Effectiveness and safety of antithrombotic strategies in elderly patients with acute myocardial infarction
Elisa Rondano,Marzia Bertolazzi,Alessandro Galluzzo,Ludovica Maltese,Paolo Caccianotti,Sergio Macciò,Stefano Mazza,Maria Virginia Di Ruocco,Serena Favretto,Eraldo Occhetta,Francesco Rametta
Abstract
Key Words:Antiplatelet therapy;Anticoagulant therapy;Elderly patients;Safety;Acute myocardial infarction
INTRODUCTION
Elderly patients,with an increased average lifespan,represent a rapidly growing part of the population who are more susceptible both to acute coronary syndromes (ACS)and to their complications as well as complications related to antithrombotic treatment[1,2].These patients are poorly represented in clinical studies and are more likely to have multiple comorbidities[3,4].
There is no universally accepted definition of an “elderly” patient.The most commonly used cut-off in the literature is 75 years as a significant worsening of outcome after an acute coronary event has been shown by this age[5],but a cut-off of 80 years might be more significant and correspond to clinical practice[1].As these patients more frequently present with atypical symptoms,the diagnosis of myocardial infarction (MI) may be delayed or missed.Irrespective of age,an early invasive strategy should be considered in ACS,although increasing age is known to be an important predictor of worse outcomes[6-8].Furthermore,the need to start antiplatelet therapy and eventually anticoagulant therapy,if atrial fibrillation (AF) is associated,increases the risk of morbidity and mortality in this frail population.For all these reasons and due to the paucity of specific evidence,the management of these patients still represents a challenge[9].
In the present real-world study on a population of “elderly” patients hospitalized due to an acute myocardial infarction,we aimed to investigate our practice during inhospital time and outcomes during the first year of follow-up,including the safety of antithrombotic therapy[10].
MATERIALS AND METHODS
All consecutive patients older than 80 years admitted to the Division of Cardiology of St.Andrea Hospital of Vercelli from January 2018 to December 2018 for ST-elevation myocardial infarction (STEMI) or non-ST elevation myocardial infarction (NSTEMI)were retrospectively evaluated.The diagnosis was based on the European Society of Cardiology guidelines for the management of acute myocardial infarction in patients presenting with and without ST-segment elevation[3,4].
For each patient,we evaluated cardiovascular risk factors (hypertension,hyperlipidemia,diabetes,overweight defined as body mass index >25,smoking,family history of coronary artery disease),creatinine and hemoglobin levels at admission and discharge.An evaluation of the global hemorrhagic risk for each patient was performed a posteriori by calculating the PRECISE-DAPT score[11].We also reported the prevalence of previous paroxysmal,persistent/permanent AF or its inhospital de-novo incidence.
In-hospital management,consisting of coronary angiography and percutaneous coronary angioplasty or conservative strategy is described,as well as the following medical therapy for each patient,in particular treatment with single or dual antiplatelet therapy (DAPT) started during hospitalization and,when necessary,anticoagulant therapy [vitamin K inhibitors (VKAs) or direct oral anticoagulants(DOACs)].
The 1-year follow-up data were collected through ambulatory visits or telephone interviews and were focused on the efficacy endpoint consisting of major adverse cardiovascular events (MACEs,including CV death,stroke and myocardial infarction)and the safety endpoint including minor and major bleeding,classified according to the modified thrombolysis in myocardial infarction trial definitions[12]:A bleeding event was defined as major if it was intracranial or if red blood cell transfusion was clinically indicated in association with a significant drop in hemoglobin level.Oneyear global death is also reported.
A comparison between STEMI and NSTEMI patients was performed concerning clinical features,invasive and medical management and subsequent follow-up.
Statistical analysis
Data are shown as median (interquartile range) for continuous variables,and number(percentage) for categorical data.Student'st-test,Mann–WhitneyUtest,Fisher's exact test,andχ2test were used,as appropriate.APvalue <0.05 was considered statistically significant.Survival curves including the log-rank test for STEMI and NSTEMI patients were built.Statistical analyses were performed with SPSS Statistics Version 23(IBM,United States).The statistical methods used in this study were reviewed by our expert Biostatistician Eraldo Occhetta.
RESULTS
Baseline patients’ characteristics are shown in Table 1.Of the 105 patients enrolled,68(64.8%) were admitted for NSTEMI and 37 (35.2%) for STEMI (Figure 1).The mean age of these patients was 83.9 ± 3.6 years.
Patients presenting with STEMI were more likely to receive an invasive treatment:34 (91.9%) underwent coronary angiography and all of them were treated with percutaneous revascularization;among the NSTEMI patients,42 (61.8%) underwent coronary angiography and 16 (38.1%) of them had a percutaneous angioplasty performed (Table 2 and Figure 2).The most common reasons for revascularization not being performed in this subgroup of patients were non-obstructive coronary artery disease,small target vessels inappropriate for intervention,extensive three vessel disease without a “culprit lesion” identified and associated severe valvular disease.The most common reason for coronary angiography not being performed in 38.2% of patients,instead,was the perception of the absence of a net clinical benefit by the treating physicians considering the global risk/benefit ratio.
