The risk factors of postpartum urinary retention after vaginal delivery:A systematic review
Qiomeng Li ,Shening Zhu ,Xio Xio
a Obstetric Department,Affiliated Shenzhen Maternity & Child Healthcare Hospital,Southern Medical University,Shenzhen,Guangdong,China
b Nursing Department,Affiliated Shenzhen Maternity & Child Healthcare Hospital,Southern Medical University,Shenzhen,Guangdong,China
c Affiliated Shenzhen Maternity & Child Healthcare Hospital,Southern Medical University,Outpatient Department Shenzhen,Guandong,China
Keywords:Natural childbirth Postpartum period Risk factors Urinary retention
ABSTRACT Objectives:This review aimed to explore the independent risk factors of postpartum urinary retention(PUR) after a vaginal delivery.Methods:The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was followed and relevant studies were retrieved from eleven databases.The quality of the included articles was assessed using Critical Appraisal Skills Programme tools or the Appraisal tool for Cross-Sectional Studies.The data analysis was performed using Review Manager version 5.3.Results:A total of nine articles were included and five risk factors were identified,namely,episiotomy(OR=2.99,95%CI=1.31-6.79,P=0.009),epidural analgesia (OR=2.48,95%CI=1.09-5.68,P=0.03),primiparity (OR=2.17,95%CI=1.06-4.46,P=0.03),instrumental delivery (OR=4.01,95%CI=1.97-8.18,P < 0.001),and the duration of the second stage of labor (MD=15.24,95%CI=11.20-19.28,P<0.001).However,fetal birth weights of more than 3800 g were not identified as an independent risk factor (MD=64.41,95%CI=-12.59 to 141.41,P=0.10).Conclusion:This systematic review indicated that the independent risk factors for PUR were found to include episiotomy,epidural analgesia,instrumental delivery,primiparity,and a longer second stage of labor.In clinical practice,healthcare providers could pay more attention to women with these factors and prevent postpartum urinary retention.
What is known?
· The risk factors for postpartum urinary retention(PUR),such as epidural analgesia,instrumental delivery,fetal macrosomia,and longer labor time,have been explored in many articles.However,because of the unclear diagnosis of covert PUR,and the low quality of some studies on the subject,the relationship between these risk factors and the development of PUR is still a matter of debate.
What is new?
· The results of this review will help health professionals to identify the risk factors of PUR,provide interventions for the early prevention of PUR,and optimize postpartum care to women.
1.Introduction
Postpartum urinary retention(PUR) is common among women who have undergone vaginal delivery[1].According to Yip et al.[2],PUR can be classified into two kinds:overt PUR and covert PUR.The definition of overt PUR is clear and widely agreed upon.Women cannot urinate spontaneously within 6 h after natural childbirth or 6 h after the removal of an indwelling catheter in the case of a cesarean section.Covert PUR is defined as a post-void residual volume (PVRV) of more than 150 mL after the first spontaneous urination,as measured by an ultra-sound or catheter,which indicates incomplete urination [2].
The normal mechanism of urination is the initial relaxation of the pelvic floor musculature and the urethral sphincter,in synchrony with increasing contractions of the detrusor muscle and intrabdominal pressure.Urination would be constrained by the weakness of the detrusor muscle with or without relaxation of the urethra[3].Although the pathophysiology of PUR remains unclear,multiple factors related to the physiological,neurological,and mechanical processes that take place during pregnancy and vaginal delivery have been reported [4].For example,in the period of gestation,physiological adaptations occur.These include increases in bladder capacity,urethral length,urethral closure pressure,and urethral pressure,which are precautions against urinary incontinence in pregnancy.These changes will increase the incidence of PUR [5].Also,the obstruction caused by peri-urethral and vulvar edema after childbirth would cause a physical obstruction leading to obstruction of the bladder outlet,resulting from over-distention of the bladder and permanent damage to the detrusor [6].Therefore,the physiological adaptations after pregnancy and the trauma owing to vaginal delivery may lead to PUR.
However,there are no clinical guidelines on the management of postpartum bladder and the treatment of PUR,leading to undertreatment or over-treatment of patients in clinical practice [7].The routine treatment is to initially use non-pharmaceutical methods to induce urination,such as playing the sound of running water,providing a warm compress massage over the bladder region,warm baths,perineal rinsing,acupuncture treatments,and providing privacy and a comfortable place to rest [8].However,these methods were not effective for some postpartum women,which could lead to suboptimal postpartum care and a lower level of treatment satisfaction [9].
