Pheochromocytoma as a cause of repeated acute myocardial infarctions,heart failure,and transient erythrocytosis:A case report and review of the literature
Fei Shi,Li-Xian Sun,Ying Zhang,Department of Cardiology,Affiliated Hospital of Chengde Medical University,Chengde 067000,Hebei Province,China
Sen Long,Department of Traditional Chinese Medicine,Affiliated Hospital of Chengde Medical University,Chengde 067000,Hebei Province,China
Abstract BACKGROUND Pheochromocytoma is a rare catecholamines-secreting tumor arising from chromaffin cells in the adrenal medulla.It classically presents with paroxysmal hypertension,headaches,palpitations,sweating,and metabolic disorders.Atypical presentations such as acute myocardial infarction,heart failure,cardiomyopathy,stroke,and transient erythrocytosis have been infrequently documented.CASE SUMMARY We describe the case of a 72-year-old man diagnosed with pheochromocytoma presenting with non-ST segment elevation myocardial infarction,heart failure,and transient erythrocytosis with nonobstructed coronary arteries.This was his second heart attack.The patient was previously diagnosed with myocardial infarction,and an immense mass was found on the left adrenal gland 3 years prior.Based on clinical and laboratory findings,a diagnosis of pheochromocytoma was confirmed.His coronary angiogram showed nonobstructed coronary arteries except for a myocardial bridge in the left anterior descending branch.This was a form of type-2 myocardial infarction.The myocardial cell lesions were caused by sudden secretion of catecholamines by the pheochromocytoma.Even more atypically,his hemoglobin level was obviously elevated at admission,but after a few days of treatment with an alpha-adrenergic receptor blocker,it dropped to normal levels without additional treatment.CONCLUSION Pheochromocytoma may be a cause of acute myocardial infarction,heart failure,and transient erythrocytosis.
Key Words:Pheochromocytoma;Myocardial infarction;Heart failure;Cardiomyopathy;Erythrocytosis;Case report
INTRODUCTION
Pheochromocytoma is a neuroendocrine tumor of the adrenal medulla.The prevalence of pheochromocytoma is estimated at between 1:4500 and 1:1700 in the general population[1].Severe cardiovascular complications including ventricular tachycardia,ST and non-ST segment elevation myocardial infarction (NSTEMI),heart failure,stress cardiomyopathy,and hypertensive urgency can occur in 19.3% of pheochromocytoma patients[2,3].It classically presents with paroxysmal hypertension,headaches,palpitations,sweating,and metabolic disorders[4-7].Plasma and urinary catecholamine and 24-hurine vanillylmandelic acid measurements can be helpful to aid its diagnosis in addition to computed tomography scans or other imaging examinations.In this study,we present a case with acute myocardial infarction,heart failure,and transient erythrocytosis secondary to pheochromocytoma.
CASE PRESENTATION
Chief complaints
A 72-year-old Chinese man presented to the Emergency Department of our hospital with retrosternal chest pain.The pain lasted approximately half an hour and was associated with palpitations,sweating,dizziness,nausea,and difficulty breathing.
History of present illness
In the prior 3 years,the patient experienced intermittent retrosternal pain with palpitations,sweating,fatigue,and dizziness lasting from a few minutes to an hour.The patient’s symptoms relapsed 3 d before admission in a resting state.He was previously diagnosed with NSTEMI,and an immense mass was found on his left adrenal gland 3 years prior.Since then,he was treated with aspirin,statin,and nitrate for an extended time,but there was no obvious effect.At the same time,progressive weight loss was observed (approximately 5 kg within the prior 6 mo,16 kg in total since NSTEMI diagnosis).
History of past illness
The patient had a history of paroxysmal hypertension for 3 years.Because of the large fluctuation of blood pressure (from 11.9/7.3 kPa to 30.6/18.6 kPa),taking medicine was burdensome to him.He was treated with oral nifedipine intermittently (nifedipine was taken when blood pressure higher than 18.6/13.3 kPa).
Personal and family history
He had been smoking approximately 10 cigarettes a day for 30 years.There was no significant family history to note.
Physical examination
During the patient’s hospital stay,his blood pressure showed erratic fluctuations from 27.1/17.0 kPa to 11.8/7.4 kPa and heart rates from 79 to 138 beats per minute associated with the symptoms described previously.His body weight was 54 kg and height was 170 cm (BMI 18.7 kg/m2).The physical examination revealed mild bilateral basilar crackles,with no jugular venous distention and normal heart sounds.He had tenderness beneath the xiphoid process,and there was no peripheral pedal edema.