Twenty-five patients (23.8%) had AF either before or as new onset during the index hospitalization that required specific treatment with oral anticoagulation.No significant difference was found between NSTEMI and STEMI patients concerning the history or new onset of AF.
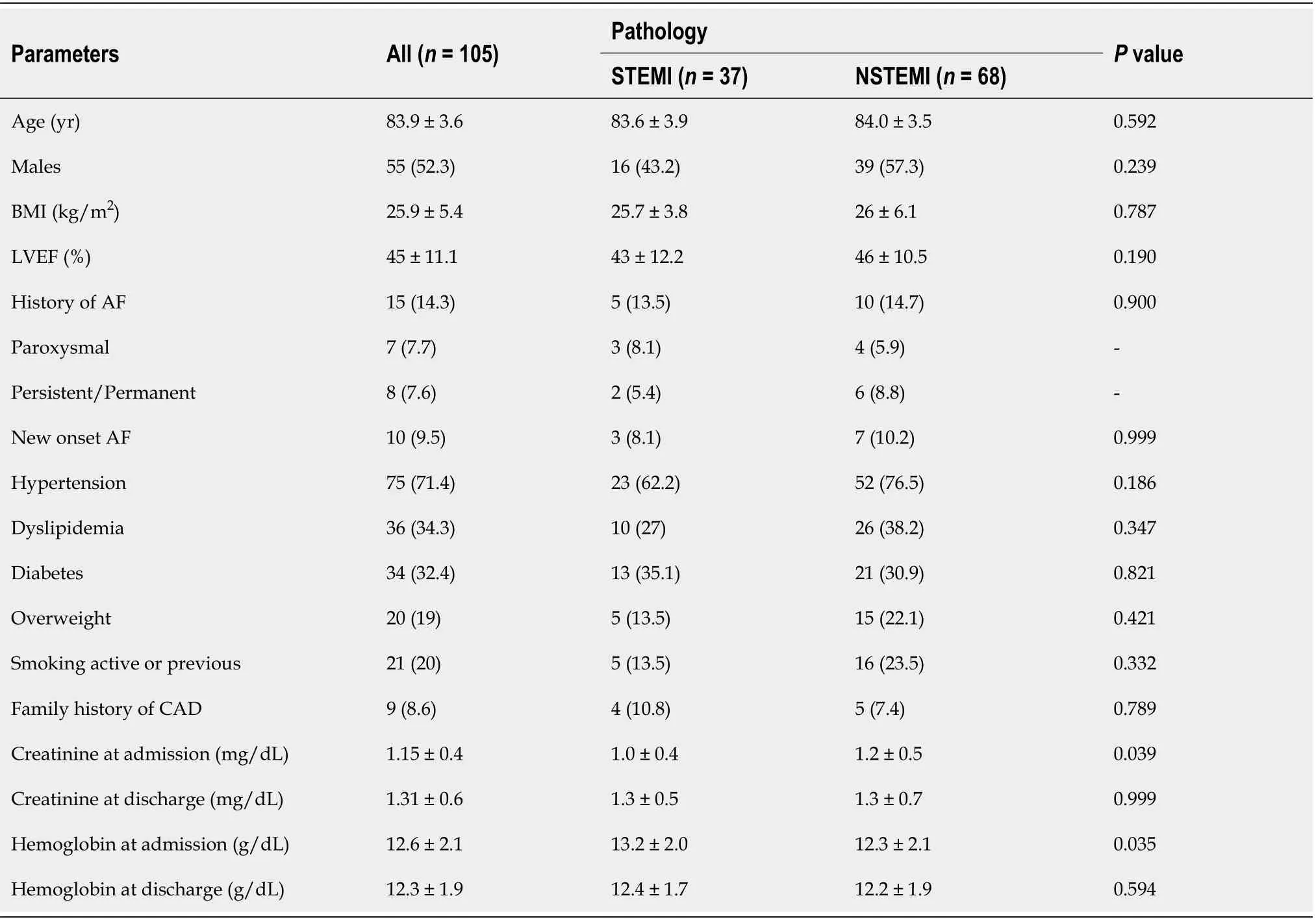
Table 1 Baseline patients’ characteristics,n (%)
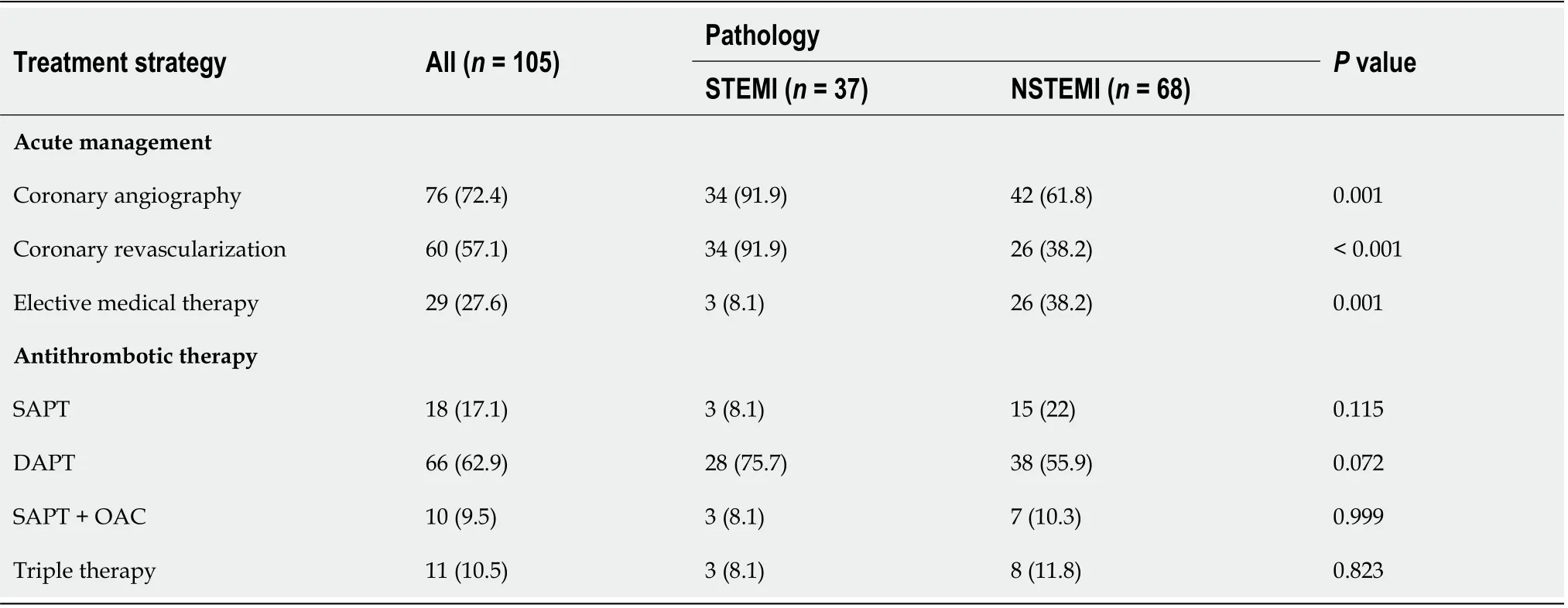
Table 2 Acute management and antithrombotic therapy,n (%)
With regard to antithrombotic medications:8.1% of STEMI patients and 22% of NSTEMI patients received a single antiplatelet therapy;75.7% of STEMI patients and 55.9% of NSTEMI patients were treated with DAPT;8.1% of STEMI and 10.3% of NSTEMI were treated with single antiplatelet therapy plus antithrombotic therapy(VKAs or DOACs);8.1% of the STEMI group and 11.8% of the NSTEMI group were treated with DAPT plus anticoagulant therapy (VKAs or