If such non-drug conservative treatments are ineffective,pharmacological methods (acupoint or intramuscular injection neostigmine) and/or catheterization may be used.Intramuscular neostigmine is only effective in 70%of patients,and it is associated with some side effects such as bradycardia,bronchoconstriction,increased secretions,nausea,and vomiting [10].Regarding overt PUR,catheterization,including indwelling catheterization and intermittent catheterization,is the standard treatment but may increase the risk of urinary tract infection[6,11].The latest research conducted by Mulder et al.[7]compared clean intermittent catheterization (CIC) to transurethral indwelling catheterization (TIC)for the treatment of overt urinary retention after a vaginal delivery,using a multicenter randomized controlled clinical trial.The result shows that in longer-term bothersome micturition,there were no significant differences between the CIC group and the TIC group.The CIC group took less time than the TIC group to recover the ability to urinate spontaneously.Also,no correlation was found between the duration of catheterization and the initial residual volume of urine that was retained.However,that study lacked sufficient data on urination culture to compare the rate of bacteriuria between the two groups and the cost-effectiveness of the treatments.An additional aim of that study was to evaluate longterm micturition symptoms at 3 months after delivery; however,only 85 women were recruited,68 of whom completed the questionnaire.Thus,the small sample size and the cross-sectional design may have limited the generalizability of the results [12].Therefore,the authors suggested that further primary research (a randomized clinical trial)involving a larger number of participants be conducted on bladder care after delivery,focusing on the issues of cost-effectiveness and bacteriuria.The study did increase awareness of the need to create guidelines on the treatment of PUR and the management of bladder after delivery [13].Further evidence on bladder care in the postpartum period is needed.
Furthermore,although PUR is considered to be transient and not life-threatening[14],there is insufficient evidence to state that PUR has no long-term adverse effects.Also,PUR may be detrimental because of spontaneous bladder ruptures after natural childbirth,which have been reported in many studies [15,16].However,according to Zussman et al.[17],the clinical impact of PUR on longterm urological gynecological diseases is negligible,which is reassuring information to patients and healthcare providers.Simultaneously,Zussman et al.[17]also emphasized the importance of identifying the risk factors of PUR promptly and diagnosing the condition.It was found that unidentified PUR may cause recurrent urinary tract infections,upper urinary tract injuries,permanent dysfunction of the bladder,and urinary retention [18].Mehta and Anger [13]also emphasized the need to continue to explore the relationship between various obstetric parameters and PUR.Therefore,the present review aimed to recognize and quantify high-risk factors in the development of both overt PUR and covert PUR and the influence of these factors.This may help in the early detection and diagnosis of PUR,and in the implementation of timely interventions,leading to the effective management PUR and the prevention of adverse urinary tract complications in clinical practice [4].
2.Methods
The primary aim of this systematic review was as follows:
Objective:to undertake a comprehensive systematic review to explore and quantify the risk factors in postpartum urinary retention.
The review question can be structured using a PEO(population,exposure,and outcome)framework,which is outlined in Appendix A.
2.1.Search strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [19]was followed to identify related English articles published from 01/01/2009-31/12/2019.Some electronic databases were searched for relevant literature,including CINAHL Complete,MEDLINE,PsycINFO,PubMed,NHS Evidence,Cochrane Library,Maternity,and Infant Care,Trip,ScienceDirect,AMED -The Allied and Complementary Medicine Database,and Web of Science.A search was also made for grey literature,such as policy documents,position papers,and research reports,through OpenSIGLE(http://www.opengrey.eu/)and Clinical Trials.Although grey literature is published in a context in which the primary task is not published and is usually not peer-reviewed,relevant information can sometimes be found in grey literature.Therefore,it was necessary to search through the grey literature to obtain comprehensive search results[20].Google Scholar and reference lists were also searched for related literature to ensure that the search was as comprehensive as possible.Keywords were used to cover synonyms,transatlantic terms,medical subject headings (MeSH),wildcards,and acronyms.These keywords also were linked with appropriate Boolean operators,such as and,or,and not [21].The first keyword used for identifying “urinary retention” included“urinary complaints” “urination dysfunction” “voiding dysfunction” “voiding difficulties” “bladder retention” “bladder dysfunctions” “bladder disorder” “failing of bladder emptying” “urinary bladder”.The second keyword used for identifying “vaginal”included “natural childbirth” “normal childbirth” “natural labor”“eutocia”.The third keyword used for identifying “postpartum”included “post-partum” “postnatal” “post-natal” “peripartum”“postpartum period” “postnatal period” “puerperium” “puerperal”“newly birthed”.
