Preliminary evaluation of the radiotherapeutic efficacy of 131I-atorvastatin in rats with hepatocellular carcinoma
Nourihan S. Farrag· Abeer M. Amin
Abstract As one of the most critical types of cancer,hepatocellular carcinoma (HCC) affects many people worldwide.This study demonstrated the prospective use of atorvastatin, a drug that inhibits the mevalonate pathway,causing hypolipidemia, as a carrier to deliver the iodine-131 (131I) isotope to liver tissues for HCC radiotherapy.The atorvastatin radioiodination method was optimized for utilizing the 131I isotope.The radiochemical quality and the in vitro stability of the generated [131I]atorvastatin were investigated.In addition,the biodistribution experiments of[131I]atorvastatin were evaluated in both normal and HCCinduced rat models. [131I]atorvastatin was produced at a maximum radiochemical yield of 86.7 ± 0.49%. The[131I]atorvastatin solution purified via high-performance liquid chromatography showed good in vitro stability for 12 h after tagging. Biodistribution analyses revealed remarkable liver targeting capacity of[131I]atorvastatin and good localization of 131I in liver tissues. Overall, the encouraging biochemical profile and histopathological findings have been reported,and preliminary investigations on the possible use of[131I]atorvastatin as a radiotracer and its impact on HCC radiotherapy in rats show promise.
Keywords Hepatocellular carcinoma · [131I]Atorvastatin ·Biodistribution · Radiotherapy
1 Introduction
The liver is an active metabolic organ that is easily influenced by many environmental conditions [1]. Hepatocellular carcinoma (HCC) is ranked as the third most prevalent cause of cancer-related deaths globally [2, 3].Environmental agents play a dominant role in causing HCC.Exposure to hepatitis B and C viruses are among the most common causes leading to HCC [4]. Other risk factors of HCC include consumption of alcoholic drinks,aflatoxins, diabetes mellitus, and nonalcoholic hepatic steatosis disease,as well as immune-related factors such as autoimmune hepatitis and primary biliary cirrhosis [5, 6].
Despite the presence of different novel treatment options, including cryo-surgery, radio-frequency thermal ablation, and chemo-embolization, the management of patients with severe HCC has remained difficult. Therefore, it is extremely necessary to develop appropriate therapeutic approaches [7]. Radiotherapeutic strategies have been chosen to control tumor growth during the progressive stages of HCC [6]. Radiotherapy can be classified into either internal (IR) or external beam radiotherapy (EBR). EBR can be used solely for tumor growth control or, in most cases, together with chemotherapy.Such combination has not succeeded in therapeutic trials;even so, this combination may still have a positive impact on the tumor. A better way is to target the affected part of the liver via radiation [2]. IR is achieved by delivering radioisotopes to the site of interest through different administration routes. The ideal criteria of the radioisotopes used in IR include: a short half-life, beta (β) ray emission for therapeutic purpose, and a small fraction of gamma(γ)ray emission which is necessary for verification.The most commonly used isotopes are Yttrium-90 (90Y),131I, and Holmium-199 (199Ho).90Y is a pure β-emitter with a physical half-life of 2.7 days.It has been introduced by intratumoral injection of90Y-glass microspheres[6,8,9]or via a transarterial strategy.131I,a mostly β-and a little γ-emitter, with a half-life of 8 days [10], was used as131I-lipiodol[11,12].199Ho,also mostly a β-ray emitter with little γ emission, with a half-life of 26.8 h, has also been evaluated in a chitosan complex form and was administered either intratumorally or via a transarterial approach [13, 14].
Atorvastatin (ATV) is a drug that inhibits hydroxymethylglutaryl coenzyme A (HMG-CoA) reductase, the enzyme that catalyzes the rate-limiting step of the cholesterol biosynthetic pathway. ATV is among the most frequently prescribed drugs worldwide [15] for the treatment of hypercholesterolemia.ATV is localized in the liver as its target organ [16] and inhibits HMG-CoA reductase. ATV not only competes with the enzyme’s active site but also changes its conformation, making the enzyme fail to perform its main function. Additonally, the change in conformation at the active site makes ATV very effective and specific [17]. Previously, statins have been introduced as potential agents for cancer therapy [18–21]. Furthermore,ATV has other biological properties [22] such as anti-inflammatory, antiproliferative, antioxidant, and anti-apoptotic activities [23–25].