DOACs) (Table 2).Following statistical analyses,STEMI patients,as compared with NSTEMI patients,showed a trend towards a higher rate of DAPT administration.
Values of serum creatinine varied significantly from admission to discharge,in STEMI but not in NSTEMI patients,while a trend towards significance was found for hemoglobin;these differences may likely reflect the higher percentage of the invasive strategy in the former group.
During hospitalization,6 (5.7%) patients (3 in the NSTEMI and 3 in the STEMI group) died,all due to cardiovascular causes.One major bleeding complication(hematoma at the femoral access site) and 2 minor bleeding complications occurred.
After hospital discharge,9 patients were lost to follow-up.For the remaining 90 patients,the mean follow-up was 11.1 ± 7.2 mo.Table 3 summarizes the main outcomes.
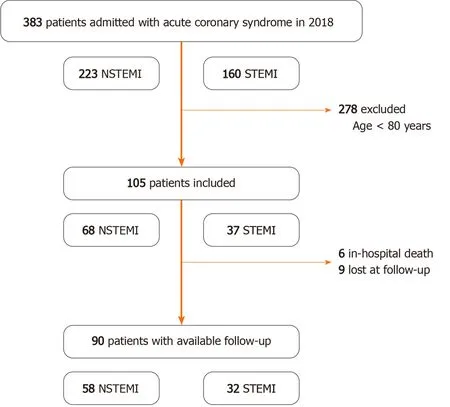
Figure 1 Study flow-chart.
