Robotic vs laparoscopic right colectomy - the burden of age and comorbidity in perioperative outcomes:An observational study
Fulvio Tagliabue,Morena Burati,Marco Chiarelli,Luca Fumagalli,Elisa Arborio,Department of Robotic and Emergency Surgery,Ospedale A.Manzoni,ASST Lecco,Lecco 23900,Italy
Angelo Guttadauro,Department of Surgery,University of Milan-Bicocca,Istituti Clinici Zucchi,Monza 20900,Italy
Matilde De Simone,Ugo Cioffi,Department of Surgery,University of Milan,Milano 20122,Italy
Abstract
Key words:Right hemicolectomy;Robotic surgery;Laparoscopic surgery;Elderly patients;Comorbidity;Hospital stay
INTRODUCTION
Minimally invasive surgery has gained wide acceptance for colon cancer resection.Several studies have demonstrated that the laparoscopic approach for treatment of right colon cancer is safe and feasible,and its outcomes are equivalent to open surgery[1,2].Moreover,better recovery,consisting of less post-operative pain and shorter hospital stay,after laparoscopic right colon resection has now resulted in this minimally invasive procedure being the gold standard for surgical treatment of ascending colon neoplasms[3-5].Nevertheless,laparoscopic right hemicolectomy (LRH)can be technically challenging,and its learning curve has been demonstrated to be consistently longer than the open approach[6].Since its introduction in the early 2000’s,robotic surgery seems to offer a solution to this issue,overcoming the technical limitations associated with the laparoscopic approach,thanks to the multiple degrees of freedom of instrumentation and 3-dimensional imaging.In addition,international studies have shown the safety,feasibility and oncologic adequacy of robotic right hemicolectomy (RRH)[7,8].In the last decades,life expectancy has constantly improved causing a higher incidence of malignancies.At the same time,elderly patients present with more comorbidities which usually lead to a high risk of post-operative complications.Even if the laparoscopic approach for right colon resection is considered feasible in elderly patients,most of the studies,analyzing minimally invasive surgery,tend to exclude this population,as they are considered to be more prone to post-operative morbidity,especially when it comes to procedures requiring long anesthesia and preternatural operative positions.
Therefore,we conducted this retrospective study to assess the burden of age and comorbidities on laparoscopicvsrobotic surgery for right colon cancer.
MATERIALS AND METHODS
Setting and participants
We retrospectively collected and analyzed data on patients who underwent minimally invasive laparoscopic or RRH at the Robotic and Emergency Surgery Department of the Alessandro Manzoni Hospital,Lecco,from January 2014 until September 2019.Adult (age > 18 years) patients with a diagnosis of adenocarcinoma or endoscopically unresectable adenoma of the right colon (cecum,ascending colon,and hepatic flexure) were included.In all cases,diagnosis was confirmed by definitive histopathologic examination.Patients submitted for multivisceral resection or emergency procedures were excluded[9].The Alessandro Manzoni Hospital is defined as a tertiary-level Hospital.The Division of General Surgery performs approximately 150 colorectal resections per year and robotic colonic surgery was routinely introduced from 2017.Surgical procedures were performed according to standardized techniques[10-12]by two operators with consistent experience in minimally invasive surgery (Tagliabue F and Chiarelli M).A colonoscopy and a chest-abdomen computed tomography scan were performed as pre-operative investigations as well as an anesthesia evaluation and blood tests.No bowel preparation was prescribed,and a short-term prophylactic antibiotic treatment was administered 30 min before surgery.The post-operative period was managed following enhanced recovery after surgery protocols[13].The discharge criteria were:Apyrexia,oral intake of solid diet,and normal bowel and urinary function.The selection bias was minimized by restricting the study to a narrow range of pathologies in a defined population;moreover,the surgical indications (related to tumor stage or patients’ comorbidities) and postoperative management were identical in the two groups.
Data collection
Written informed consent for data collection was obtained from each patient.The local Ethics Committee approved the study (protocol RP02-0008564/17U).Demographic,clinical,pathologic,pre-,and post-operative data were collected from the clinic electronic register of the Division of General Surgery,while the intraoperative data were collected by the surgical electronic register of the Department of Robotic and Emergency Surgery.A 90-d and 180-d follow-up was considered adequate to fully evaluate post-operative complications.To minimize information bias,the investigators (Burati M,Arborio E and Guttadauro A) who gathered data from the clinic register were different to the two operators (Tagliabue F and Chiarelli M) and were masked regarding the surgical technique.The two operators collected the intra-operative data.The final dataset was collated by matching the data of the two registers using a linkage record technique.