Laboratory examinations
The patient was diagnosed with NSTEMI because troponin I was abnormal (0.75 ng/mL and 0.89 ng/mL,normal reference <0.4 ng/mL).Electrocardiogram showed sinus tachycardia,incomplete right bundle branch block,and no significant change in ST segment or T wave (Figure 1).Brain natriuretic peptide (BNP),a biomarker of heart failure,was significantly increased (2980 pg/mL,normal reference <100 pg/mL).An unusual blood test was also found.The levels of the patient’s hemoglobin increased remarkably (203 g/L and 194 g/L,normal reference 130-175 g/L).These episodic symptoms,the erratic blood pressure pattern,and the volume of the mass on adrenal gland raised the suspicion of pheochromocytoma.Plasma and urinary catecholamines were elevated more than 10-fold compared to the reference range (Table 1).The value of 24-h urine vanillylmandelic acid was also extremely high (86.2 mg/24 h and 69.5 mg/24 h,normal reference 0-12 mg/24 h).
Imaging examinations
Computed tomography and Doppler ultrasound showed a well-defined,rounded mass in the left adrenal gland,measuring 46.4 mm × 53.5 mm × 56.0 mm (Figure 2),which was consistent with the diagnosis of pheochromocytoma.The left ventricular ejection fraction (LVEF) was measured by cardiac Doppler ultrasound and was only 41%.Additionally,a regional wall motion defect was observed.The patient’s biomarker of acute myocardial infarction was mildly elevated,and there were no new Q waves or changes in ST segment.We suspected that there was no obstruction in his coronary arteries.After a loading dose of aspirin and clopidogrel,coronary angiography was performed and revealed no occlusion in coronary arteries except a myocardial bridge in the left anterior descending branch (Figure 3).
FINAL DIAGNOSIS
The final diagnosis was pheochromocytoma with secondary acute myocardial infarction and heart failure.
TREATMENT
The patient was medically stabilized with an alpha-adrenergic receptor blocker(terazosin,4 mg per day).Dyspnea was relieved by diuretics (furosemide,20 mg per day and spironolactone,20 mg per day).He refused to have a left adrenalectomy.