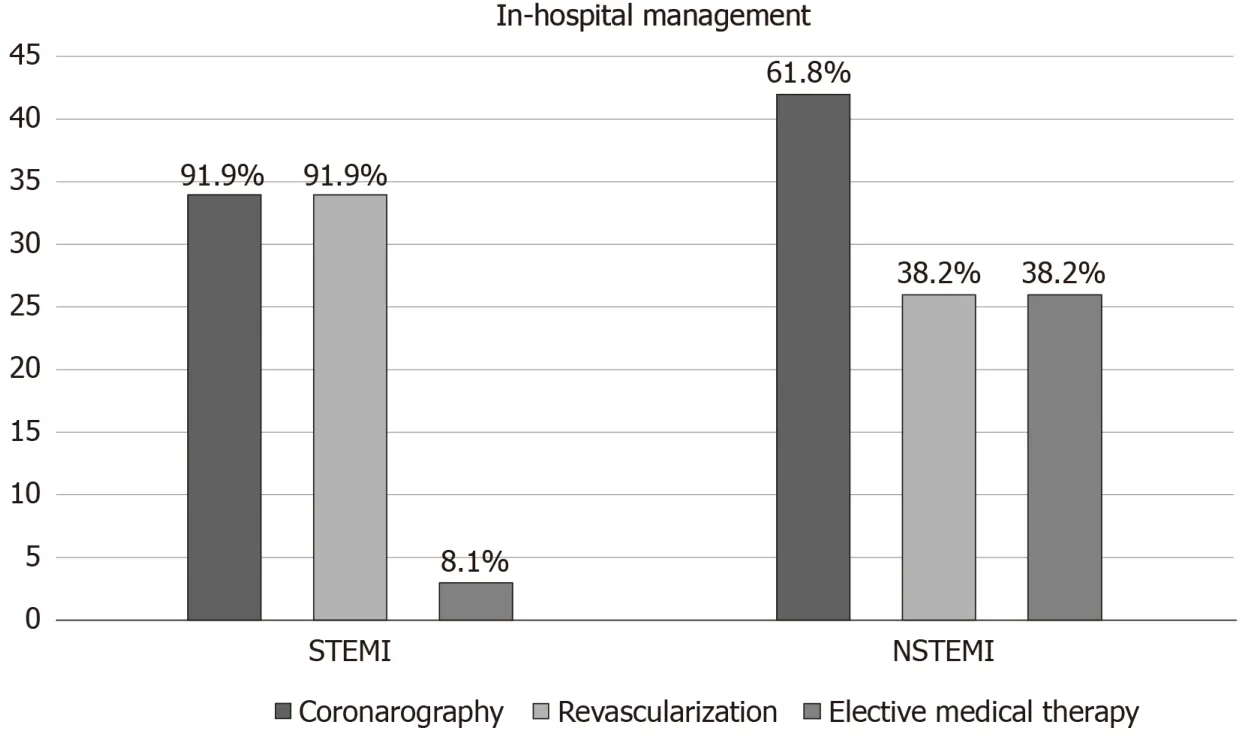
Figure 2 In-hospital patient management.
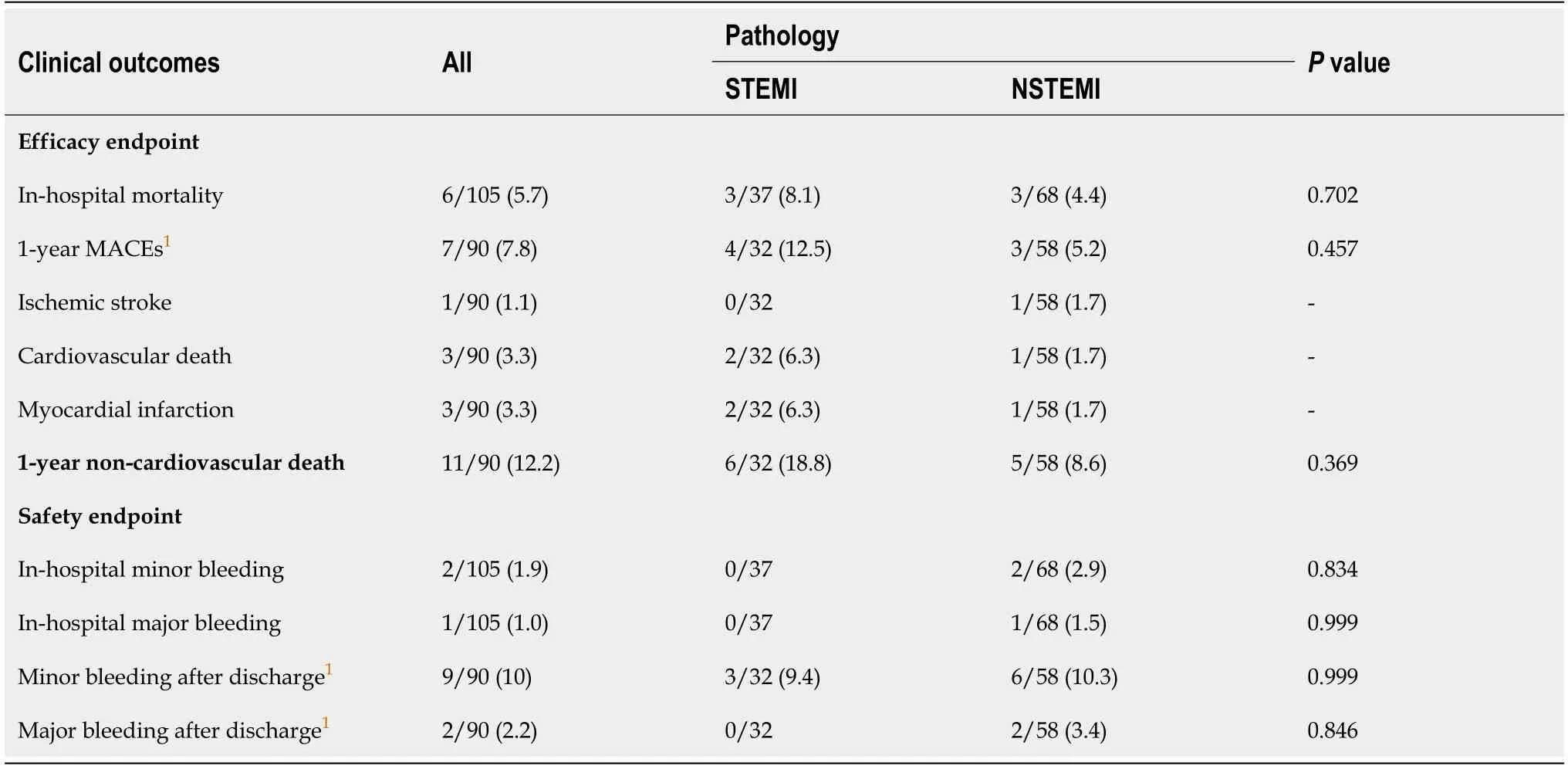
Table 3 Clinical outcomes,n (%)
MACEs were recorded in 7 patients (7.8%).Only 3 patients (3.3%) experienced cardiovascular death,while 11 patients (12.2%) died of non-cardiovascular causes,mainly due to malignancy,pneumonia or sepsis.No deaths attributable to bleeding complications were recorded.
No significant difference was found between NSTEMI and STEMI patients concerning the incidence of all-cause death or any event during hospitalization or follow-up (Figure 3 and Table 3).
Concerning the safety endpoint,2 patients experienced a major non-fatal spontaneous bleeding event at follow-up:One of them was on DAPT,the other was on triple antithrombotic therapy.Minor bleeding was reported in 9 patients (10%).Even if no specific antithrombotic strategy significantly correlated with the safety endpoints,all patients who experienced bleeding were taking DAPT or dual/triple antithrombotic therapy.The hemorrhagic risk estimated through the PRECISE-DAPT score [median value 35 (IQR 29-40)] did not correlate with the incidence of minor or major bleeding events (P= 0.602);however,as specified,this score was retrospectively calculated and was not used to determine the duration of DAPT.
DISCUSSION
In this retrospective registry of elderly patients admitted to our division due to myocardial infarction,we describe our in-hospital management of this population,and report a low incidence of complications in the short and medium-term follow-up.