Considering the liver targeting ability of ATV,this work was designed to explore the localization and radiotherapeutic efficacy of [131I]atorvastatin in HCC-induced rat models. Therefore, ATV radiolabeling processes with131I isotope were optimized to deliver this radionuclide to rat livers for the radiotherapy of HCC.
2 Experimental
2.1 Materials and animals
ATV and chloramine-T (CAT) were ordered from Sigma-Aldrich, Homburg, Germany. The rest of the chemicals used were reactive reagents. No-carrier-added131I (nca Na131I, 3.7 GBq/ml diluted with 0.1 N NaOH)was kindly received from the Radioisotope Production Facility, RPF, EAEA, Cairo, Egypt.
Male albino rats (150 ± 5 g) were collected from the Animal House of Nuclear Researches Center, EAEA,Cairo, Egypt and fed a normal rodent diet. Animals were housed under 12 h of light and 12 h of darkness per day in the animal care unit and maintained at 24–28 °C with relative humidity of 60–70%and water given ad libitum.In a separate, lead-shielded animal shelter, the animals that received [131I]atorvastatin were housed. All animal-related procedures were conducted according to the regulations defined by Animal Ethical-Committee of EAEA.
2.2 Methods
2.2.1 Optimization of [131I]atorvastatin preparation
ATV was electrophilically substituted by the131I isotope for radiolabeling in the subsistence of CAT as an associate oxidizer. Various parameters (ATV amount, CAT amount,reaction mixture pH, reaction temperature, and reaction time) which influence the reaction were optimized to prepare [131I]atorvastatin. Briefly, different volumes of ATV methanol solution (1 mg/ml), Na131I solution (10 μl,3.7 MBq), and different volumes of freshly prepared CAT methanol solution (1 mg/ml) were added successively into a tightly screw-capped brown vial. The pH of the reaction solution was adjusted to a wide range of values (2–11)thereafter. The mixtures were completed to the same final volume using double distilled water (DDW) and stirred with a vortex generator for 1 min. After that, the mixtures were incubated at different temperatures ranging from ambient temperature (25 ± 5 °C) up to 100 °C for different reaction times (5–60 min). Finally, the reactions were terminated after the addition of an aqueous solution of sodium metabisulfite (50 μl, 20 mg/ml) and subsequent vortex stirring was performed for 2 min [26].
2.2.2 Radiochemical yield assay
An [131I]atorvastatin radiochemical yield assay was conducted using thin layer chromatography (TLC, silica GF254plates backed by aluminum). The plates were cut into strips of 1 × 13 cm. At a point 2 cm from one end,5 μl of each sample was added and left to dry.The solvent,a homogenous mix of chloroform:ethanol in a ratio 9:1 v/v,was allowed to reach 10 cm from the origin. After drying,the strips were cut into small segments with dimensions of 1 cm by 1 cm each. A well-type NaI gamma-counter,Scaler-Ratemeter SR-7 (Nuclear Enterprises LTD, USA),assessed radioactivity in each segment. [131I]atorvastatin moved with the solvent front and free iodide (131I-)remained at the point of application. The radiochemical yield was calculated by dividing radioiodinated compound activity over the total activity multiplied by 100,according to Eq. (1) [27, 28]:
2.2.3 Radiochemical purity assay of [131I]atorvastatin
The radiochemical purity of the freshly prepared [131-I]atorvastatin compound was analyzed via high-performance liquid chromatography (HPLC). HPLC of inactive ATV, radiotracer [131I]atorvastatin, and free iodide were performed using a Shimadzu-model (Kyoto, Japan) detector SpD-6A,with the column RP-C18,250 mm × 4.6 mm,5 μm, and LiChrosorb as a stationary phase. A sample volume (10 μl) was injected and a mixture of DDW and acetonitrile (15:85, v/v) in a medium of pH 4.5 (adjusted with phosphoric acid) that was adjusted by adding phosphoric acid, was utilized as an eluent in the isocratic strategy. The rate of fluid flow was adjusted to 1 ml/min,and the UV detector was adjusted to a wavelength of 261 nm [29]. A refractive index detector was used in combination with a NaI gamma scanner detector for monitoring131I-activity.
2.2.4 Stability of [131I]atorvastatin in vitro
The HPLC-purified[131I]atorvastatin obtained under the optimized reaction conditions was placed at ambient temperature to observe its radiolabeling stability in vitro. The mixture was incubated for 1 day. Stability was evaluated using the TLC method as described before [28], and the result was expressed as percentage of radioactivity of[131I]atorvastatin relative to all radioiodine activity.
