Open reduction and internal fixation for radial head fractures: A prospective observational study
Imran Khan Mangi, Arslan Ahmed Abro, Muhammad Naveed Memon, Shahjahan Siyal, Naveed Khan, Nouman Memon, Muhammad Kazim Rahim Najjad
Orthopaedic Surgery, Liaquat National Hospital and Medical College, Karachi, Pakistan
ABSTRACT Objective: To evaluate the effect of open reduction and internal fixation on radial head fracture and assess the post-operative function.Methods: This prospective observational study was conducted from June 2016 to July 2017 at Liaquat National Hospital and Medical College, Karachi. Altogether, 28 patients with radial head and neck fractures were enrolled in our study. These patients were admitted to the hospital and their fractures were fixed with open reduction and internal fixation. Baseline information of the patients was collected, and patient-rated elbow evaluation scores were calculated.Results: Out of the 28 patients, 21 were male and 7 were female.Besides, 16 fractures were on the right side and 12 were on the left side and 17 involving the dominant hands. In addition, 8 patients had Mason type II fracture and 20 had Mason type III fracture.The mean age of patients was (31.0 ± 8.0) years, and the mean follow-up is (1.2 ± 0.5) years. The mean average patient-rated elbow evaluation scores were (27.64 ± 1.60) at 1-year follow-up.Conclusions: The majority of the patients who had radial head fractures and treated by open reduction and internal fixation have attained an excellent range of motion postoperatively.
KEYWORDS: Radial head fractures; Open reduction and internal fixation; Functional outcome
1. Introduction
Among elbow fractures, radial head fractures have the highest prevalence, but the treatment is still controversial. Radial head fractures that are not displaced and minimally displaced can be managed non-operatively with good results[1]. It is also known that there are more favorable outcomes with early radial head replacement than that with open reduction and internal fixation(ORIF) for patients who suffered complete articular radial head fractures with more than three displaced fragments[2,3].
Radial head and neck fractures are described by Mason’s classification. The classification has been modified several times and is commonly divided into four groups. According to Broberg and Morrey classification, Mason I is undisplaced fractures; Mason II is fractures with more than 2 mm displacement, involving at least 30% of the radial head; Significantly comminuted fractures are Mason III; Mason IV is fractures of the radial head or neck with associated elbow dislocation. Treatment of Mason I fractures is conservative with a pressure bandage and sling for support, and active mobilization as early as possible. Referring to treatment of Mason type II fractures, there is still a controversy. Both conservative and surgical treatment is described with a favorable outcome in literature. Various options of treatment are available for Mason III and IV fractures, such as ORIF, arthroplasty, and resection of the radial head[4-12].
The goal of this study is to summarize functional outcomes of the radial head and neck fractures treated by ORIF.
2. Materials and methods
2.1. Ethical approval
The study was approved by the Ethics Review Committee of Liaquat National Hospital and Medical College, Karachi (0229-2016). And the informed consent has been obtained from each patient.
2.2. Study design
This prospective observational study was conducted from June 2016 to July 2017 at Liaquat National Hospital and Medical College,Karachi.
2.3. Inclusion and exclusion criteria
Patients with artial articular radial head fractures displaced greater than 2 mm but less than 5 mm were included in the study.Displacement was defined as the greatest distance of separation of fracture fragments as seen radiographically on CT scan. Patients with traumatic Broberg-Morrey Mason II-III radial head or neck fractures are eligible for inclusion. Patients between the ages of 25 to 55 years were included.
Exclusion criteria included skeletal immaturity, age >55 years,documented isolated elbow dislocation, any other fracture around the elbow, or clinically evident ligament injury elsewhere in the ipsilateral upper limb.
2.4. Data collection and analysis
In 12th months, a detailed review of the patients was done, which included the range of motion and patient-rated elbow evaluation(PREE) scores. Descriptive statistics were calculated using SPSS version 21. The outcome was divided into four categories as excellent (scores: 0-20), good (scores: 21-40), fair (scores: 41-60),and poor (scores: >60), as per scoring system, the patients were divided into four groups on the basis of functional outcome.
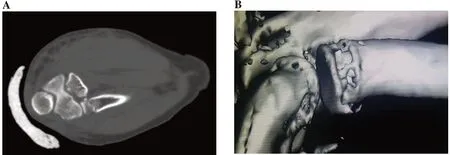
Figure 1. Radial head fracture. A: Axial view of elbow CT scan showing radial head fracture with partial displacement; B: 3D reconstruction image showing partial radial head fracture.
