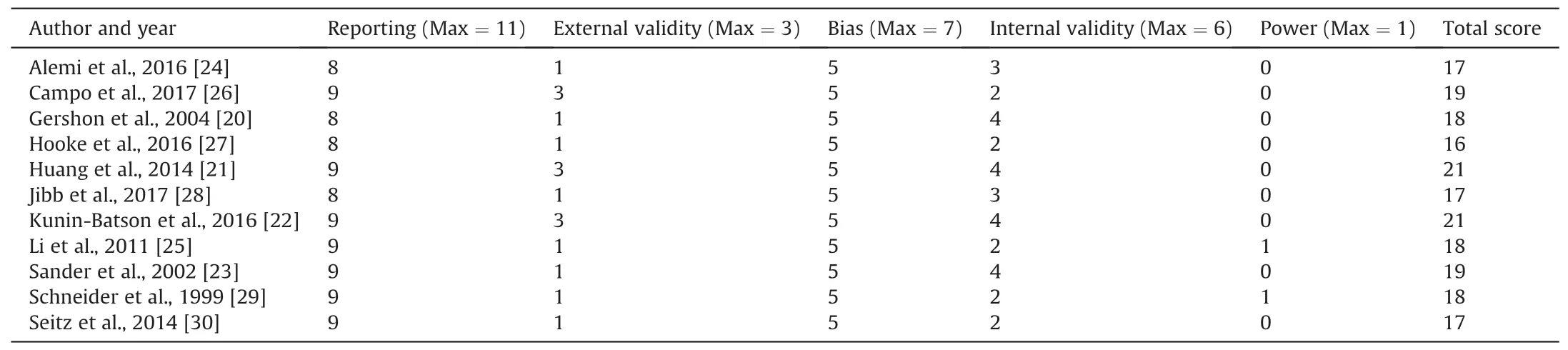
Table 3 Quality of studies.
4.Discussion
In this review,we examined the effect of digital health technologies on managing symptoms across the pediatric cancer continuum.There were seven digital health technologies aimed at addressing seven symptoms in pediatric cancer patients and survivors.Our findings were generally consistent with previous reviews that current evidence supports this intervention is generally mixed and inconclusive [31].Of note,there is a trend that more positive effects were found in the interventions that feature the interactive function of digital health technologies.Meanwhile,influencing factors from the symptoms,participants,and context may influence the intervention’s effects.
In this review,the main categories of digital health technologies included the internet (web-based information provision,webbased therapy),mobile health (app,text messages and wearable devices),telehealth (videoconference),and emerging technologies(visual reality and humanoid robot).The functions of these technologies varied from information deliveries to interactive communications.In general,the technology that involved more interactive features (e.g.,web-based therapy,apps,videoconference,humanoid robot)was likely to generate positive evidence that supports the symptom management across the pediatric cancer continuum.For instance,the internet assists in delivering highquality and tailored symptom management information [32].However,in this review,only when used in conjunction with interactive components (e.g.,web-based therapy,phone,and text message) could the benefit of the internet be evident [21,30].The simple application of online information provision did not lead to positive outcomes [22].Of the three mobile health and one telehealth technologies,their common strengths were consistently shown in symptom management regarding real-time data collection and response,user convenience,patient-clinician connections and interactions.Likewise,in terms of the two emerging digital health technologies,while interactive humanoid robots were proved to be capable to alleviate symptoms,there remained mixed outcomes from the studies on distractions by virtual reality.Obviously,the importance of an interactive feature of digital health technology should not be overlooked in its development and implementation stages.Particularly,for young children with cancer,this feature will catch their attention and get them involved.While for adolescents and young adults with cancer,a digital intervention with an interactive feature will give them a feeling of being recognized and cared for,which is essential for their development of autonomy and self-conscience in symptom management.
When examining the effect of digital health technology,there is a need to take into consideration about the influencing factors from the symptoms,participants,and context levels.First,with respect to symptoms,compared to the various symptoms experienced by children and adolescents with cancer [3],this review only found a limited number of symptoms intervened by digital health technologies.Of note,most of the symptoms were related to psychological health.Although it is widely reported that intersecting and troubling symptoms (e.g.,fatigue,pain and depression) often coexist and are recognized as a part of a symptom cluster [33,34]through a common underlying pathophysiological mechanism,e.g.,systemic inflammation [35].Few studies estimate the synergy effects of symptoms or leverage their digital health interventions according to the targeted symptoms’ relationships.