2.2.5 HCC induction in rats
Diethyl-nitrosamine (DENA) or N-nitrosamine-related compounds are considered as animal hepatocarcinogens[30]. DENA is commonly used to initiate cancer in HCC induction experiments, whereas other factors such as carbon tetrachloride (CCl4) are introduced as promoters of carcinogenesis [31, 32].
Pure DENA was dissolved in a physiological saline solution (0.9% sodium chloride) and intraperitoneally administered to every rat in a single injection of 200 mg/kg bodyweight [33]. Two weeks later, CCl4was subcutaneously injected into the animals at a dosage of 3 ml/kg bodyweight once a week for six weeks to boost the carcinogenicity of DENA [34]. At the end of the HCC induction cycle, the animals were made to fast overnight,were anesthetized, and euthanized. Blood samples were then collected,centrifuged at 3000 rpm for 15 min,and the sera carefully isolated and preserved at-20 °C for further biochemical analyses. Hepatic tissue was fixed in 10%buffered formalin and prepared for histopathological examination.
2.2.6 In vivo radio pharmacokinetic evaluation of [131I]atorvastatin in normal and HCC-bearing rats
In this study, two groups of animals, normal rats and HCC-induced rats(five rats for each time point,total of 20 rats per group), were used. The two groups received intravenous injections of 0.2 mCi [131I]atorvastatin(200 μl) to determine the biodistribution of the radioiodinated compound at 1,2,4 and 8 h post injection(p.i.) The rats did not receive inactive iodine prior to the experiment.Thereafter, the injected rats were anesthetized by chloroform and were euthanized. Organ and tissue samples(blood,bone and muscle)were isolated,weighed,counted,and claimed to be 7, 10, and 40 percent of the overall weight, respectively [35]. Next, the heart, liver, spleen,lungs,kidneys,intestine,stomach,and thyroid glands,were excised,washed with normal saline,and weighed carefully.Radioactivity uptake in these organs was then measured using a gamma counter. The radioactivity concentration in the organs and body fluids were reported as percent injected dose per gram (%ID/g).
2.2.7 Radiotherapeutic efficacy of [131I]atorvastatin on rats with HCC
A maximum of ten rats with HCC were divided randomly into two groups(treatment group and control group)to evaluate the radiotherapeutic efficacy of [131I]atorvastatin. A dose of 0.1 ml [131I]atorvastatin (5 mCi/day) was injected intravenously into the tail vein of each rat as a bolus dose for 3 days.The control group received 0.1 ml of 0.9% sodium chloride intravenously for comparison. The rats were then anesthetized after treatment and euthanized.The blood samples and liver tissues were collected as described before.
2.2.8 Statistical analysis
SPSS software was used to conduct all statistical analyses (version 20; SPSS Inc., Chicago, IL). Values are expressed as the mean ± standard deviation of three independent optimization processes for radiolabeling experiments and five independent biological studies experiments. The statistical analysis between groups was carried out using one-way ANOVA.A p value <0.05 was considered to be statistically significant.
3 Results and discussion
3.1 Radiochemistry
ATV(100 μg)was radiolabeled with131I isotope via an electrophilic substitution reaction after oxidizing radioiodide (131I-) to iodonium ion using 100 μg of CAT. The reaction mixture, adjusted to be of neutral pH, was incubated at ambient condition for 30 min. The maximum radiochemical output of the prepared[131I]atorvastatin was 86.7 ± 0.49%.
Figure 1 illustrates the chemical scheme of [131I]atorvastatin radiolabeling which was unambiguously determined by Moustapha et al. [36] by synthesizing the127I analog. Moreover, the synthesized [127I]atorvastatin was interpreted using elemental analysis, mass spectrometry,and proton-NMR strategies [36].
The radioiodination of ATV, the influence of ATV amount, CAT amount, pH of the medium, incubation temperature, and incubation time on the radio yield of[131I]atorvastatin were systemically altered to optimize the radioiodination conditions.
As shown in Fig. 2, when the amount of ATV was increased from 50 μg to 100 μg, the radio yield increased from 66.5 ± 0.41% to 86.7 ± 0.49%, respectively. It was found that any further increase in the amount of ATV was accompanied by a notable decrease in the radiochemical yield, thereby demonstrating that 100 μg of ATV was enough to capture all of the released iodonium cations[37].Alternatively,it may be due to the fact that the molarity of ATV exceeded the molarity of iodonium cations in the solution [38]. In addition, upon increasing the amount of ATV, solubility becomes an important factor [39]. An increase in ATV concentration may lead to insufficient solubility, which made the radiolabeling process difficult,consequently leading to a decrease in the radio yield [39].
