COVlD-19 outbreak and endoscopy:Considerations in patients encountered in a foregut surgery practice
Tanya Olszewski,Andrew D Grubic,Shahin Ayazi,Blair A Jobe,Esophageal and Lung Institute,Department of Surgery,Allegheny Health Network,Pittsburgh,PA 15224,United States
Abstract Severe acute respiratory syndrome coronavirus has become a critical challenge to global health.Since the arrival of coronavirus disease 2019 in the United States,several government agencies and professional societies have issued guidelines to healthcare systems and medical providers.Endoscopy is a substantial portion of the practice of many general surgeons in the United States.With upper endoscopy,manipulation of the upper aerodigestive tract can turn the droplets to an aerosolized form and increase the likelihood of transmission and therefore is considered a high-risk procedure.In this article we review some aspects of the coronavirus disease 2019 outbreak that are relevant to practice of surgical endoscopy.The emphasis of this communication is on the mode of transmission,previous experiences during other coronavirus outbreaks and society guidelines.We then highlight the changes that we have made to our practice to incorporate these factors to improve the safety of patients,health care providers,and community as a whole.
Key words:SARS-CoV-2;COVID-19;Endoscopy;Pandemic;Best practice;Personal protection equipment
INTRODUCTION
Since identification of novel severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) as the causative agent from a cluster of pneumonias in the Hubei providence of China in December 2019,coronavirus disease 2019 (COVID-19) has rapidly evolved into a global pandemic.The United States with more than 175000 confirmed cases is now the global epicenter of this pandemic.
With the arrival of COVID-19 in the United States,several government agencies and professional societies have issued guidelines to healthcare systems and medical providers.Surgical providers have been forced to reconsider many aspects of their routine clinical practice.Elective surgeries are cancelled,and all non-urgent heath care is postponed.The Centers for Medicare and Medicaid Services also created a framework of tiers to help surgeons identify whether to forego surgical or endoscopic procedures for given clinical presentations[1].The framework includes 3 tiers and recommends intervention in high acuity procedures in healthy and unhealthy patients or patients who have intermediate acuity and potential future morbidity and mortality by delaying care for their disease.
As surgeons we aim to practice within best practice models using sound evidence to protect our patients,staff,ourselves and subsequently future patients,families and the community from infection.Endoscopy is a substantial portion of the practice of many general surgeons in the United States.With upper endoscopy,manipulation of the upper aerodigestive tract can turn the droplets to an aerosolized form and increase the likelihood of transmission and therefore is considered a high-risk procedure.
In this article we review some aspects of the COVID-19 outbreak that are relevant to practice of surgical endoscopy.The emphasis of this communication is on the mode of transmission,previous experiences during other coronavirus outbreaks and society guidelines.We then highlight the changes that we have made to our practice to incorporate these factors to improve the safety of patients,health care providers,and community as a whole.
CLINICAL PRESENTATION AND DIAGNOSIS OF COVID-19
Patients infected with SARS-CoV-2 who develop COVID-19 primarily present with fever (91%) and dry cough (67%) but have also been shown to have dyspnea,weakness,fatigue,diarrhea,abdominal discomfort and/or poor appetite[2-4].Patients with dyspnea can possibly progress to acute respiratory distress syndrome as well as coagulation dysfunction,either of which can lead to death[3].Pan and colleague reviewed 204 confirmed COVID-19 patients and found that 18% of them initially presented with gastrointestinal symptoms including diarrhea,vomiting and abdominal pain.Some patients primarily had these symptoms without coinciding respiratory symptoms and therefore led to delay in diagnosis and admission[5].
One of the challenges of health care providers during this outbreak is the nonspecific presentation of the disease and limitations of current diagnostic tests.The primary method of diagnosis is by real time reverse transcription-polymerase chain reaction analysis of nasopharyngeal swab specimens.This technique is highly specific but lacks sensitivity.False negative values of this test are reported to be 30%-40%;therefore,reliable exclusion of COVID-19 infection requires multiple negative tests[6].
