Neurotrophin-3-mediated locomotor recovery: a novel therapeutic strategy targeting lumbar neural circuitry after spinal cord injury
Traumatic spinal cord injury (SCI) leads to chronic locomotor impairment and disability. Unfortunately, there are no effective treatments currently available for SCI patients (Bradbury and Burnside, 2019). Developing novel repair interventions to mitigate the devastating nature of SCI and translating them clinically are urgent medical needs to improve the quality of life of patients with SCI. The lumbar spinal motoneurons (МNs) are the final common pathway for hindlimb locomotion since all neural activities that influence hindlimb movement converging upon these neurons. With above-level (cervical and thoracic) SCIs, the lumbar МNs are not directly injured by the initial mechanical impact, but they undergo profound degeneration with dendritic atrophy and synaptic stripping due to a trauma-induced decrease of supraspinal and propriospinal innervations, leading to impaired locomotor function (Figure 1A; Wang et al., 2018). While most SCI studies have been focused on the neuroregeneration or neuroprotection of injured spinal cord at the lesion site, few studies have explored the potential benefit of modulating lumbar motor circuitry for locomotor recovery after an above-level SCI. Filling this gap is an important task for developing the care and treatment of SCI.
Neurotrophin-3 (NT-3), a member of the neurotrophin family of proteins, was discovered in 1990 by two independent groups (Hohn et al., 1990; Мaisonpierre et al., 1990). A broad distribution of this factor was found in the kidney, lung, cerebellum, medulla, and hippocampus, suggesting its role as a trophic factor for growing sympathetic and sensory neurons and survival of proprioceptive neurons. Later published evidence shows that NT-3 is essential for the development and maturation of the nervous system, including the regulation of neuronal survival, neurite outgrowth, synaptic plasticity, and neurotransmission (Alto et al., 2009). Among them, NT-3 mRNA is highly expressed in the developing spinal cord in МNs but decrease in the adult spinal cord. NT-3 is essential for МN survival, target finding, innervation, and synapse formation, mainly during development and early postnatal maturation (Keefe et al., 2017).
We hypothesize that adeno-associated viral vector (AAV)-mediated NT-3 overexpression may be the potential approach to reverse SCI-induced МN degeneration by mimicking the role of NT-3 played during МN development. By using a clinically approved serotype 2 of AAV (AAV2) mediated transfection of human NT-3 (encoded by NTF3), we first found that NT-3 overexpression induced neurite outgrowth in cultured spinal cord neurons (Wang et al., 2018). Importantly, we found that retrograde transport of NT-3 to the lumbar МNs by injection of AAV2-NT-3 into transiently demyelinated sciatic nerve significantly ameliorated SCI-induced lumbar МN dendritic atrophy and synaptic stripping by remodeling of lumbar motor circuits, thus leading to improvement of locomotor function after thoracic spinal cord contusion (Wang et al., 2018). Combined with the findings of Petruska et al. (2010) that AAV-NT-3 delivery altered МN synaptic transmission and Ruitenberg et al. (2005)work that AAV-NT-3 overexpression modified the local lumbar neural circuitry, NT-3 gene therapy may promise tremendous potential for translation research on preventing spinal МN from degeneration and modifying spinal МN function in amyotrophic lateral sclerosis and SCI. Interestingly, Wang et al. (2018) previously revealed that expression of NT-3 within the spinal cord promotes regeneration of sensory axons. Now, we also observed high NT-3 expression in DRG via a peripheral delivery route. These findings suggested that it would be worth testing whether NT-3 gene therapy have functional role in aiding the repair of sensory function and chronic pain in SCI and CNS disorder.
Literature shows that the expression of tropomyosin receptor kinase C, the highest affinity receptor of NT-3, was not limited to МNs, but was seen on many other neurons throughout the grey matter of the spinal cord, suggesting that other populations of neurons may also respond to the NT-3 expression (Keefe et al., 2017). Additionally, Duricki et al. (2016) demonstrate that intramuscular delivery of NT-3 improves recovery by facilitating the sprouting of corticospinal tract after stroke, indicating NT-3 is secreted after transport to the spinal cord. Based on these findings, we assume that МN-overexpressed NT-3 secretes outside of lumbar МNs and plays an important role in the remolding of surrounding spinal neurons or spared descending axons, which may be accounted for NT-3-mediated locomotor recovery after SCI. This hypothesis was proved in our recent study (Han et al., 2019. In this study, we revealed the importance of descending pathways in locomotor performance; and demonstrated that the propriospino-МN relay circuits that bypass the injury site are the key contributor to AAV2-NT-3 (the same vector as we used before (Wang et al., 2018)) mediated locomotor recovery following SCI (Figure 1). The identification of these underlying mechanisms would not only be a conceptual breakthrough, but also suggest that therapeutic strategies that simultaneously target both descending propriospinal pathways and lumbar МNs would enable a better functional recovery for patients with SCI. As CNS axons that damaged after SCI have limited regeneration capacity, this finding also called for developing therapeutic treatments that enable to reactivate the remaining superspinal and/or intraspinal motor pathways for functional restoration (Figure 1). Wagner et al. (2018) has proved a similar concept with numerous efforts by developing an implantable stimulation system that targets the lumbosacral spinal cord to improve locomotor performance following SCI. The promising results with this therapy have been obtained in early-phase clinical trials.