3. Results
In total, 28 patients with radial head and neck fractures were enrolled in our study (Figure 1A and Figure 1B). Out of the 28 patients, 21 were male and 7 were female. Among the patients, 16 fractures were on the right side and 12 were on the left side and 17 involving dominant hands. Besides, 8 patients had Mason type II fracture and 20 had Mason type III fracture. The mean age of patients was (31.0 ± 8.0) years.
All patients were operated under general anesthesia in the supine position with injured arm on radiolucent arm table. Image intensifier positioned perpendicular to the injured arm coming from foot side. Kocher approach was used in all patients, and incision started from 2 cm proximal to lateral humeral epicondyle across elbow joint, over the radial head, and approximately 5 cm distal to the joint. The identification of interval between extensor carpi ulnaris and anconeus muscle was done. Then, supinator proximal fibers split in deep dissection, staying on posterior cortex of the radius away from posterior interosseous nerve, incised joint capsule longitudinally, and exposed the radial head and annular ligament. The fracture was identified, hematoma was evacuated,and articular surface was restored anatomically and held in position with 1.4 mm k wires, and 2 mm Herbert screws were passed, and 4 or 5 holes radial head reconstruction plate was applied (Figure 2A and Figure 2B). Postoperatively all the patients were given 2 doses of cefuroxime and analgesia as needed for pain. Above elbow, back slab was given to all patients for soft tissue injury and for pain reduction. On the second day of operation, the dressing was changed and patient discharged. The backslab was removed after four weeks, and range of motion was started in all patients.Patients were followed in Out-Patient Department at 2 weeks’ time for removal of skin staples, and follow-up was done at 6 weeks,3 months, 6 months, and 12 months, and the mean follow-up is of (1.2 ± 0.5) years. In each visit, the same surgeon examined the patient for any sign of wound infection.
At the 1-year follow-up by using PREE scores, 11 patients(39.2%) had the scores of 0-20 (excellent result), 13 patients(46.4%) of 21-40 (good result), 4 patients of 41-60 (fair result)and 0 patient of above 60 (poor result). Besides, the mean average PREE scores were 27.64 ± 1.60. In addition, no significant complications like deep infection, malunion, non-union, nerve palsy, re-fracture were observed.
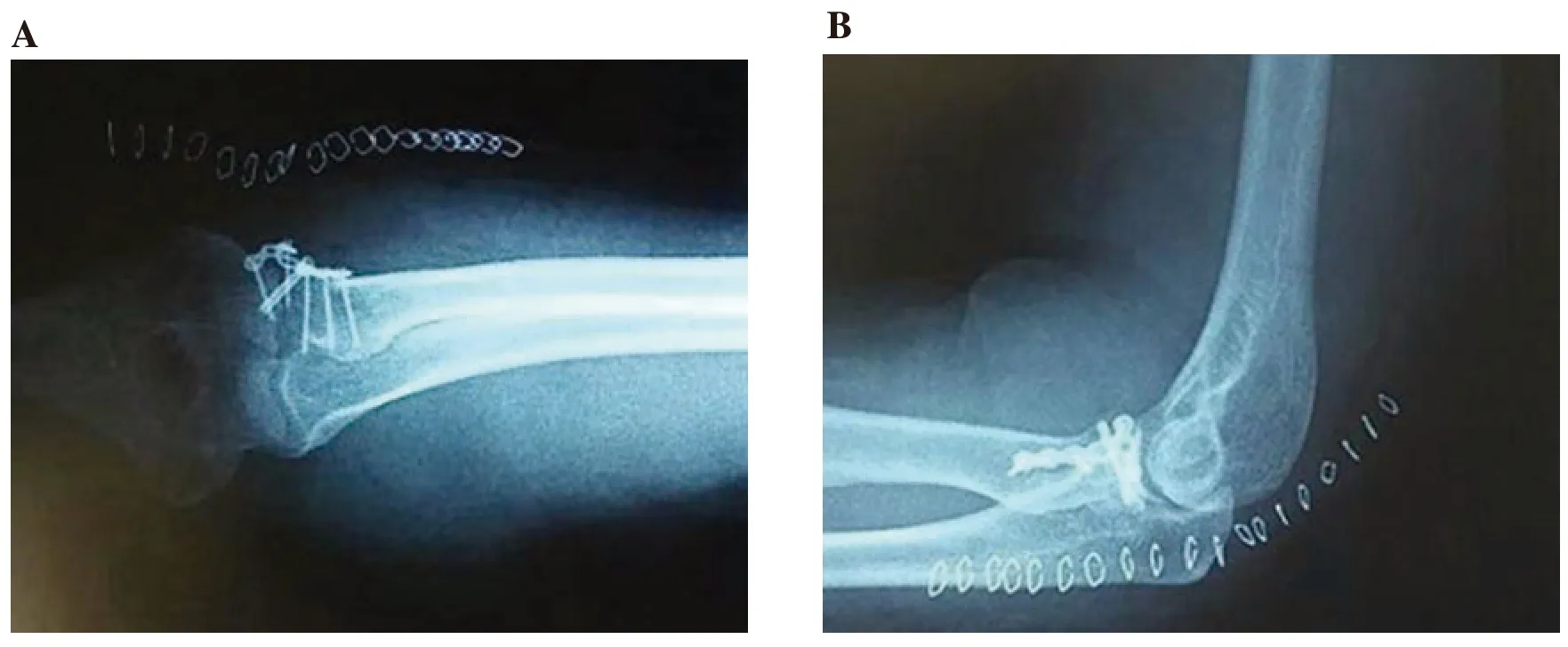
Figure 2. Post-operation X-ray showing right elbow. A: Anterior-posterior view; B: Lateral view.