Outcomes,exposure and predictors
The primary clinical outcome of the study was the length of hospital stay (LOS)measured in days.The secondary outcomes were time to first flatus (TFF) and time to first stool (TFS) evacuation.The exposure was the robotic technique;the control was the laparoscopic technique,the current standard treatment for carcinoma or endoscopically unresectable adenoma of the right colon[14].Routine demographic variables were obtained,including age at time of surgery and gender.Age was subsequently dichotomized to 75 years,as previously described[15].Body mass index(BMI) and American Society of Anesthesiologists (ASA) physical status were registered.The age-adjusted Charlson Comorbidity Index (ACCI) of each patient was calculated[16]and was subsequently dichotomized to 7.A score equal or higher than 7 is associated with a 0% 10-year survival and,consequently the investigators considered a value equal to 7 indicative of high comorbidity status[16,17].In the case of carcinoma,tumor stage according to the tumor node metastasis (TNM) system was recorded.The following intra-operative variables were determined:Surgical technique,length of surgical procedure,conversion to open technique,and intraoperative complications.
All post-operative complications were registered and classified according to the Clavien-Dindo classification[18,19].All patients with a Clavien-Dindo grade I or higher were considered to have developed a complication.
Study size
The investigators considered a 2-d reduction in LOS following the robotic technique as relevant.From historical data,laparoscopic right colectomy was characterized by a mean LOS of 8 ± 4.5 d.The hypnotized effect size for thet-test for independent means with homogeneous variance was 0.45,corresponding to approximately 60 patients for each group,considering first-type error α = 0.05 and second-type error β = 0.2.
Statistical methods
Continuous variables were expressed as the mean and standard deviation or median and interquartile range (IQR),as appropriate.Categorical variables were presented as frequencies and percentages.For the continuous variables,the normality was valued by the Shapiro-Wilk test and the homogeneity of variances by the Bartlett test.Comparisons between continuous data were assessed by the Student’st-test or Mann-Whitney U test,as appropriate;comparisons between categorical variables were made by Pearson’sχ2test.The significance level of α was set at 0.05.The outcomes of the study were quantitative data and consequently linear regression models were used.Each multivariable regression model was built with a backward sequential method.The predictors of the final model were chosen on the basis of significant β coefficients(P< 0.05 att-test) and relative confidence intervals;theF-test of the analysis of the variance of regression was also considered for the selection of predictors.The coefficient of determinationR2was specified for any regression model.The multicollinearity of variables was measured by variance inflation factors (values > 5 were considered indicative of high collinearity).Normality and homoscedasticity of residuals were tested by the Shapiro-Wilk test and Breusch-Pagan test,respectively.In the case of violation of the linear regression assumptions,a robust regression model was employed.To evaluate the relevance of potential confounders and relevant interactions all final regression models included these confounders and interactions.Statistical analysis was performed using STATA®version 14 (StataCorp LLC,College Station,TX,United States).
Subgroup analysis
All predictors significant in the regression models were independently analyzed in relation to primary and secondary outcomes.Moreover,the associations between the relevant predictors and Clavien-Dindo grading or specific complications were explored.
RESULTS
General population characteristics
Between January 2014 and September 2019,272 patients underwent right colectomy at Alessandro Manzoni Hospital.One hundred forty-nine patients were excluded from the study:86 for urgent colectomy,15 for multivisceral resection,and 48 for benign pathology.Consequently 123 patients were retrospectively analyzed:68 cases underwent laparoscopic right colectomy and 55 robotic procedures.The final data collected included no missing data.Most of continuous data were not normally distributed,therefore they are presented as median and IQR.The median age of the study population was 72 years (IQR 64-79);47 (38.21%) patients were 75 years old or more and 76 (61.79%) were less than 75 years old.In relation to gender,72 (58.54%)patients were males and 51 (41.46%) females.The median body mass index was 24.51(IQR 22.39-27.91).Twenty-five (20.33%) patients were classified as ASA 1,63 (71.54%)patients as ASA 2,34 (27.64%) patients as ASA 3,and 1 (0.81%) as ASA 4.The median ACCI value was 6 (IQR 5-7);36 (29.27%) patients had an ACCI greater than 7 and 87(70.73%) less than 7.In 27 (21.95%) cases the definitive diagnosis was adenoma and in 96 (78.05%) cases the definitive diagnosis was adenocarcinoma.According to the TNM system,27 (28.13%) patients were classified as stage I,35 (36.46%) patients as stage II,32 (33.33%) patients as stage III and 2 (2.08%) as stage IV.Median operation time was 160 min (IQR 135-198) with 8 (6.5%) conversions to open surgery;in one case(0.81%) an intra-operative cardiac complication occurred.The median number of removed lymph nodes was 27 (IQR 21-37).There was no 90-d mortality;180-d outpatient follow-up did not reveal any further post-operative complications,confirming the absence of mortality.