Figure 3 shows that by using CAT as an oxidizing agent,radiochemical yield increased with increasing CAT concentration until it reached 86.7 ± 0.49%,when the amount of CAT was 100 μg. Furthermore, it was noticed that the radiochemical yield decreased with any further increase in CAT amount, which is explained by the genesis of oxidative byproducts.
The radiochemical yield, as shown in Fig. 4, depended heavily on the pH of the reaction solution. By increasing the pH up to 7, the radioiodination rate was obviously improved. Subsequently, it decreased with a further increase in the pH value;thus the peak radiochemical yield of[131I]atorvastatin(86.7 ± 0.49%)was reached at around pH 7.This might be explained by the fact that by producing HOI species, CAT functions well as an oxidizer in neutral media [40]. It might also be associated with the improved stability of the[131I]atorvastatin and the good performance of the direct radioiodination processes at pH 7.
The influence of incubation temperature on the radio yield of[131I]atorvastatin was also investigated.The results are shown in Fig. 5 and seem to suggest that ambient temperature (25 ± 5 °C) has the highest impact on the radiochemical yield of[131I]atorvastatin,which reached its maximum value of 86.7 ± 0.49%.It was found that raising the reaction temperature above the ambient temperature led to a lowering of the radio yield of[131I]atorvastatin,which shows that [131I]atorvastatin had poor stability at elevated temperatures.
Additionally, it is evident in Fig. 6 that incubation time substantially influences the radio yield of[131I]atorvastatin,where the highest value(86.7 ± 0.49%)was achieved after incubation for 30 min.
Analysis of [131I]atorvastatin via HPLC illustrated that ~85% of131I binds with ATV (Fig. 7), forming a single labeled compound. The retention time for inactive ATV was 6 min, the retention time for [131I]atorvastatin was 9 min, whereas the retention time for free131I-was 3 min. [131I]atorvastatin-containing fractions were eluted,pooled together, evaporated to dryness, and dissolved in physiological saline. Finally, the [131I]atorvastatin solution was filtered through a Millipore filter (0.22 μm) and used in biodistribution studies.
The in vitro stability of HPLC-purified[131I]atorvastatin was evaluated upon incubation at ambient temperature up to 24 h. It is important to note that the percentage of radioactivity of[131I]atorvastatin relative to all radioiodine activity was 99.8 ± 0.08% and 99.5 ± 0.09% at 1 and 12 h post labeling, respectively. [131I]atorvastatin deiodinated at a much slower rate over time, implying its good stability up to 12 h (Table 1). It is worth mentioning that,although the radioactivity percentage of [131I]atorvastatin(98.7 ± 0.31)significantly differed from the others at 24 h,it indicated a good stability of the radio-labeled compound.The in vitro stability of the [131I]atorvastatin enabled it to be used as a radiotracer for cancer therapy.
3.2 Animal experiments
Serum aspartate-transaminase (AST) and alaninetransaminase(ALT)are the prime enzyme biomarkers used to observe hepatic constitutional function and injury, and they also assists in the identification of hepatotoxicity[41].Additionally,alpha fetoprotein(AFP)is the most prevalent tumor marker applied in HCC screening [42].Elevation of AFP grade denotes poor prognosis in contrast to the low AFP grades [43, 44]. The reference values of AST, ALT,and AFP are 50–150 IU/L, 10–40 IU/L, and 2–20 ng/ml,respectively [45]. As shown in Table 2, the group that received DENA/CCl4demonstrated a significant rise in the biochemical markers ALT,AST,and AFP when compared to the negative control group as well as to the normal values.

Table 1 The stability of[131I]atorvastatin in vitro
Histological analysis (Fig. 8) showed that low-grade HCC was composed of moderately pleomorphic cells with prominent nucleoli arranged in a trabecular pattern, separated by thin fibrovascular septa, and micro- and macrovesicular steatosis, which indicated the successful induction of HCC in rats.
Treatment of HCC often leads to poor results [46].Therefore, it is necessary to pursue better therapy modalities to offer hope for patients with HCC. In the current study, [131I]atorvastatin was used as a relatively novel radioformula to evaluate its impact as a treatment for HCC. In this investigation, the β-emitter131I isotope was chosen to radiolabel ATV.