One other major concern is transmission during the asymptomatic incubation period.Data obtained from the Diamond Princess cruise ship in which all quarantined passengers were screened,showed that 619 (17%) of passengers tested positive,and over half of cases were asymptomatic at the time of diagnosis[7].If asymptomatic patients undergo endoscopy during their incubation period they can infect the health care staff and contaminate the physical space of the gastrointestinal suite or operating room.Since,conventional personal protection equipment (PPE) does not provide adequate protection against COVID-19,the endoscopy team is also at risk.
IMPACT OF DIFFERENT MODES OF TRANSMISSION
Large respiratory droplets are considered to be the primary transmission vector of the SARS-CoV-2 virus.Guidelines for proper PPE have been largely aimed at airway procedures such as intubations.However the data on aerosolization during esophagogastroduodenoscopy is limited as well as possible fecal-oral route of transmission during colonoscopy.Given that colonoscopy is one of the most common procedures performed by general surgeons in the United States,we must consider the implications of disease spread for both upper endoscopy and colonoscopy.In order for surgeons to manage emergent and urgent situations endoscopically,the need to standardize endoscopic treatment is necessary for the safety of everyone.
In the late 1800's Joseph Lister described a phenomenon of “minute particles suspended in (the air)” which could infect wounds in patients with open fractures.Since this time our knowledge of airborne transmission of infection has rapidly evolved,including the risk posed to patients,healthcare workers,and support staff by aerosol generating procedures (AGPs).Prior studies have shown that AGPs including endoscopic procedures generate a variety of airborne particles,classically characterized as droplets and aerosols.Droplets are collections of hydrostatically bound liquid which frequently contain cellular debris including pathogens.Aerosols are similar,but finer particles which linger in the air and travel greater distances,thus increasing infectious potential.Biological aerosols may vary in size from 0.5-5 µm while droplets are considerably larger ranging 5-200 µm.Part of the reason for this delineation is that particles of < 5 µm may travel to the lower respiratory tract,while more substantial particles tend to be filtered and deposited in the nasopharynx and oropharynx.There is debate regarding the infection potential related to the various size classifications.A prior influenza study showed that viral copies were 8.8 times more numerous in smaller (≤ 5 µm) than in larger (> 5 µm) airborne particles[8,9].
RECOMMENDATIONS OF PROFESSIONAL SOCIETIES
Recommendations from American Gastroenterological Association,American Association of the Study of Liver Disease,American College of Gastroenterology and American Society for Gastrointestinal Surgery have been combined into a joint communication for their memberships.They recommend that during any endoscopic procedure,all members of the team wear gloves,mask,eye shield or goggles,face shields and gowns,which is in adherence to Centers for Disease Control and Prevention guidelines for droplet precautions[10].Zhanget al[2]created a workflow for endoscopy being performed in China after the COVID-19 outbreak and recommends protection at biosafety level 3 for all kinds of endoscopic procedures in COVID-19 infected or suspected patients,which is equivalent to airborne precautions.
N-95 masks can filter > 95% particles that are 0.3 microns or greater.If well fitted,they can provide excellent protection from aerosolized particles.A powered airpurifying respirator has been proposed to provide improved protection compared to N-95,due to health care worker transmission during similar viral outbreaks,but this observation may be confounded by improper fitting of N-95 masks.Prior work with influenza has shown that a full face shield may decrease inspired particles and contamination of the underlying mask,particularly at close proximity to the patient.Negative pressure rooms should be considered for AGPs if available and safely feasible.
The increasing prevalence of COVID-19 coupled with the suspected asymptomatic and presymptomatic transmission of the virus,generates a question for need for“universal precautions”.This concept has been widely adopted for blood borne pathogens,and treats all individuals as potential infectious carriers.While we are currently experiencing limited global supply of N-95 masks,there should be strong consideration of “universal precautions” for all personnel during all AGPs.Ultimately implemented policies will need to reflect current N-95 supply and regional COVID-19 prevalence[11].