Comparison between groups
Univariate analysis of continuous data was performed with non-parametric tests(Mann-WhitneyUtest),because the assumptions of normality and homoscedasticity of primary and secondary outcomes were not satisfied.The baseline characteristics of the two groups are summarized in Table 1:No significant differences were found in pre-operative epidemiological and clinical variables.The results for intra-operative outcomes are shown in Table 2:Only operative time in the RRH group was significantly longer than that in the LRH group.LOS was shorter in the RRH group(Table 3);also,TFF and TFS were significantly earlier in the RRH group (Table 3).Post-operative complications are summarized in Table 4:No differences between the two techniques were registered,except for wound infection and ileus.Prolonged postoperative ileus was greater in patients who underwent LRH.No differences were found at Clavien-Dindo grading (Table 5).
Multivariable regression models
To create an a priori predictive model,multivariate analysis was exclusively performed with pre- and intra-operative variables.In the multivariable regression model,the robotic technique was confirmed to be significant in the model of primary outcome;in addition the dichotomous variables of age over 75 years (age ≥ 75 years)and ACCI more than 7 (ACCI ≥ 7) were significant predictors of the LOS (Table 6).Similarly,in the multivariable regression models of the secondary outcomes the robotic technique was confirmed to be a relevant predictor in association with age ≥75 years (Tables 7 and 8).Linear robust regression was employed in all three models because the residuals of regression did not respect the assumptions of normality and homoscedasticity.No relevant interactions between predictors were found.
Subgroup analysis
Age ≥ 75 years and ACCI ≥ 7 were independently analyzed in relation to primary and secondary outcomes (Table 9).Patients aged ≥ 75 years had longer LOS and later TFF/TFS,while patients with ACCI ≥ 7 were only associated with a prolonged hospital stay.No predictors were significantly associated with Clavien-Dindo grading.Regarding specific post-operative variables,wound infection,pleural effusion and respiratory complications were more frequent in patients older than 75 years;atrial fibrillation and respiratory complications were more frequent in patients with a high comorbidity index (ACCI ≥ 7).
DISCUSSION
The present study,analyzed 123 minimally invasive (laparoscopicvsrobotic) right colectomies performed in our center,and the results seem to confirm that robotic colonic surgery is associated with better recovery compared to the laparoscopic approach[20].In fact,in our series,LOS,TFF,and TFS were significantly shorter in the robotic group.At the same time,prolonged ileus was significantly more common after LRH.
It is well known that robotic surgery is related to high costs[21].Thus,in common practice,patients tend to be accurately selected to maximize the benefits of this miniinvasive technique.The main goal of this study was to analyze the impact of age and comorbidities on robotic and laparoscopic colectomy for right colon cancer.It is important to highlight the definition of old age and comorbidity.There is no international accepted definition of when a patient can be considered old.Similar to other authors,we consider 75 years as the cutoff for elderly[15,22,23].Nevertheless,others tend to set this limit at older or younger ages (70 years or 80 years)[24,25].The Charlson Comorbidity Index is based on 19 disease conditions,each assigned a weighted score[16].The ACCI is a modification that considers age as an additional comorbidity factor[26].The ACCI has been accepted as an effective predictor of patient outcome in colorectal surgery[27].Also,the ASA score is widely used to describe the comorbidities in surgical patients.Its assessment is highly subjective;therefore,it is much less precise in predicting post-operative outcomes,compared to the ACCI[28].According to some authors who analyzed the impact of comorbidities on post-operative outcomes,an ACCI score of 6 or higher is considered as severe comorbidity[29,30].A score of 7 corresponds to 0% 10-year survival rate;therefore we set an ACCI of 7 as the limit for high comorbidity[16,17].We also considered a large retrospective study which demonstrated that an ACCI higher than 7 was connected to higher 30-d mortality in ICU patients[31].Moreover,in the majority of cases,the baseline ACCI value of our patients was 4 (2 points for solid tumor and 2 points for a patient older than 60 years).In addition,a Charlson Comorbidity Index score of 3 is considered the watershed for high comorbidity in international literature[32].Interestingly,in our study,a score of 7 corresponded to the third interquartile of the variable ACCI.According to our multivariable regression analysis,age and high pre-operative morbidity affected recovery in both the laparoscopic and robotic groups.Also,following multivariable analysis,the robotic technique was still predictive of significantly shorterhospitalization and faster restoration of bowel function,when compared to the laparoscopic technique.Moreover,age ≥ 75 years and an ACCI ≥ 7,were associated with prolonged hospital stay (Table 6),but only age ≥ 75 years was related to longer TFF and TFS (Tables 7 and 8).With regard to post-operative complications,as shown by the subgroup analysis,wound infection and pleural effusion were more frequent in elderly patients,while atrial fibrillation was more frequent in patients with severe comorbidities.Post-operative respiratory complications were more common in patients with both predictors of age ≥ 75 years and ACCI ≥ 7.