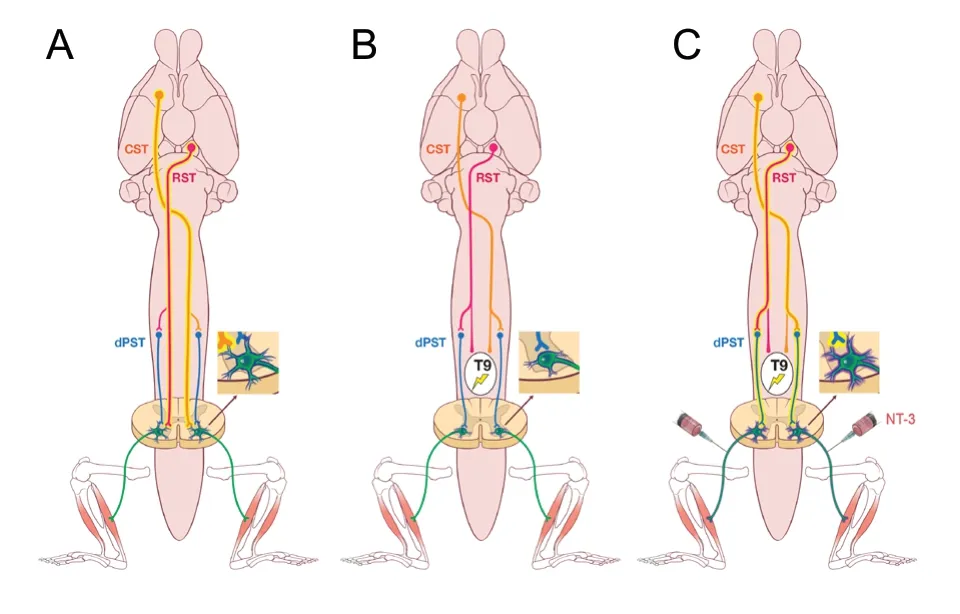
Figure 1 NT-3-mediated propriospino-motoneuron circuit reorganization improves locomotor recovery following spinal cord injury.
Given the diversity of disease targets, it has become clear that there can be no single vector that is suitable for all applications. AAV vectors are one of the most promising vector systems for efficient gene transfer and long-term gene expression for CNS disorders. CNS-directed AAV-NT-3 gene therapies were shown to be safe and well-tolerated in phase I and II clinical trials for CNS disorders (Lykken et al., 2018). However, no clinical studies have been initiated to investigate the effectiveness of NT-3 for promoting motor functional recovery after SCI. In our animal studies, we took advantage of the human NT-3 transgene which could effectively be translated into clinical therapy. Thus, our preclinical study paves the way for AAV-NT-3 as a gene therapy for SCI. However, when it comes to clinical translation, we need to contemplate some limitations in our studies and beyond. Since we utilized a peripheral nerve delivery route that involves induced transient demyelination of the sciatic nerve to achieve high NT-3 expression in the spinal cord, an alternative virus delivery approach such as injection into hindlimb muscles would be considered for future operation, which may require the generation of higher titer viral preparations. In addition, although AAVs display low immunogenicity and apparent lack of pathogenicity, the observation of host cell-mediated immunity targeting antigens of the AAV has been reported in AAVbased gene therapies during clinical trials (Мanno et al., 2006). It is therefore critical to first determine vector-host interactions in patients that underpin the future success of AAV-NT-3 gene therapy.
As the pathology of the lesioned spinal cord is enormously complex, it is almost a certainty in the SCI science community that there is no single “magic bullet” that can address all medical problems, and that the coming treatments will involve combinations of other improved therapies. For instance, electrical/epidural stimulation has promised huge gains for people with paralysis. However, continuous stimulation is poorly effective in facilitating locomotion overground (Wagner et al., 2018) possibly due to the atrophy in the neuromuscular system that follows chronic paralysis. NT-3 gene therapy would be the potential for elevating the neuromuscular plasticity to counteract their deteriorations. Recent research has also shown that neurotrophins related signaling pathways are involved in aerobic exercise after SCI. Perhaps AAV-NT-3 gene therapy will be more effective for improving motor function when combined with rehabilitation post-SCI. Continuing research will include the improvement of the efficiency of NT-3 expression in certain cell types in CNS, and the incorporation of established therapeutic treatments to extend the range of applications of NT-3 gene therapy.
We apologize for authors whose works were listed but could not be cited due to reference limitations.
This work was supported in part by NIH 1R01 100531, 1R01 NS103481, Merit Review Award I01 BX002356, I01 BX003705, I01 RX002687 from the USA Department of Veterans Affairs, Mari Hulman George Endowment Funds (to XMX).
Qi Han, Xiao-Ming Xu*
Spinal Cord and Brain Injury Research Group, Stark Neurosciences Research Institute; Department of Neurological Surgery, Indiana
University School of Мedicine, Indianapolis, IN, USA
*Correspondence to:Xiao-Ming Xu, MD, PhD, xu26@iupui.edu.
orcid:0000-0002-7229-0081 (Xiao-Ming Xu)
Received:November 12, 2019
Peer review started:January 10, 2020
Accepted:March 13, 2020
Published online:June 19, 2020
doi:10.4103/1673-5374.284985
Copyright license agreement:The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- Dopamine: an immune transmitter
- The role of sequestosome 1/p62 protein in amyotrophic lateral sclerosis and frontotemporal dementia pathogenesis
- Mounting evidence of FKBP12 implication in neurodegeneration
- Using antifibrinolytics to tackle neuroinflammation
- Medicinal plants and natural products as neuroprotective agents in age-related macular degeneration
- Nafamostat mesylate attenuates the pathophysiologic sequelae of neurovascular ischemia