4. Discussion
Good-to-excellent results have been confirmed in incomplete radial head partial articular fractures managed by means of ORIF,as shown in several retrospective studies[13-16].
Khalfayanet al.[17] studied different outcomes in radial head incomplete articular fractures with displacement or angulation of >2 mm in which 16 patients were managed by conservative treatment while 10 patients by operative means. He retrospectively studied the outcomes with a mean follow-up of 1.5 years. He found 90% of good-to-excellent results in the studied patients were managed with operative intervention versus the 44% of good-toexcellent results in the non-operative treatment group (P<0.01).After the follow-up, X-rays of the patients treated non-operatively showed a greater degree of displacement, malalignment of the joint surface, and arthritic changes around joint.
Pearceet al.[18] studied 19 patients having isolated, displaced partial articular fractures that were managed by operative means(ORIF), which demonstrated comparable functional outcome in all enrolled participants.
Ringet al.[19] has mentioned in their retrospective study which included 30 patient’s in two groups with 15 patients in each group.One of the groups included patients with comminuted fractures while other groups contain patients with a single fragment. Both group’s managed with ORIF. However, satisfactory results were noticed in patients with single fragments while unsatisfactory results were noticed in another group of patients (approximately 27%).
For articular radial head fracture, when an incomplete fragment obscure and obstruct elbow joint range of motion, and the fragment can not be managed with ORIF, then the fragment should be excised. Before the excision of the fragment, it must be confirmed that the stability of elbow or upper forearm must not be compromised. If stability is doubtful, radial head replacement should be performed. Besides, the consequences of radial head fracture on biomechanics and stability of elbow depends on the size of fracture. If fracture size is >25% of total intraarticular disc,radial head should not be removed or excise. Patients must be informed and should be explained in detail regarding the possibility of removal of radial head, it’s replacement with radial head prosthesis, and para articular osteotomy if needed for symptomatic malunion or nonunion.
ORIF is a valuable option for treating radial head fractures in young, athletic population. We found that 85% of the patients were able to return to full activity following surgery. ORIF should be performed when a stable fixation is needed in order to attain maximum radio-capitellar contiguity, and a preliminary elbow range of motion is advisable/advantageous. Fracture with minimum metaphyseal bone loss, articular fragment with no joint impingement or distortion, the fragment of adequate size, and standard bone condition to have maximum screw purchase are the favorable factors for ORIF.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
I.K.M. and M.N.M. conceived of the presented idea. A.A.A.developed the theory and performed the computations. S.S. and N.K.verified the results. M.K.R.N. encouraged. and N.M. supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
 Journal of Acute Disease2020年4期
Journal of Acute Disease2020年4期
- Journal of Acute Disease的其它文章
- "Resuscitator": Golden medtech proposal introducing a new era for CPR
- Incidence of Enterobius vermicularis in acute appendicitis: A systematic review and meta-analysis
- Prevalence and antimicrobial susceptibility patterns of bacteria in ICU patients with lower respiratory tract infection: A cross-sectional study
- Effect of 8-week and 12-week triple therapy (doxycycline, rifampicin,and gentamicin) on brucellosis: A comparative study
- Cope’s sign and complete heart block secondary to acute cholecystitis: A case report
- Adult-onset Still's disease: A case report