Available data to guide the management of elderly patients are limited,both because they are underrepresented in Acute Coronary Syndrome registries (27%–34%)and randomized controlled trials (RCTs) (13%-15%)[13-15],and because,due to a selection bias,RCTs may not be representative of the population treated in everyday clinical practice[1,2].It is known that the atypical clinical and ECG presentation and the lower specificity of troponin assays may delay the diagnosis[16,17].In registries,elderly patients are less likely to receive evidence-based therapies and undergo an invasive strategy compared with younger patients[13].Therefore,focusing on this subgroup is of particular interest for two main reasons.Firstly,with the aging of the population,the elderly represent a growing number of patients presenting with myocardial infarction.Moreover,age is a very important prognostic factor:Patients over 75 years account for 60% of the entire mortality due to cardiovascular diseases and they are often more subject to infarct-related complications such as heart failure and pulmonary edema,which occur in more than half of patients over 75 years and in 65% of patients over the age of 85;shock occurs in more than 10% of patients over 75 years and is mainly due to rupture of the left ventricular free wall or papillary muscles or to advanced ventricular dysfunction[2,18].
In our real-world cohort,the mean age was 83 years,higher than that reported in previous studies[19,20].A tailored therapeutic approach based on a comprehensive evaluation of the patient’s status and comorbidities proved successful as we report a rate of adverse events at follow-up lower than previous studies[21,22](Table 4).Since the available evidence differs between NSTEMI and STEMI elderly patients,we differentiated these populations,reporting data for each subgroup.