The tissue uptake pattern of[131I]atorvastatin in animals is illustrated in Table 3. The analysis suggests that the rescue of the radiotracer from circulation was slightly low as the proportion decreased from 10.1 ± 2.5%at 1 h p.i.to 3.99 ± 0.9% at 8 h p.i. This may be due to the ability of ATV to bind plasma protein. The liver-targeting ability of[131I]atorvastatin was also observed as there was a high uptake in the liver, which reached its maximum value of20.3 ± 3.9%, at 2 h p.i. Because the elimination of ATV happens through the liver, the gut content of the radio compound elevated over time from 13.2 ± 2.9% at 1 h p.i to 20.45 ± 3.4% at 8 h p.i. Although [131I]atorvastatin is metabolized by the liver,part of it is eliminated through the kidneys. Radioactivity was found in the kidneys, confirming that hypothesis,and the radioactivity in urine increased with time. The other organs (bone, lung, heart, muscles,and spleen) showed a minimal uptake. The thyroid glands showed normal uptake over time, which indicated the in vivo stability of [131I]atorvastatin.

Table 2 Serum levels of biomarkers of liver function
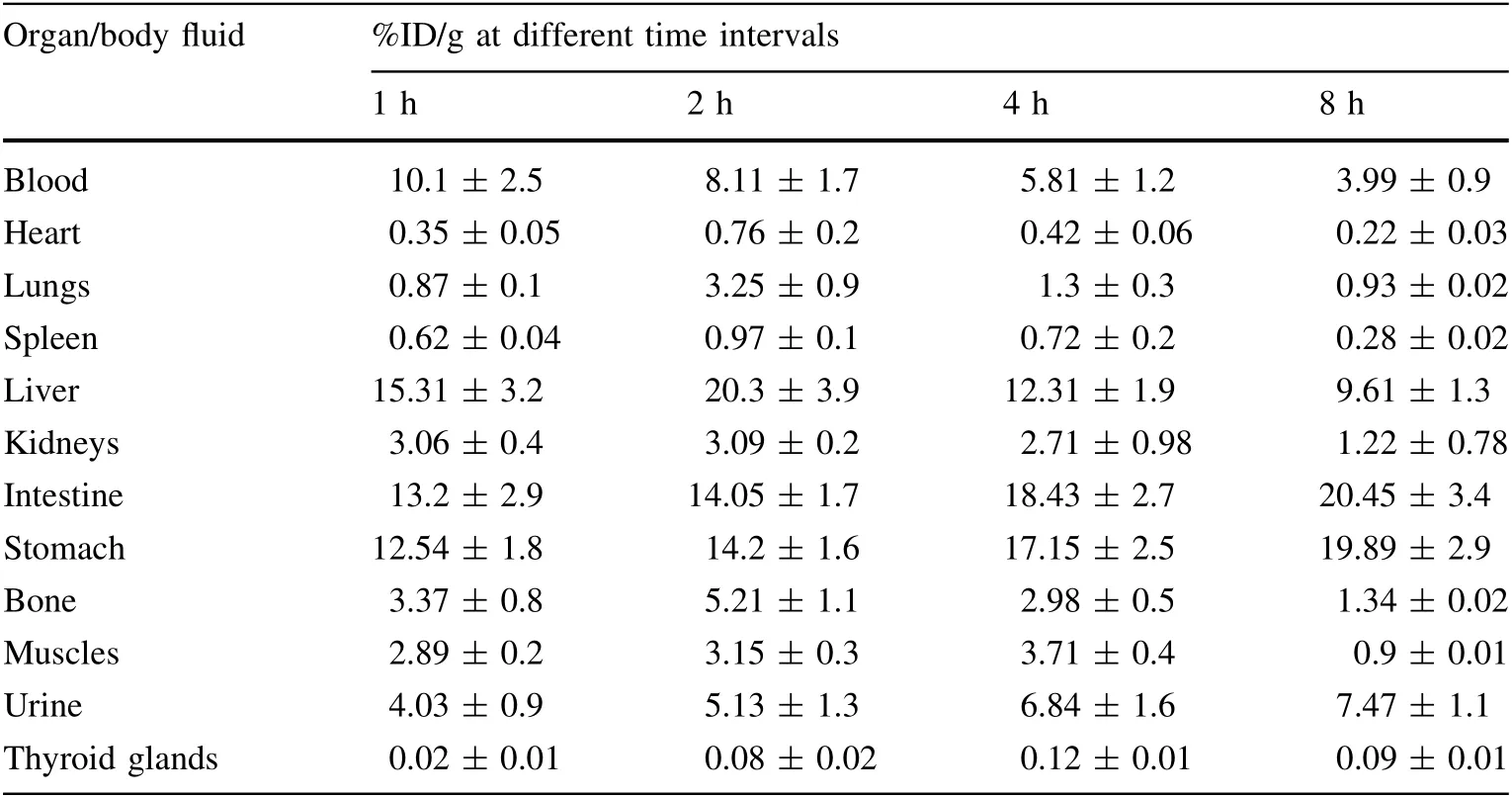
Table 3 Biodistribution profile of [131I]atorvastatin in normal rats
The tissue distribution profile of [131I]atorvastatin in HCC-induced rat models upon intravenous administration is demonstrated in Table 4. The analysis shows that [131-I]atorvastatin uptake was focused in the liver, with a percentage equal to 30.01 ± 4.3% at 2 h p.i. The results revealed the ability of [131I]atorvastatin to target the radionuclide,131I, in the HCC area, which indicated the potential use of ATV as a vehicle to deliver131I isotopes to liver tissues for radiotherapy in HCC.