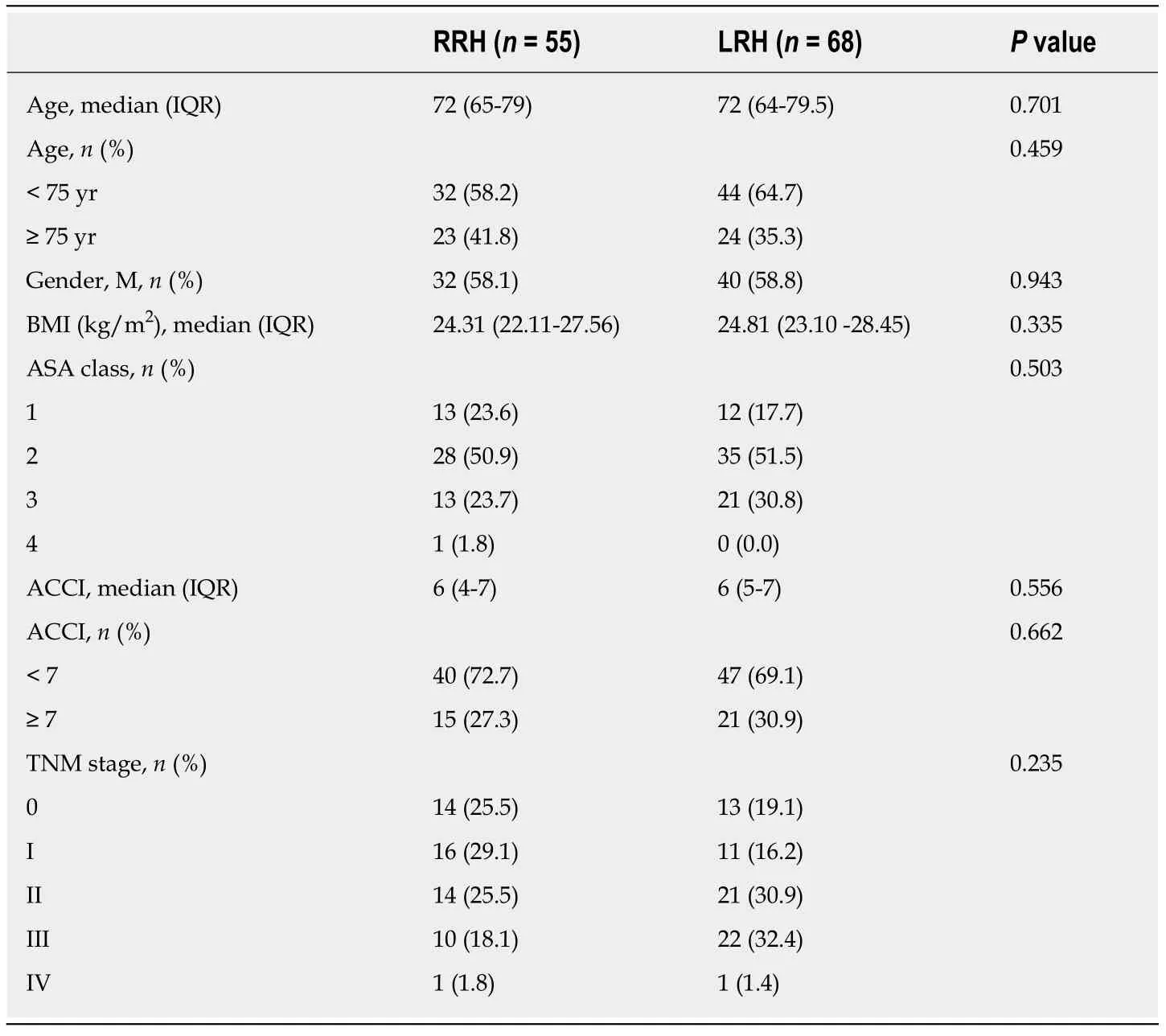
Table1 Pre-operative variables
It is clear that these types of post-operative events have a high impact on recovery,lengthening the hospital stay.Our results suggest that patients who are fit for surgery can benefit from minimally invasive techniques (especially the robotic approach),due to decreased abdominal trauma.On the other hand,patients with severe comorbidities,partially fit for surgery,seem to respond poorly to wall trauma,and tend to respond adequately only to visceral trauma.Therefore,even if associated with poorer recovery outcomes,older age and comorbidities do not contraindicate a robotic approach,but the high costs related to this sophisticated technology should always be taken in consideration in this specific population.
According to international literature,the learning curve of RRH (technical skills necessary to significantly reduce operative time,conversion to open surgery rate and to significantly improve the number of harvested lymph nodes) is complete after 45 procedures[12].Moreover,right colectomy is considered the best procedure to gain proficiency in robotic general and colorectal surgery.Importantly,this case series includes the very first robotic procedures performed in our center:This could have affected both operative time and conversion rate,as well as the incidence of complications.