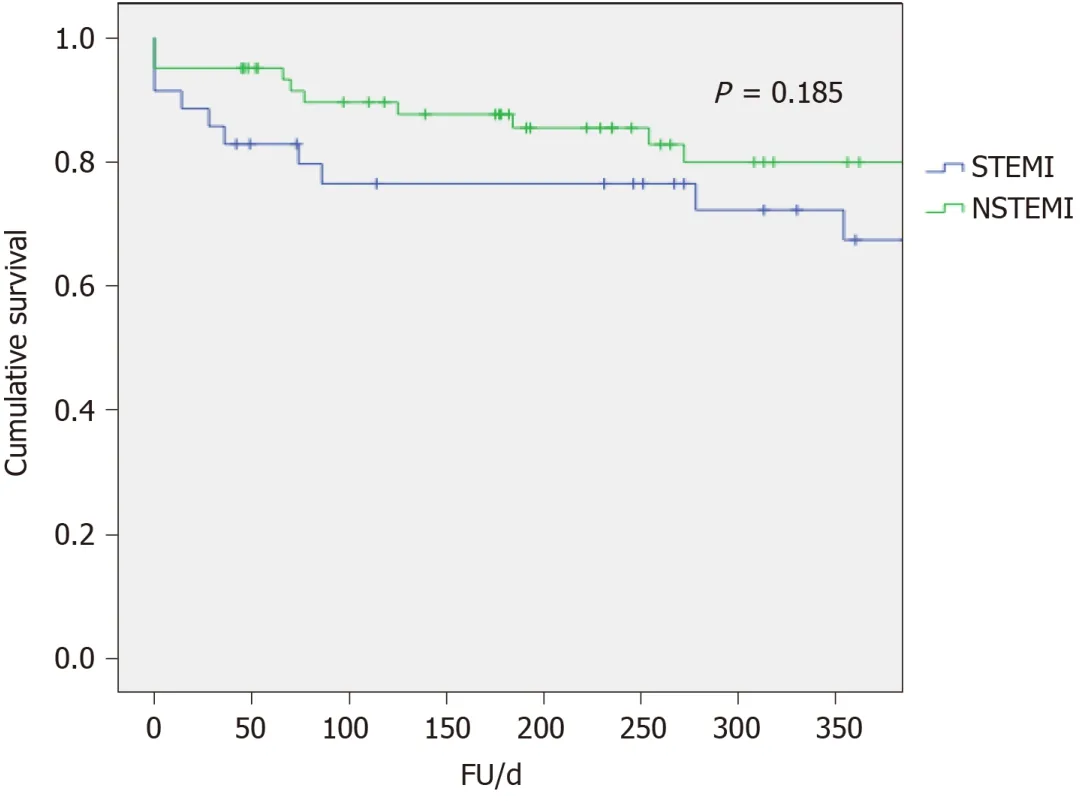
Figure 3 Kaplan-Meier curves of all-cause death.
Revascularization in NSTEMI
European clinical practice guidelines on non-ST elevation acute coronary syndrome(NSTE-ACS) state that elderly patients should be considered for an invasive strategy and emphasize the need for a detailed clinical evaluation including comorbidities,life expectancy,quality of life,frailty and patient preferences,in order to individualize the risks and benefits[3].However,no specific recommendation is available to guide therapeutic decisions based on these parameters.
With regard to NSTEMI in the GRACE registry,coronary angiography was performed in 67% of patients <70 years of age compared with 33% in patients over 80 years[21,22].Similar percentages were observed in the CRUSADE experience (coronary revascularization performed in 40.1% of patients 75–89 years of agevs12.6% in those ≥90 years)[23,24],in the SWEDEHEART experience[25]and in the Euroheart ACS survey[13].In our experience,the percentages were higher than those reported in previous studies.In fact,61.8% of NSTEMI patients greater than 80 years underwent coronary angiography and of these 61.9% underwent percutaneous revascularization.Nagataet al[19]adopted an invasive strategy in 94% of NSTEMI but reported high rates of inhospital mortality (8.5%) in patients >80 years of age.
Whether acute revascularization is the best strategy for these patients is still a matter of debate.In the FRISC II-ICTUS-RITA-3 study,the invasive therapeutic strategy performed better in elderly NSTE-ACS patients than in younger patients[26].On the contrary,Sanchiset al[27]and García-Blaset al[28]showed that invasive management did not modify long-term outcome in comorbid elderly patients with NSTEMI.The Italian-ACS trial included 313 NSTE-ACS patients over 75 years and found no significant benefit of the routine invasive strategy in a composite primary endpoint including ischemic and bleeding events,when compared to selective invasive strategy[6].On the other hand,the After Eighty trial (457 NSTE-ACS patients ≥80 years) showed a significant benefit of the routine invasive strategy in the composite primary ischemic endpoint compared to the conservative strategy[29],although only 457 patients were included out of 4187 screened and the included population may not reflect the whole spectrum of elderly patients.In a meta-analysis of four RCTs comparing routine invasive strategy with a selective invasive strategy,including 1887 patients (mean age 79 years) no significant difference in all-cause death,cardiovascular death or major bleeding was found between both strategies at a median 36-mo followup[30].
The prognostic impact of revascularization in our patients would be difficult to assess due to the retrospective nature of the study design.Within this context,evidence from the literature and clinical practice shows that a routine early invasive strategy is not always the most favorable,because similar results may be obtained with a medical conservative strategy.