Figure 9 illustrates the difference of liver uptakes of[131I]atorvastatin at different time points in normal and HCC-bearing rats. The p values were calculated for each time point and found to be less than 0.01 at 1 and 4 h p.i.Meanwhile,the p values were found to be less than 0.05 at 2 h p.i. and less than 0.001 at 8 h p.i. These findingsconfirmed the significant difference between the uptake of[131I]atorvastatin in the normal rat liver and HCC liver at different time intervals.

Table 4 Biodistribution profile of [131I]atorvastatin in HCCinduced rat model
The effects of[131I]atorvastatin on selected biochemical parameters(AST,ALT,and AFP)are presented in Table 5.It was found that [131I]atorvastatin administration resulted in a significant decrease in all tested enzyme activities,including AFP, in blood plasma compared to the control group: by 60.6% for AST, 77.9% for ALT, and 51% for AFP (p <0.05).
Figure 10 shows a liver containing portal tracts with dilated, congested, and thrombosed portal veins, fibrous bands extending from one portal tract to another (P–P),dilated central veins with a detached lining, scattered apoptosis in peri-portal and peri-venular areas, macro- and micro-vesicular steatosis more marked in peri-venular area,and no viable tumor cells.In contrast,no histopathological changes were observed in the control group (data not shown). After [131I]atorvastatin radiotherapy, all the data yielded results confirming the positive impact of [131-I]atorvastatin on HCC.
4 Conclusion
Our hypothesis regarding the potential use of [131-I]atorvastatin as a radiopharmaceutical agent for HCC radiotherapy was successfully confirmed in this study.ATV was radioiodinated using the beta emitter131I isotope,generating 86.7% of stable [131I]atorvastatin for 12 h in vitro. The biodistribution profile of [131I]atorvastatin in both normal and HCC-induced rat models showed a good localization in liver tissues even at 2 h p.i. Interestingly,biochemical parameter analysis(AST,ALT,and AFP)and histopathological studies provided evidence that [131-I]atorvastatin has a positive impact against DENA/CCl4-induced HCC in rats.

Table 5 Serum levels of biomarkers of liver function.Results are given as mean ± SD from 5 rats in each group
AcknowledgementsThe authors would like to acknowledge Dr.Hossam El-Deen A. Awad, Department of Clinical Pathology, New Egypt Hospital for Armed Forces, Cairo, Egypt, for his contribution in the part of biochemical parameters and histopathological analyses.
Author’s contributionsNourihan S. Farrag carried out the practical work and analyzed the data.Abeer M.Amin supervised the design of the experimental plan. All the authors wrote and revised the manuscript.
 Nuclear Science and Techniques2020年11期
Nuclear Science and Techniques2020年11期
- Nuclear Science and Techniques的其它文章
- Analytic RF design of a linear accelerator with a SLED-I type RF pulse compressor
- Preliminary analysis of fuel cycle performance for a small modular heavy water-moderated thorium molten salt reactor
- Effective (kinetic freeze-out) temperature, transverse flow velocity, and kinetic freeze-out volume in high energy collisions
- Design, assembly, and pre-commissioning of cryostat for 3W1 superconducting wiggler magnet
- Simulation-based correction of dose enhancement factor values in photon brachytherapy with metal nanoparticle targeting
- Design of a 162.5 MHz continuous-wave normal-conducting radiofrequency electron gun