Coronavirus has historically been identified in stool samples during the SARS-CoV epidemic as well.Interestingly,in a study done by Leunget al[12]in 2003,patients who had diarrhea during their disease course of SARS-CoV had a significantly higher need for intensive care unit care (P≤ 0.001) and also ventilator support (P= 0.004).Postmortem evaluations on four deceased patients and in one patient who underwent colonoscopy with biopsies showed viral particles consistent with coronavirus present in the small intestine.The particles were found both intracellularly in the endoplasmic reticulum and also on the surface microvilli.They reported viral RNA detection in stool samples up to 73 d after symptom onset although no viable virus was able to be recovered from stool samples,therefore it was unclear whether the virus was infectious from the fecal-oral route[12,13].
SARS-CoV-2 has also been shown to be present in feces.Xiaoet al[13]studied a total of 73 patients and found that 53% had SARS-CoV-2 RNA in their stool.In addition to their study,other case reports have identified patients who present with negative pharyngeal and sputum viral tests however they test positive for the virus in their fecal specimens[13,14].Additionally,Xiaoet al[13]'s research included upper endoscopy and colonoscopy on COVID-19 positive patients and identified numerous infiltrating plasma cells,lymphocytes and viral nucleocapsid proteins in the stomach,duodenum and rectum although no obvious damage to these cells was identified.These viral particles were present in stool up to 12 d later.The Food and Drug Administration recently released information that SARS-CoV-2 may be transmitted by fecal microbiota for transplantation,the act of recolonizing a patient's gastrointestinal tract after an infection such as recurrent Clostridium difficile,and therefore instituted new guidelines for use of transplants obtained after December 2019[15].These are all strong indicators of a possible fecal-oral route of transmission of the virus[13].
Another area to consider when discussing transmission to staff or uninfected patients is the endoscope itself.There are several resources describing the cleaning process.As a practice,we follow that as described by Ryuet al[16].Their study concluded that a majority of exogenous infection outbreaks were caused by the reprocessing procedures of contaminated endoscopes.They recommend a seven step process of pre-cleaning,cleaning,rinse,high-level disinfection,rinse,drying(air/alcohol) and storage[16].
One study tracking the disease propagation of Middle East respiratory syndrome -CoV identified that patients with falsely negative tests but with symptoms are at high risk for spread of the disease.The transmissions appreciated in the study showed four generations of disease all within health care workers,identifying the need to enact detailed surveillance and screening of health care workers despite presence of symptoms[17].
OUR BEST PRACTICE OUTLINE FOR ENDOSCOPY
Given all the information we have available regarding SARS-CoV-2 from disease process to routes of transmission;our surgical team has decided to create our own best practice guidelines to follow during this COVID-19 pandemic:(1) Follow the ACS guidelines and to reschedule all elective surgical cases and endoscopies.We follow the tiered approach to classify patients into elective,urgent and emergent categories and offer both surgical and endoscopic approaches to these patients as necessary(Table1);(2) Screen all patients by telephone with a questionnaire the day before in addition to checking temperature before admission to endoscopy suite.To consider changing to rapid COVID-19 test if it becomes available;(3) Consider all patients as possible asymptomatic carriers who can transmit virus to staff;(4) Consider SARSCoV-2 as transmissible by surface contact,droplet,airborne and fecal-oral;(5) Limit number of staff necessary during procedure.All staff present should wear a fit-tested NIOSH-approved N-95 mask,gloves,eye shield or goggles,face shields and gowns.All patients should be considered infectious,regardless of symptoms or testing status.Universal,full PPE including N-95 mask should be used,but due to global shortage,this practice may be limited by government and institutional policy;(6) Staff handling endoscopic biopsies after endoscopy will wear gloves,mask,eye shield or goggles,face shields and gowns;and (7) After the patient and endoscope has been removed from the room,all hard surfaces should be cleaned and sanitized per Centers for Disease Control and Prevention guidelines.If a non-negative pressure room is used,aerosolized particles may linger in the air and may settle.Ideally surface cleaning should occur after 30 min to minimize re-contamination of cleaned surfaces.