OUTCOME AND FOLLOW-UP
After 10 d of medication,the patient’s symptoms improved.The biomarkers of myocardial injury returned to normal,and BNP decreased to 1070 pg/mL.Interestingly,his hemoglobin level also dropped to normal (137 g/L) without additional treatment.At the 1-mo follow-up,he had no complaints and his BNP decreased to 385 pg/mL and LVEF returned to normal (52%).
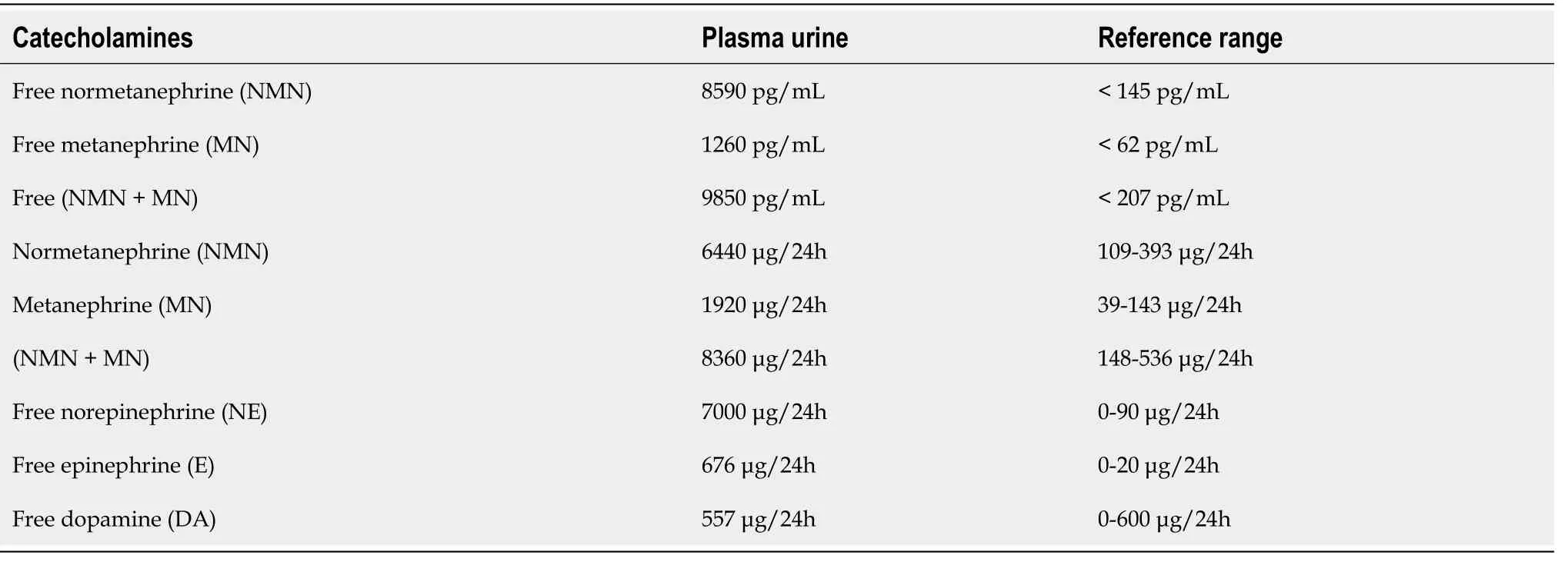
Table 1 Laboratory test results of plasma and urinary catecholamines
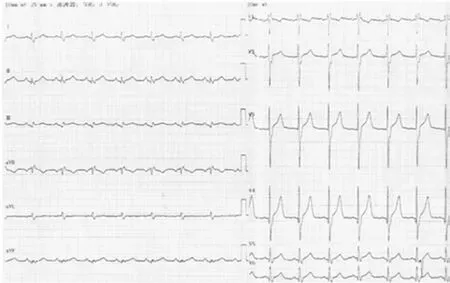
Figure 1 Electrocardiogram at hospital admission.
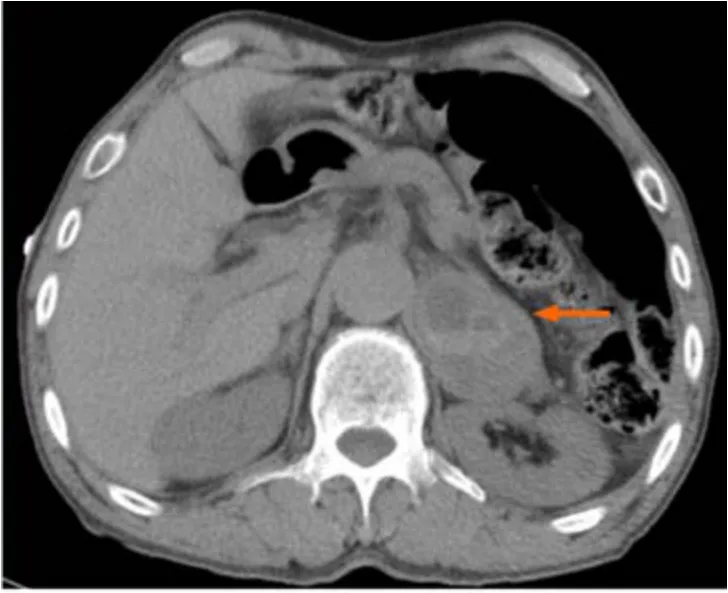
Figure 2 Computed tomography scan revealing an immense mass (marked by arrow) in the left adrenal gland (46.4 mm × 53.5 mm × 56.0 mm).
DISCUSSION
Pheochromocytoma with life-threatening cardiovascular complications is rare and atypical.In our case,the patient was diagnosed with pheochromocytoma presenting with repeated acute myocardial infarctions and heart failure.The coronary angiogram showed nonobstructed coronary arteries.We noted that most of such patients had few significant coronary atherosclerosis in past reports[8-10].Most reports suggested that cardiomyopathy,severe coronary vasospasm,myocarditis,and tachycardia caused by excessive release of catecholamines result in elevated cardiac troponin and reduced left ventricular systolic function[11,12].This case illustrates pheochromocytoma as one of the differential diagnoses for myocardial infarction with nonobstructed coronary arteries,especially in patients with unexplained erratic blood pressure and symptoms suggestive of pheochromocytoma.

Figure 3 Coronary angiogram showing nonobstructed coronaries.
In this case,the patient’s biomarker of acute myocardial infarction was mildly elevated,which was not consistent with the severity of heart failure.Pheochromocytoma can lead to different cardiomyopathies,including Takotsubo cardiomyopathies and catecholamine cardiomyopathies[13,14].