This study has some limitations.First,the study was retrospective and nonrandomized in design.Another limit is the dichotomization of the continuous variables age and ACCI.On the one hand the categorization tends to impoverish data from a statistical point of view,but on the other hand it gives clinicians a benchmark for daily practice.Furthermore,the coefficients of determination of the regressions were not high and consequently the multivariable models were not completely explicative of the outcomes in analyses.We decided to analyze only pre- andintraoperative variables:Our choice aimed to include in the regression models only potential predictors that could be managed during the planning phase of surgery.Other pre- and post-operative factors will need to be taken in consideration to clearly define all the variables related to the primary and secondary outcomes.To our knowledge,this is the first study to analyze RRH in terms of age and ACCI.According to our results,RRH seems to be associated with a shorter hospital stay and faster restoration of bowel function compared to the laparoscopic approach.Older age(age ≥ 75) and severe comorbidity (ACCI ≥ 7) can affect post-operative recovery,which was significantly longer after both the robotic and laparoscopic approach.
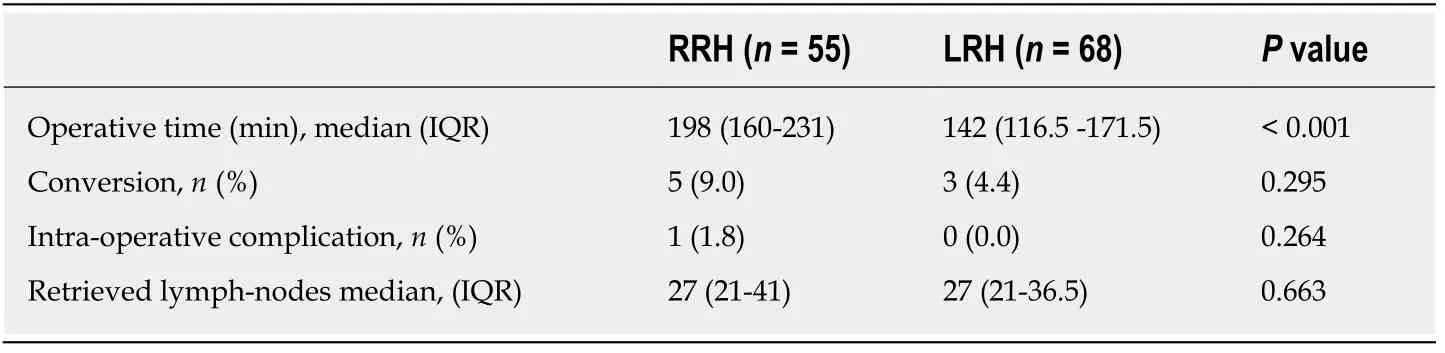
Table2 lntra-operative variables
In conclusion,RRH is safe,feasible and associated with a shorter LOS when compared to LRH,but older age and several comorbidities tend to reduce its benefits.The robotic approach could be considered as a surgical option even in older patients with comorbidities,but its high costs should always be taken into account.Randomized trials are needed to confirm the better results of RRH over LRH for right colonic cancer and further cost-effectiveness studies are required to determine whether the robotic technique can be proposed in elderly oncologic patients with high comorbidity.