With these changes to our present practice,we aim to limit the spread from both symptomatic and asymptomatic patients to our staff in order to also protect our future patients.We recognize the need to limit the number of procedures we perform as well in order to limit exposure as well as limit the overall use of PPE.
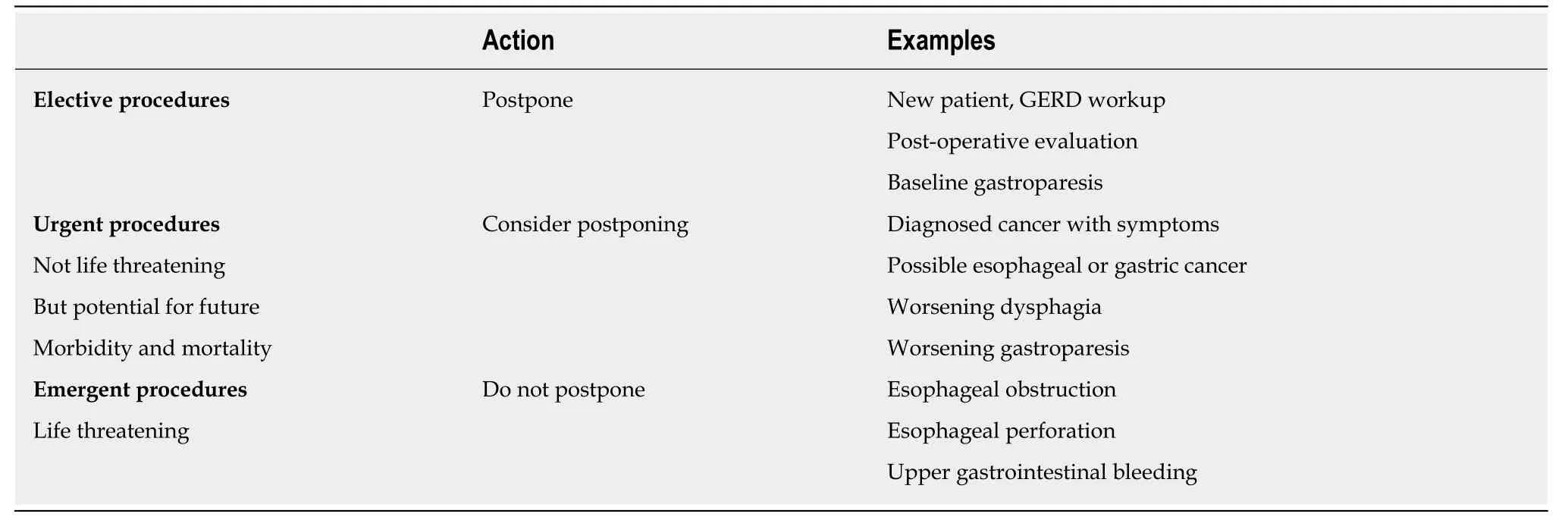
Table1 Foregut surgeon endoscopic procedures
 World Journal of Gastrointestinal Surgery2020年5期
World Journal of Gastrointestinal Surgery2020年5期
- World Journal of Gastrointestinal Surgery的其它文章
- When the bowel meets the bladder:Optimal management of colorectal pathology with urological involvement
- Effect of cholesterol on in vitro cultured interstitial Cajal-like cells isolated from guinea pig gallbladders
- Software improvement for evaluation of laryngopharyngeal pH testing (Restech) - a comparison between DataView 3 and 4
- Management of synchronous lateral pelvic nodal metastasis in rectal cancer in the era of neoadjuvant chemoradiation:A systemic review
- lntroduction of new techniques and technologies in surgery:Where is transanal total mesorectal excision today?