2.2.Eligibility criteria
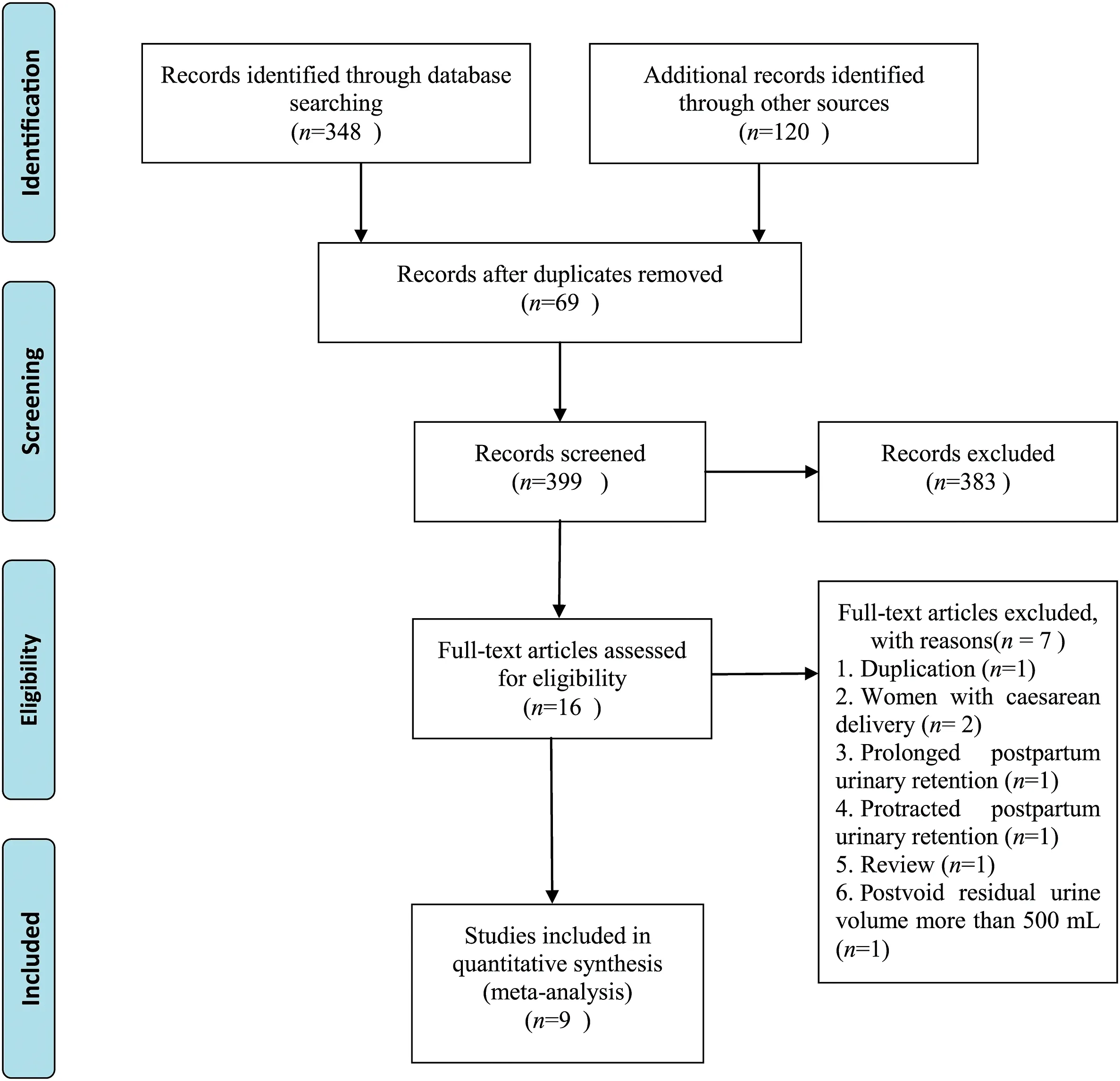
Fig.1.Flow chart of the studies selected for this systematic review.