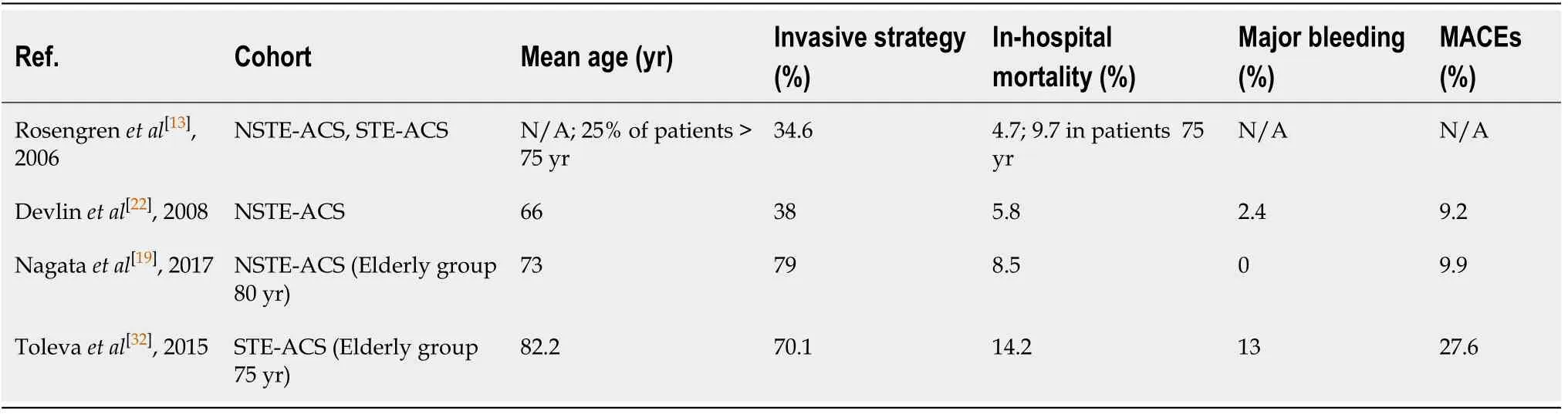
Table 4 Comparison of observational studies including elderly patients with acute coronary syndrome
Revascularization in STEMI
Despite the lower rate of revascularization in the elderly,its benefit appears to be maintained at an older age in this context[7].There is no upper age limit with respect to reperfusion,especially with primary percutaneous coronary intervention (PCI)[31].Observational studies have shown that coronary reperfusion therapy (thrombolysis or PCI) also during STEMI is little used in older age,with a trend directly correlated to age (64.8% between 65 and 69 years,60.1% between 70 and 74 years,50.4% between 75 and 79 years,35.4% between 80 and 84 years,20.4% >85 years)[32].A possible explanation for this is the paucity of data on reperfusion in the elderly with STEMI,the presence of atypical symptoms and the related diagnostic and therapeutic delay and comorbidities[18].In our hospital 91.9% of STEMI patients underwent coronary angiography and primary PCI.
Antithrombotic therapy
The optimal therapy after STEMI and NSTEMI acute treatment is well codified by the actual ESC guidelines[33].In addition,anticoagulant therapy association in AF patients(triple therapy) has recently been confirmed in a Joint European Consensus[34].One of the reasons for suboptimal administration of evidence-based medications in the elderly is that patients may more frequently have contraindications to medications or pharmacodynamic characteristics (absorption,metabolism,distribution and excretion of drugs) that make them prone to medication side effects[1,2].In particular,they have an augmented bleeding risk due to aging,impaired renal function and comorbidities.Observational studies have shown frequent excess dosing of antithrombotic therapies in elderly patients:In this context,lower doses of DOACs could avoid these risks[35,36].Moreover,personalized therapeutic choices between dual and triple antithrombotic therapy for concomitant AF may improve benefits and reduce risks in frail and elderly patients[37,38].Our population presented a high hemorrhagic risk as shown by the median values of the PRECISE-DAPT score;however,with a tailored therapeutic approach we found a low rate of significant bleeding even in those treated invasively.
In conclusion,the authors of this article acknowledge that specific guidelines on the management of elderly patients with ACS are lacking,yet these patients tend to present with various comorbidities,often associated,and exploring every specific scenario in order to standardize clinical management would be impractical.
Trials necessarily restrict enrollment criteria and tend to exclude extreme ages or patients with comorbidities due to the heterogeneity of their clinical presentation.
We therefore present a small cohort of patients showing what is likely to be a common scenario in a cardiology ward.We do believe that,in such a complex context,the approach to treatment should be tailored to the patient:Even if a thorough knowledge of the scientific evidence is essential,physicians need to draw on experience and common sense.
Limitations of the study
Our study has some limitations.First of all,due to the limited sample size studied,our comparison between STEMI and NSTEMI patients does not have adequate statistical power (90%) for all the results reported (though keeping in mind the limits of a posthoc power analysis),which therefore need to be interpreted with caution.
Moreover,the retrospective design of the study did not allow a more comprehensive evaluation of patients through a “frailty” assessment that may be useful in the context studied.Moreover,as the PRECISE-DAPT score values were retrospectively calculated,we could not assess its impact in guiding DAPT duration in order to reduce bleeding events.Observational studies,despite their methodological limitations,may reflect evidence closer to the real-life population.Indeed,our study was conceived to describe our real-world practice in elderly patients with acute myocardial infarction and provide information on the management and outcome of this disease in the aging society.