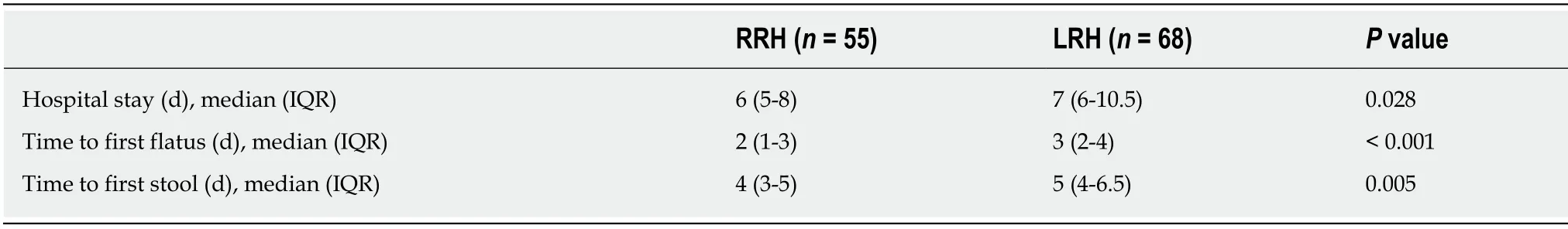
Table3 Post-operative outcomes
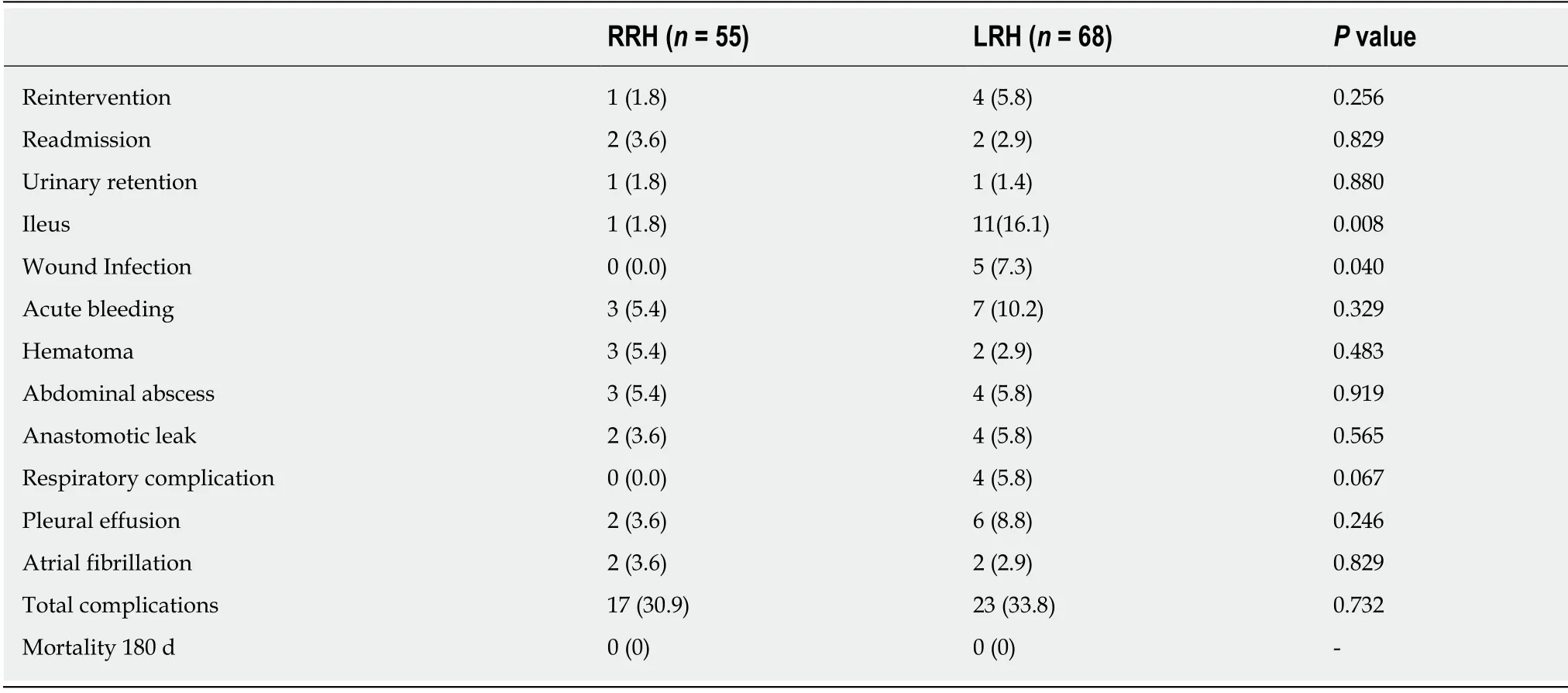
Table4 Post-operative complications,n (%)
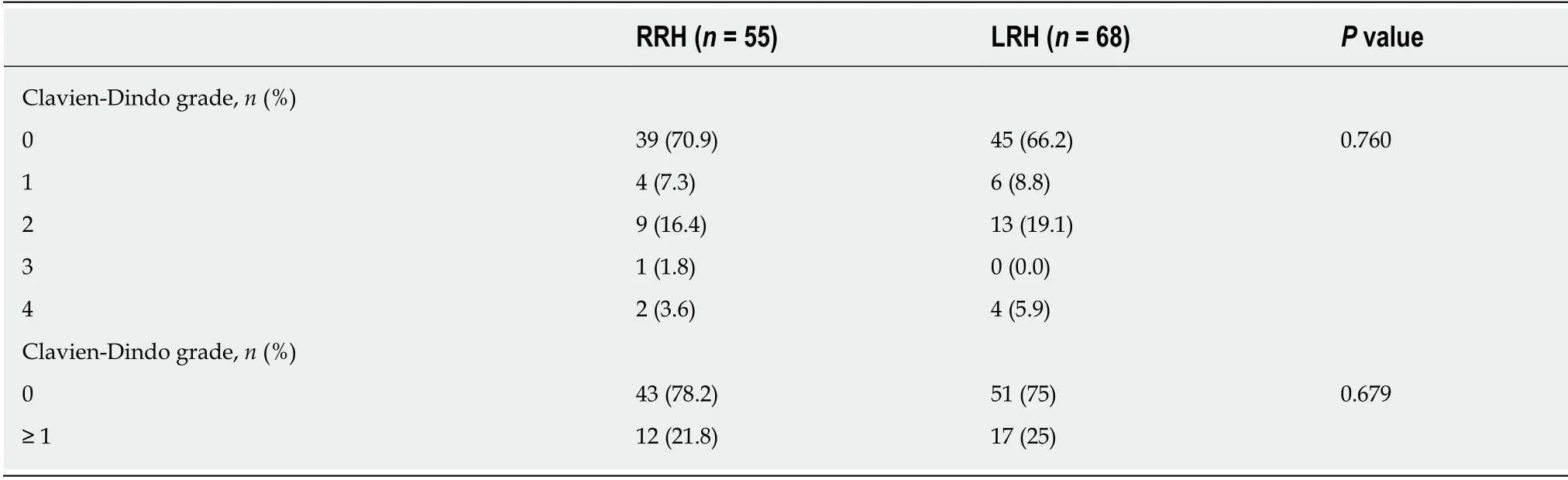
Table5 Post-operative complications according to Clavien-Dindo classification
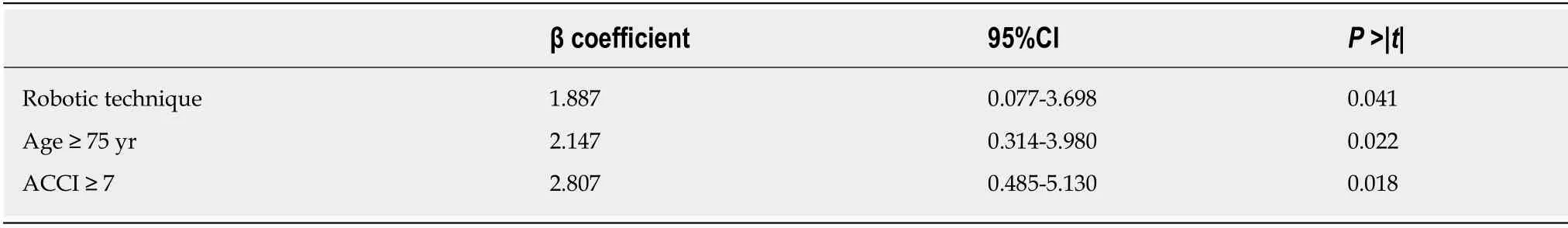
Table6 Multivariable regression model of length of stay
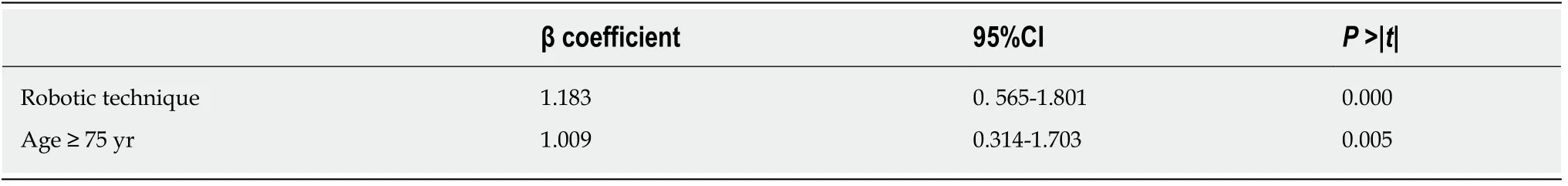
Table7 Multivariable regression model of time to first flatus
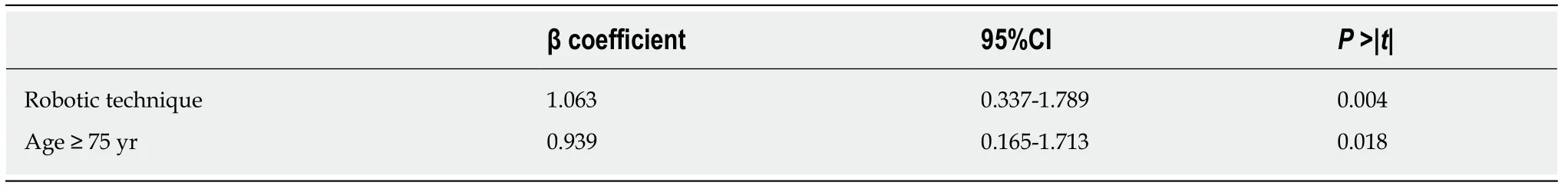
Table8 Multivariable regression model of time to first stool
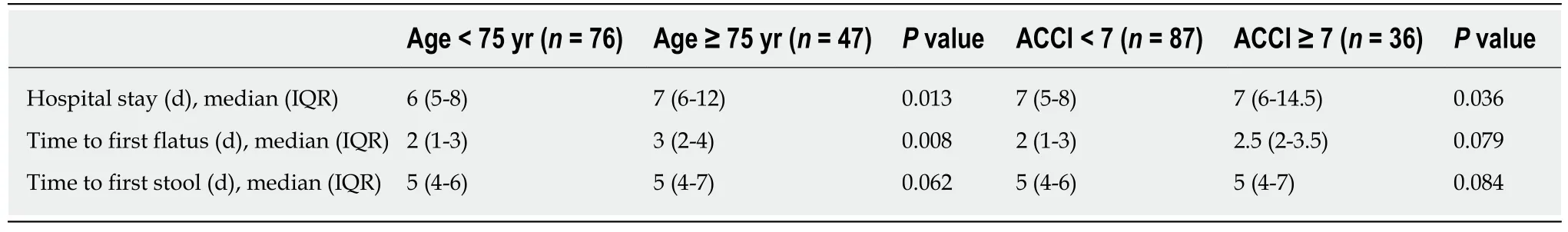
Table9 Post-operative outcomes sorted by age
ARTICLE HIGHLIGHTS
Research background
Several studies have shown the safety,feasibility and oncologic adequacy of robotic right hemicolectomy (RRH).Although robotic surgery is related to better recovery outcomes compared to the laparoscopic approach it is associated with higher costs.In the last decades,life expectancy has constantly improved causing a higher incidence of malignancies.At the same time,elderly patients have more comorbidities and are usually more prone to post-operative complications.Consequently,due to progressive aging of the population,an increasing number of minimally invasive procedures are performed on patients over 75 years old with several comorbidities.
Research motivation
Currently,it is difficult to predict which patients could effectively benefit from a robotic approach.In this study we assessed the burden of age and comorbidities on laparoscopicvsrobotic surgery for right colon cancer.