Primary studies exploring the risk factors for PUR,including overt and covert PUR,were included in the current review.According to Omair [22],compared to randomized control trials(RCT),observational studies,such as case-control studies or cohort studies,would be more suitable for exploring the association between diseases and risk factors.Therefore,instead of including RCTs,quasi-experimental research designs and survey research designs were included in this systematic review,such as casecontrol studies,cohort studies,cross-sectional studies,or studies with longitudinal research designs [23].
Patients who had a normal or instrumental vaginal delivery with uncomplicated pregnancies,regardless of whether they had undergone epidural anesthesia,were included in the present review.Patients who had pre-existing kidney disease,urinary tract disease,overactive bladder,pelvic organ prolapses,previous bladder surgery,or any pre-existing condition that could result in urinary retention were excluded.Patients also were excluded if their infant had required neonatal intensive care or if they had experienced postpartum hemorrhaging,infections,unstable vital signs,or other postnatal complications.Women who delivered via cesarean section and those who required catheterization after labor for any reason other than acute urinary retention were excluded.
2.3.Study selection
The process of selecting studies for inclusion followed the structure recommended by Higgins and Green[24]in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0.Two reviewers selected the studies independently by screening the title,abstract,and full text of the studies after duplicates were removed using Endnote X7.2.
2.4.Quality appraisal
Critical Appraisal Skills Programme (CASP) case-control study checklists were used to assess the quality of case-control studies and cohort studies respectively in this review.Regarding the crosssectional studies,the Appraisal tool for Cross-Sectional Studies(AXIS tool)was used[25].The AXIS tool provides users with greater flexibility than other tools to combine reporting on quality and the risk of biases when making judgments about the quality of crosssectional studies [25].Two reviewers independently assessed the quality of the included articles with selected quality appraisal tools.When the opinions were inconsistent,they would refer to the comments of the corresponding author.The included studies were categorized as high,medium,and low quality according to assessment results and the discussion within the research team.
2.5.Data extraction
During the data extraction process,two reviewers extracted data independently.In the case of a disagreement,the reviewers engaged in discussions to reach a consensus.The characteristics and major findings of each study needed to be extracted using a data extraction form.The characteristics of a study included the title of the article,the authors,the year of publication,the aim or objective of the study,the study design,and the strengths and limitations of the study.The major information on each study included the size of the study population(a total number;overt and covert PUR,respectively),the major risk factors,the risk estimate and the 95% CI,the results of the multivariate logistic regressionanalysis,and the conclusions or some recommendations for further investigation.Dichotomous data and continuous data were extracted using a two-by-two table.If some of the data in a study were unclear or missing,the present author conducted further checks to clarify the data or determine if the missing data could be found.In such cases,the original authors were contacted to obtain some relevant information if necessary.The study was excluded from the current review if complete data could not be obtained.
2.6.Data synthesis
In the present review,a meta-analysis was conducted to summarize the major outcomes of individual articles that had been included.The mean difference and 95% confidence intervals (CI)were calculated for dichotomous data.About continuous data,the odds ratio (OR) and 95% confidence intervals (CI) were used to present the results.Review Manager version 5.3 was used to construct the forest plots.Heterogeneity was used to measure differences in the included articles,and P values were calculated by the I2of the chi-square test.When the I2was greater than 50%,indicating high heterogeneity,a random-effects model was used.When the I2was less than 50%,indicating low heterogeneity,a fixed-effects model was used.
3.Results
A total of 468 potentially eligible articles were identified from this search.Using Endnote software,69 duplicates were removed.Three hundred and ninety-nine articles were screened for eligibility by reading the title and abstracts,and 383 were excluded.The full-text versions of the remaining 16 articles were further checked.In the end,nine articles involving 5,890 participants were included in this review.Details of the PRISMA flow chart are shown in Fig.1.
3.1.Characteristic of the included articles
The nine included studies were published between 2009 and 2019.The included studies were categorized into three types of studies,including case-control [27,29-31,33,34],cohort [28],and cross-sectional studies [26,32].A detailed description of the nine included articles is given in Table 1.The reasons for the exclusion of the other seven articles are presented in Appendix B.
3.2.The results of the quality assessment of the nine included articles
In the nine included articles,three were of high quality[26-28];four were of medium quality[29-32];and two were of low quality[33,34].