Takotsubo cardiomyopathy,also called stress cardiomyopathy or apical ballooning syndrome,may lead to transient left ventricular systolic dysfunction and mimic ST segment elevation myocardial infarction[15-17].The left ventriculography and echocardiography can show a ballooning pattern that is most apparent in the anterior wall and apical septum rather than the basal part of the left ventricle[18].The abnormal motion of the myocardium would normalizes within a few days to several weeks[19-21].In this case,the patient was diagnosed with NSTEMI with nonobstructed coronary arteries and segmental left ventricular wall motion abnormalities (no ballooning pattern,and LVEF was only 41%).This is a form of catecholamine cardiomyopathy.The two types of cardiomyopathies may be explained by the same pathophysiological mechanism of catecholamine oversecretion which induces microvascular dysfunction,epicardial spasm,and direct effects on cardiac myocytes[22].Acute pulmonary edema is more frequent in catecholamine cardiomyopathy.Left ventricular mass index,relative wall thickness,and elevated blood pressure are more prominent in catecholamine cardiomyopathy compared to Takotsubo cardiomyopathy[23].Patients with Takotsubo cardiomyopathy exhibit better recovery of left ventricular ejection fraction.The reported in-hospital mortality rate of pheochromocytoma-induced cardiomyopathy is relatively low (2.5%)[24].Early diagnosis of both conditions is crucial for improving prognosis[25].
Pheochromocytoma with erythrocytosis is rarely reported.This atypical syndrome may result from somatic mutations in hypoxia-inducible factor 2A (HIF-2A) and germline mutations in prolyl hydroxylases 1 and 2 (PHD1andPHD2),which have been identified to function as regulators of erythropoietin and its receptor[26-29].A new report provides evidence of an association between a somatic iron regulatory protein (IRP1) mutation and pheochromocytoma with secondary erythrocytosis[30].IRP1 is a principal regulator of translational derepression ofHIF-2AmRNA in iron-deficient cells,which facilitatesHIF-2AmRNA accumulation and increased stimulation of erythropoietin expression[31,32].These findings explain the transient exacerbation of secondary polycythemia in patients with erythropoietin-secreting pheochromocytoma[33].Elevated hematocrit contributes to increased blood viscosity and platelet adhesion[34,35].Increased blood viscosity promotes blood clot formation and increased platelet activation at the vessel wall and thus,presents a higher risk of coronary heart disease[36].
Many different treatment options are used to control the effects of catecholamine hypersecretion including blockades (such as alpha blockers,calcium channel blockers,beta blockers,and tyrosine hydroxylase inhibitors),surgical resection,radiofrequency ablation,and radiotherapy[37].Alpha blockers and surgical resection are the primary approach for managing patients with pheochromocytoma.Phenoxybenzamine is a long-lasting and noncompetitive inhibitor that is commonly used in perioperative management.Other alpha blockers such as doxazosin,terazosin,and prazosin can be used when phenoxybenzamine is not available or when a patient's hypertension is not severe enough to warrant the use of a long-acting alpha blocker.Calcium channel blockers can also be used for additional blood pressure control.These include nifedipine,amlodipine,and verapamil.In patients with tachycardia,arrhythmias,or angina,beta blockers such as propranolol,atenolol,or metoprolol are indicated.Beta blockers should never be used in the absence of an efficient α-blockade because loss of β-adrenoceptor-mediated vasodilatation can lead to hypertensive crises and even cardiac arrest[38,39].Surgical resection,especially laparoscopic surgery,has been successfully performed in patients with pheochromocytoma with outcomes similar to open surgery[40,41](Table 2).
CONCLUSION
Excessive release of catecholamines in pheochromocytoma results in elevated cardiac troponin,reduced left ventricular systolic function,and transient erythrocytosis with most lesions returning to normal within days to weeks.In patients with unexplained erratic blood pressure control and myocardial infarction with normal coronary arteries,pheochromocytoma should be considered a differential diagnosis.

Table 2 Timeline
ACKNOWLEDGEMENTS
The authors thank the patient and his family for their participation.
 World Journal of Clinical Cases2021年4期
World Journal of Clinical Cases2021年4期
- World Journal of Clinical Cases的其它文章
- Isolated interrupted aortic arch in an adult:A case report
- Fertility-sparing surgeries without adjuvant therapy through term pregnancies in a patient with low-grade endometrial stromal sarcoma:A case report
- Primary nonkeratinizing squamous cell carcinoma of the scapular bone:A case report
- Acute inferior wall myocardial infarction induced by aortic dissection in a young adult with Marfan syndrome:A case report
- Immediate implant placement in combination with platelet rich-fibrin into extraction sites with periapical infection in the esthetic zone:A case report and review of literature
- Renal failure and hepatitis following ingestion of raw grass carp gallbladder:A case report