Research objectives
The aim of the study was to determine the differences in postoperative outcomes in terms of length of hospitalization and bowel function recovery in patients who underwent laparoscopic or RRH.Moreover,our study also evaluated the impact of elderly age and comorbidities on surgical results.
Research methods
We retrospectively collected and analyzed data on patients who underwent laparoscopic and RRH from January 2014 until September 2019.Adult patients with a diagnosis of adenocarcinoma or endoscopically unresectable adenoma of the right colon were included.The study evaluated the short-term outcomes including the length of hospital stay (LOS),time to first flatus (TFF) and time to first stool evacuation.Epidemiologic characteristics,clinicopathologic features,perioperative variables,and post-operative outcomes were analyzed in the two groups(laparoscopic and robotic).Further analysis of outcomes was performed by comparing patients in terms of age and comorbidities.
Research results
LOS,TFF and time to first stool were significantly shorter in the group of patients who underwent robotic surgery.Following multivariable analysis,the robotic technique was confirmed to be predictive of a significantly shorter hospitalization and faster restoration of bowel function;in addition,age over 75 years and the age-adjusted Charlson Comorbidity Index of more than 7 were significant predictors of hospital stay.Following sub-group analysis,patients aged over 75 years had longer LOS and later TFF,while patients with an age-adjusted Charlson Comorbidity Index of more than 7 were associated with a prolonged LOS.