3.2.1.The quality assessment of case-control studies
In the six case-control studies [27,29-31,33,34],they all had a focused issue and an appropriate method.All the case and control groups were recruited acceptably except the article by Suzuki et al.[30].All the articles took account of the potential confounding factors in the study design apart from Erlangga et al.[33].A comparison of the demographic characteristics of the case and control groups showed a statistically significant difference in the mean body mass index (BMI) of the two groups (P < 0.05) [33].Overall,one study was appraised as high quality[27],three were of medium quality [29-31]; and two were of low quality [33,34].
3.2.2.The quality assessment of cross-sectional studies
Two cross-sectional studies were included in this review[26,32].One was assessed as high quality [26]and one was of medium quality[32].These two articles had a clear aim and target population.The sample size of the participants and the process of selecting the population were reasonable.One study did not analyze the effect of epidural as a potential confounding factor[32].
3.2.3.The quality assessment of cohort studies
Only one included study was a cohort study [28].The cohort population in this article were recruited acceptably and represented a defined population.One of the limitations of this study was the small size of the sample,which may have influenced the understanding of the associated obstetric parameters(n=155,the number of women with postvoid residual urine volume (PVRV) of more than 150 mL is 12,the number of women with PVRV of less than 150 mL is 143).However,the long-term sequelae of women with high residual urine volumes were not investigated,although this would have been an essential part of a complete study.Nonetheless,the results of this study are believable and generalizable.Therefore,this article is a high-quality study.
3.3.The data synthesis and results
A total of five factors were explored in the nine included articles,namely,epidural analgesia,episiotomy,instrumental delivery,a longer second stage of labor,and primiparity.Episiotomy was reported in six articles [28,30-34],with a pooled OR of 2.99 (95%CI=1.31-6.79,P=0.009) (Fig.2).Instrumental delivery was reported in six articles[28-30,32-34],with a pooled OR of 4.01(95%CI=1.97-8.18,P < 0.001) (Fig.3).Primiparity was reported in six articles [28-30,32-34],with a pooled OR of 2.17 (95%CI=1.06-4.46,P=0.03)(Fig.4).Epidural analgesia was reported in three articles [27,28,31],with a pooled OR of 2.48 (95%CI=1.09-5.68,P=0.03)(Fig.5).A longer second stage of labor was reported in four articles [27,28,31,34],with a pooled MD of 15.24(95%CI=11.20-19.28,P < 0.001) (Fig.6).However,a fetal birth weight of more than 3,800 g was not identified as an independent risk factor(MD=64.41,95%CI=-12.59 to 141.41,P=0.10)(Fig.7).
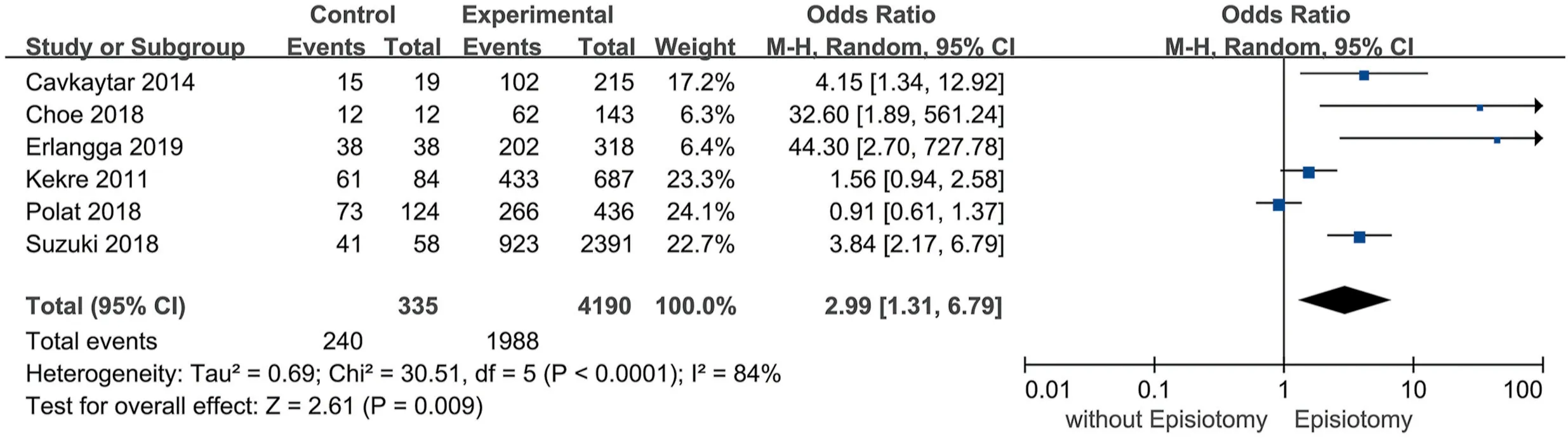
Fig.2.Episiotomy.