CONCLUSION
In this observational study,we describe data from a real-world setting of elderly patients hospitalized with acute myocardial infarction,and report low in-hospital mortality and a low rate of medium-term ischemic and hemorrhagic complications.
Although the available evidence does not allow us to establish firm recommendations in this subgroup of patients,we report that an invasive strategy in selected cases and an adequate antithrombotic therapy,even in this critical context,can be safely performed.Measures to reduce complication rates in this population include an accurate selection of patients suitable for an invasive strategy,evaluating the presence of comorbidities,a radial access whenever possible and correct dosing of antithrombotic drugs.
Larger registry cohorts with a higher number of patients enrolled are mandatory to study the setting of elderly patients with acute coronary syndromes.
ARTICLE HIGHLIGHTS
Research background
Despite the aging of the population,which makes the clinical presentation of elderly patients with acute myocardial infarction more common,there are no specific guidelines on the management of this subgroup and data are generally extrapolated from trials in which elderly patients represent a minority of the cohort studied.Indeed,controversy exists both on the need for an invasive strategy,especially in frailer patients,and on the optimal medical management.
Research motivation
Exploring and describing the setting of elderly patients with myocardial infarction is particularly useful to identify aspects that need to be improved and sources of mistakes in everyday clinical practice.
Research objectives
In the present real-world study on a population of elderly patients hospitalized due to an acute myocardial infarction,we aimed to investigate our practice during in-hospital time and outcomes during the first year of follow-up.
Research methods
We retrospectively analyzed all consecutive patients older than 80 years admitted to the Division of Cardiology of our center in 2018 for acute myocardial infarction.Clinical and laboratory data were collected.In-hospital management,consisting of an invasive or conservative strategy,and the anti-thrombotic therapy used were described.Outcomes evaluated at 1 year follow-up included an efficacy ischemic endpoint and a safety bleeding endpoint.
Research results
We enrolled a total of 105 patients with a mean age was 83.9 ± 3.6 years.Patients presenting with ST-elevation myocardial infarction (STEMI) (35%) received an invasive treatment in more than 90% of cases,while the number of patients with non-ST-elevation myocardial infarction (NSTEMI) (65%),who underwent coronary angiography and percutaneous angioplasty was lower (38%).Coronary angiography was not performed when the absence of a net clinical benefit was perceived by the treating physicians considering the global risk/benefit ratio,while coronary angioplasty was not performed mainly due to the absence of an obstructive coronary artery disease or technical reasons.Atrial fibrillation,either before or as new onset during the index hospitalization,was found in 24% of patients.With regard to antithrombotic medications,10.5% of the whole population received triple antithrombotic therapy and 9.5% single antiplatelet therapy plus oral anticoagulation(OAC),with no significant difference between the subgroups,although a higher number of STEMI patients received dual antiplatelet therapy without OAC as compared with NSTEMI patients.A low rate of in-hospital death (5.7%) and 1-year cardiovascular death (3.3%) was registered.Major adverse cardiovascular events were recorded in 7 patients (7.8%).Interestingly,11 of 14 deaths at one-year follow-up were the result of non-cardiovascular causes,mainly due to malignancy,pneumonia or sepsis.No deaths attributable to bleeding complications were recorded,while only 2 patients experienced a major non-fatal spontaneous bleeding event at follow-up.
Research conclusions
The authors of this article acknowledge that specific guidelines on the management of elderly patients with acute coronary syndrome are lacking,yet these patients tend to present with various comorbidities,often associated,and exploring every specific scenario in order to standardize clinical management would be impractical.Trials necessarily restrict enrollment criteria and tend to exclude extreme ages or patients with comorbidities due to the heterogeneity of their clinical presentation.We therefore present a small cohort of patients showing what is likely to be a common scenario in a cardiology ward.We do believe that,in such a complex context,the approach to treatment should be tailored to the patient:Even if a thorough knowledge of the scientific evidence is essential,physicians need to draw on experience and common sense.Through this approach,the rate of complications and death was relatively low in our population.The main limitation of this study,namely its retrospective nature,is somehow a point of strength,as it avoids selection biases which characterize previous studies.
Research perspectives
Future studies on the elderly population should be based on a registry design.Larger studies with a higher number of patients enrolled are mandatory.
 World Journal of Cardiology2020年11期
World Journal of Cardiology2020年11期
- World Journal of Cardiology的其它文章
- Endothelial progenitor cells mobilization after maximal exercise according to heart failure severity
- Rapid right ventricular pacing for balloon valvuloplasty in congenital aortic stenosis:A systematic review
- Effects of left ventricular assist device on pulmonary functions and pulmonary hemodynamics:A meta-analysis
- Medical therapy vs early revascularization in diabetics with chronic total occlusions:A meta-analysis and systematic review
- Transradial vs transfemoral secondary access outcomes in transcatheter aortic valve implantation:A systematic review and meta-analysis
- Cardiac adverse events of immune checkpoint inhibitors in oncology patients:A systematic review and meta-analysis