Second,the characteristics of participants may influence the usability and implementation of digital health technologies.For pediatric cancer patients and survivors,their developmental stages and malignancy treatment are twofold factors that interfere with the intervention.Specifically,the developmental issue needs to be considered when designing the digital health interventions’layout and function,impacting participants’ preference and involvement.As exemplified in this review,only two studies applied technologies targeting a particular age group,i.e.,social humanoid robotassisted therapy for children aged 6-12 years,and web-based therapy for young adults.Meanwhile,the influence of participants’ disease and treatment should not be overlooked,e.g.,neuropsychological complications may prevent a participant from using specific technologies like digital cognitive therapy.Furthermore,it is unlikely to underestimate the impact of other co-existing non-technological symptom interventions,e.g.,the simultaneous usage of EMLA cream for pain alleviation during lumbar puncture[23],other forms of off-line health education (paper format materials,booklets,etc.),and in person symptom management interventions.
Third,the contextual factors that influence digital health technologies’effect may come from users’environment,resources,and culture.It is noted that the majority of the included studies were from developed countries.Participants’financial and technological capabilities may shape their participation willingness.However,there was limited information on how socioeconomic influencers(e.g.,digital resources,sex,family income,or parent education)affects intervention outcomes.Likewise,there is limited information on any direct or indirect costs and health outcomes of different interventions.In light of the variations of health care models and payment methods,it was impossible to perform a cost-effective analysis that examines the interventions’ effect from a health economic lens.Meanwhile,cultural factors were rarely mentioned in the included studies.It would be worthwhile to explore how certain cultural elements (e.g.,the tolerance level of self-exposure during videoconference) impact or moderate the effect of digital health technologies.
This systematic review has limitations.First,the search strategies of this review only involved major databases without grey literature.There is a possibility that some literature may be missed.Second,the studies included in this review were a mixture of randomized controlled trials,pilot studies,or pre-posttests on feasibility and efficacy.The methodological limitations (e.g.,small sample size and lack of control groups)prevented the synthesis and evaluation of the strength of overall evidence.Third,there was considerable heterogeneity in the age group,patients’ developmental level,and sample size of each included study.It was not practical to perform meta-analysis or any sub-analysis but a narrative data synthesis.
Future studies on the effect of digital health technology on symptom management are recommended to address the following areas.First,large scale,robustly designed studies are demanded to test digital health interventions on this particular population.Extended follow-up is especially needed to test the effect alongside the point of diagnosis,during treatment,and in survivorship.Second,there is paucity in current research to explore the relationships between digital health implementation within routine care provision.Particularly,how the enabled distance and real-time symptom management technologies supplement face-to-face delivery of care for those who are restrained from trained providers due to distance,mobility difficulties,and cancer stigma.Third,it is necessary to fully interpret the effect of digital health technology on symptom management across the cancer continuum with consideration of the multiple influencing factors from symptoms,participants,and context levels.
5.Conclusion
At present,digital health technology serves an increasingly important role in managing symptoms across pediatric cancer continuing.However,this review suggested that current evidence supports the effect of this intervention is generally mixed and inconclusive.Of note,there is a trend of positive effects found in the interventions that feature interactive function.This review highlights the need for further investigation with rigorous research designs and increased sample sizes to further examine the effect alongside the pediatric cancer continuum.Meanwhile,influencing factors from the symptoms,participants,and context need to be considered to inform a better digital health implementation.
CRediT authorship contribution statement
Lei Cheng:Conceptualization,Methodology,Validation,Writing-original draft,Writing -review & editing.Mingxia Duan:Investigation,Data curation,Writing-review&editing.Xiaorong Mao:Investigation,Data curation,Writing -review & editing.Youhong Ge:Investigation,Data curation,Writing -review & editing.Yanqing Wang:Investigation,Data curation,Writing -review &editing.Haiying Huang:Data curation,Writing-review&editing.
Statement of ethics approval
This study does not need ethical approval as it is a systematic review of literature.
Funding
This study was supported by the China National Natural Science Foundation of China Youth Science Foundation (71904030),and Shanghai Pujiang Talent Program(2019PJC006).
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Appendices Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.10.002.
 International Journal of Nursing Sciences2021年1期
International Journal of Nursing Sciences2021年1期
- International Journal of Nursing Sciences的其它文章
- Focuses and trends of the studies on pediatric palliative care:A bibliometric analysis from 2004 to 2018
- Relationship between negative emotions and perceived support among parents of hospitalized,critically ill children
- Effectiveness of animal-assisted therapy on pain in children:A systematic review and meta-analysis
- Effects of creative expression program on the event-related potential and task reaction time of elderly with mild cognitive impairment
- Struggling to live a new normal life among Chinese women after losing an only child:A qualitative study
- Implementation and evaluation of a pain management core competency education program for surgical nurses