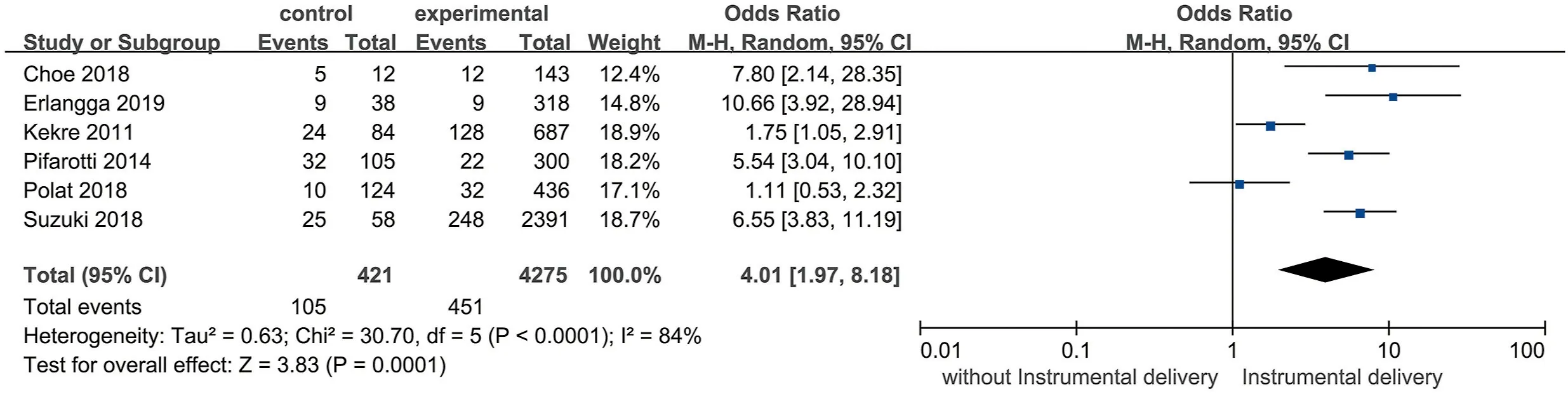
Fig.3.Instrumental delivery.
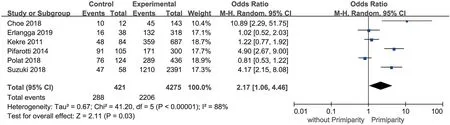
Fig.4.Primiparity.
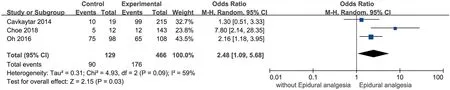
Fig.5.Epidural analgesia.
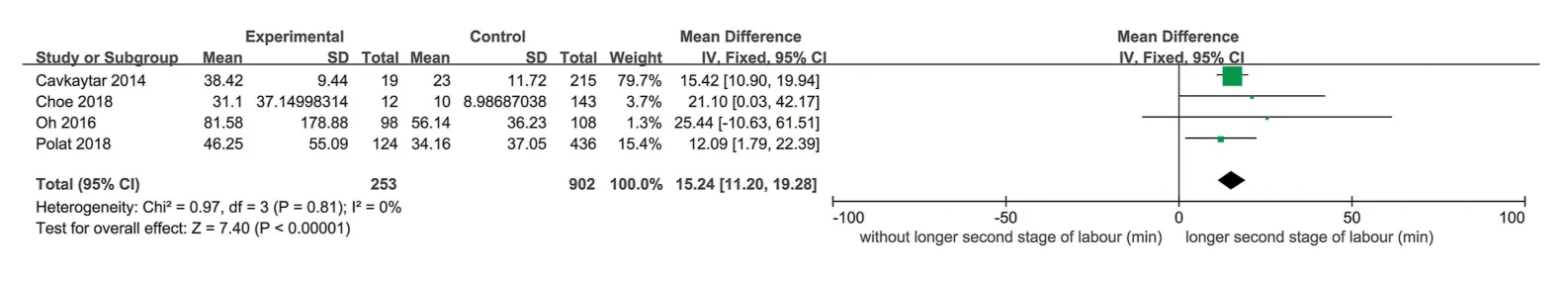
Fig.6.Longer second stage of labor.