Research conclusions
In conclusion,RRH is feasible and related to shorter LOS when compared to laparoscopic right hemicolectomy,but old age and several comorbidities tend to reduce its benefits.The robotic approach could be taken into consideration as a surgical option even in older patients with comorbidities,but its high costs should always be taken into account.
Research perspectives
Larger prospective studies and randomized trials are warranted to evaluate and compare laparoscopic and RRH,and to analyze the outcomes and costs.Further research into this field should include more extensive data sets to evaluate the impact of age and comorbidities in robotic surgery of the colon;moreover,these studies should also reveal other variables that may assist in selecting patients that could benefit from this expensive minimally invasive technique.
ACKNOWLEDGEMENTS
We thank Dr.Gerardo Cioffi,a native speaker,for reviewing the English language.
 World Journal of Gastrointestinal Surgery2020年6期
World Journal of Gastrointestinal Surgery2020年6期
- World Journal of Gastrointestinal Surgery的其它文章
- Cystic low-grade collecting duct renal carcinoma with liver compression — A challenging diagnosis and therapy:A case report
- Efficacy of the fat-dissociation method for nodal harvesting in gastric cancer
- Role of micronutrients in staging of nonalcoholic fatty liver disease:A retrospective cross-sectional study
- COVlD-19 outbreak and surgical practice:The rationale for suspending non-urgent surgeries and role of testing modalities