4.Discussion
By identifying obstetric risk factors,healthcare professionals can effectively identify women who are more likely to develop PUR and provide timely,appropriate,and effective care measurements for prevention and management [35].A total of nine articles and five factors were found in the current review,including episiotomy,primiparity,a longer second stage of labor,instrumental delivery,and epidural analgesia.
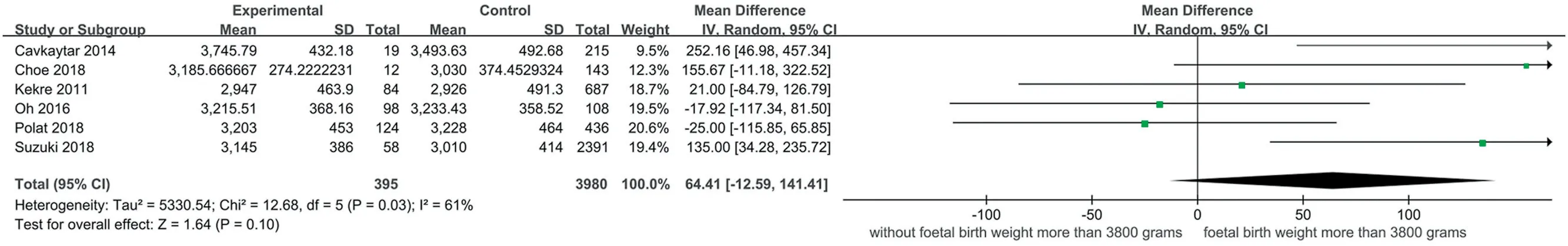
Fig.7.Foetal birth weight more than 3,800 grams.
Here are the reasons why these five risk factors were identified in the current review.Firstly,consistent with previous studies,episiotomy was identified as a risk factor for postpartum urinary retention in this review[5,37,38].The possible reason could be the pain from an episiotomy can lead to reflex urethral spasms,followed by PUR[36].Secondly,the results of this review are similar to the finding of many previous studies that primiparity is an obstetric parameter associated with PUR[9,37,39-41].This may be because,compared to multiparous women,primiparous women may experience more extreme changes and more serious damage to their pelvic floor muscles due to changes in anatomy caused by pregnancy and a vaginal delivery[26].Also,primiparity is thought to be more likely to be associated with tenderness of the pelvic floor and to damage to the pudendal nerve during a vaginal delivery than a cesarean delivery [34].Carley et al.[36]also found that primiparity is also more likely to result in an instrumental delivery(47.1%vs 12.4%;P<0.001),involving the use of regional anesthesia and episiotomy.
Thirdly,a longer second stage of labor was also identified as a risk factor for PUR in this review.The possible reason could be that during a prolonged second stage of labor,mechanical strength exerted on the pelvic floor muscles can lead to pelvic,pudendal,and urinary nerve injuries,as well as to an increase in abdominal pressure with the presence of the baby[31,34].Similar results have also been reported in previous studies [2,42].Fourthly,instrumental delivery was another risk factor for PUR in this review.One possible reason could be that it can lead to urinary neurological disorders,such as impairment of the peripheral nerves,pelvic musculature,and sphincter urethrae; damage to the micturition reflex,and perineal edema;or to bladder trauma as a direct result of mechanical outlet obstruction [32].This finding is similar to that from previous studies [36,43,44].
Fifthly,this review found that epidural analgesia may also increase the possibility of PUR.Epidural analgesia may help to reduce labor pain,while the nerves of the bladder are anesthetized at the same time.This hurts the connection between the pontine micturition center and the bladder,which inhibits the reflex mechanism that usually causes urination.Subsequently,the bladder may become over-distended,which reduces the contractility of the bladder [28].Also,the evidence suggests that an epidural can extend the duration of labor [45]and increase the chances of an instrumental delivery,which could lead to pelvic floor trauma,pudendal nerve damage,and perineal edema,resulting in mechanical obstruction and bladder motility problems after childbirth[46].Furthermore,variations in how patients respond to regional analgesia might influence the result of studies on the use of epidural analgesia [47].
The results of the meta-analysis indicate a low level of heterogeneity between the included articles(I2=0%)in connection with only one of the above five factors,a longer second stage of labor.A high level of heterogeneity(I2=59%-88%)was observed with the other factors,namely,episiotomy,epidural analgesia,instrumental delivery,and primiparity.Therefore,heterogeneity existed in these included articles.This may be because of the following reasons.First,there were three types of studies in the nine included articles,namely case-control,cohort,and cross-sectional studies.Different study designs may lead to a high level of heterogeneity.Also,these three study designs have some potential limitations.For example,while a properly designed case-control study could provide reliable results,case-control and cohort studies are observational studies that lie near the middle of the hierarchy of evidence,which is a potential and natural limitation of these types of studies [39].Second,the five risk factors could affect and interact with each other rather than act independently.When testing is strictly controlled,some risk factors are more important than others [44].In studies where the methods of data analysis are not strictly controlled,the risk factors would be different from that of other studies.Therefore,there could be many confounding factors in those studies when exploring the risk factors for PUR.Third,some articles have a special targeted population or a specific research direction.For example,the article conducted by Oh et al.(2016)[27]explored the risk factors for PUR and focused on the direction of an episiotomy.Also,in the nine included studies,two involved the recruitment of women who did not undergo epidural analgesia[30,32]; therefore,in these two studies,it was not possible to include epidural analgesia as a risk factor for PUR.Although the results of these two articles would differ from those of the others,this does not mean that epidural analgesia is not a risk factor for PUR.
Five independent risk factors for PUR were identified in this review.Compared to the systematic review conducted by Mulder et al.[39],there were some differences in the findings.First,Mulder et al.found four independent risk factors for overt PUR [39],namely,episiotomy,instrumental delivery,epidural analgesia,and primiparity.Therefore,the present review identified a longer second stage of labor as an independent risk factor for PUR,a factor not documented in the article by Mulder et al.[39].Second,the author of the current review discussed risk factors for PUR without separating the discussion into covert PUR and overt PUR.In the study by Mulder et al.[39],four independent risk factors for overt PUR and no significant ones for covert PUR were found because of high heterogeneity due to the differences in the definition of covert PUR.
5.Strengths and limitations
The current review was in strict accordance with the requirements laid out in the Cochrane Handbook for Systematic Reviews.Also,two reviewers independently conducted the process of selecting the articles,assessing their quality,and extracting data.However,there are some limitations to this review.First,although high heterogeneity existed in the included articles about some risk factors,the authors failed to find the source of heterogeneity with a subgroup analysis or a sensitivity analysis.Second,to guarantee the latest research results,only studies published in the past 10 years have been included in this review.Moreover,only those published in English were included; thus,some relevant articles might have been excluded because they appeared in other languages.Furthermore,some of the included articles were of low quality,which might have influenced the results of the current review.
6.Conclusion
After a discussion of points under debate,the independent risk factors for PUR were found to include episiotomy,epidural analgesia,instrumental delivery,primiparity,and a longer second stage of labor.The results of this review will help health professionals to identify the risk factors of PUR,provide interventions to prevent PUR in a more timely manner,and optimize postpartum care to women.
Funding
This study was funded by the Affiliated Shenzhen Maternity&-Child Healthcare Hospital,Southern Medical University(FYB2018008).
CRediT authorship contribution statement
Qiaomeng Li:Conceptualization,Methodology,Software,Data acquisition and analysis,Data curation,Formal analysis,Writing -original draft.Shening Zhu:Supervision,Writing -original draft.-Xiao Xiao:Conceptualization,Validation,Writing-Reviewing and Editing,Writing -review &editing
Declaration of competing interest
The review authors had no conflicts of interest.
Acknowledgement
We would like to appreciate Alice May and tutors in the personal development department and library from Birmingham City University for their guidance and assistance.We are grateful to Affiliated Shenzhen Maternity&Child Healthcare Hospital,Southern Medical University.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.09.002.
 International Journal of Nursing Sciences2020年4期
International Journal of Nursing Sciences2020年4期
- International Journal of Nursing Sciences的其它文章
- An exploration of the breastfeeding behaviors of women after cesarean section:A qualitative study
- Health personnel-targeted education interventions on inpatient suicide prevention in general hospitals:A scoping review
- Demands of experiential training for ICU nurses in Hunan of China
- Understanding autism spectrum disorder and coping mechanism by parents:An explorative study
- Association of swallowing problems with frailty in Chinese hospitalized older patients
- Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study
