Cost of postoperative complications: How to avoid calculation errors
Roberto De la Plaza Llamas, José M Ramia
Abstract Postoperative complications (PC) are a basic health outcome, but no surgery service in the world records and/or audits the PC associated with all the surgical procedures it performs. Most studies that have assessed the cost of PC suffer from poor quality and a lack of transparency and consistency. The payment system in place often rewards the volume of services provided rather than the quality of patients’ clinical outcomes. Without a thorough registration of PC, the economic costs involved cannot be determined. An accurate, reliable appraisal would help identify areas for investment in order to reduce the incidence of PC,improve surgical results, and bring down the economic costs. This article describes how to quantify and classify PC using the Clavien-Dindo classification and the comprehensive complication index, discusses the perspectives from which economic evaluations are performed and the minimum postoperative follow-up established, and makes various recommendations. The availability of accurate and impartially audited data on PC will help reduce their incidence and bring down costs. Patients, the health authorities, and society as a whole are sure to benefit.
Key words: Morbidity; Postoperative complications; Costs and cost analysis; Economic evaluation; Healthcare costs; Opportunity cost; Clavien-Dindo classification;Comprehensive complication index
INTRODUCTION
Expenditure on health as a proportion of gross domestic product in OECD countries in 2017 ranged from 17.2% in the United States to 4.2% in Turkey[1]. Because of the rising economic costs (EC) deriving from the growing use of expensive technology and population aging, and the need to invest in other basic health areas or global issues such as combating the effects of climate change, expenditure on health must achieve maximum efficiency, incorporating other health benefits and improving the quality of all.
Postoperative complications (PC) are a basic health outcome. Their presence has a negative effect on patients’ quality of life in the short and/or long term and increases the consumption of human, technical and economic resources. An accurate appraisal of the effects of PC would allow us to determine which specific areas are need of investment in order to reduce their incidence, improve surgical results, raise patients’quality of life, and bring down EC.
CURRENT SITUATION
At present no surgery service anywhere in the world systematically records all the morbidity associated with the surgical procedures it performs[2]or submits records of this kind to objective and impartial audit[3]. What is more, the analyses of the EC of PC lack consistency and transparency in terms of the presentation of reports on costs and resource use[4]. Without a complete and impartial registry of PC, the associated EC cannot be determined.
A prospective study by our group evaluating the PC of all surgical procedures at a surgery service found a morbidity rate of 27.7%. Depending on the complexity of the surgery, the PC ranged from 10.7% to 71.4%. In addition, among patients with complications, 51.5% presented two events or more[5].
Even patient death has a negative economic effect. One cost analysis of 1200 patients undergoing major surgery showed that hospital costs incurred by a death were significantly higher than the costs of Clavien-Dindo classification (CDC) grade I to IIIb complications (although they were significantly lower than those associated with grade IV complications in all surgeries)[6]. In pancreatic surgery the costs in patients rescued from PC were 64% lower than those incurred in patients who died due to the complication[7]. In studies validating the association of scales with EC,deceased patients should not be included in the comparative statistical analysis due to possible distortions caused by non-survivor bias[5,6]. In addition to EC, the loss of patient productivity should be taken into account.
Obviously, PC must be monitored after discharge. For example, surgical site infections are a frequent PC[7]; an incidence of 15% has been reported[8,9]and of these as many as 58% occur after hospital discharge[9].
From the hospital perspective, the minimum follow-up period of PC and their EC must be at least 90 d and readmissions must be considered. One prospective study of all interventions carried out at a general surgery service found an overall readmission rate after 90 d of 5.5%[10].
Patelet al[4]conducted a systematic literature review to assess the relationship between EC and the severity of complications in 38 studies that included pancreatic,hepatic, gynecological, urological and thoracic surgeries, and also analyzed the methodologies used. They concluded that EC depend on the type and severity of the complication and are due mainly to prolonged hospitalization. Many of the studies included used general or national databases rather than databases from the hospitals themselves, and all 38 studies included only payer/hospital (i.e., not societal) costs. It was also observed that the studies did not tend to use classifications of complication severity[4].
The association between PC severity and increased EC has been demonstrated in major abdominal surgery[6,11-14], and in another study of all procedures performed at a surgery service[15]. In the latter study for example, even the presence of mild CDC grade 1 complications was found to double postoperative costs from the hospital perspective after cholecystectomy[15].
In some cases it has been observed that complications are profitable for hospitals[16,17]. This is because the payment system rewards the volume of services provided to patients, rather than the quality of the patient’s clinical outcome[18].
ISSUES TO CONSIDER IN THE ANALYSIS OF EC ASSOCIATED WITH PC
To determine the EC related to PC, we must: (1) Quantify and register all PC and the patients affected; (2) Identify and quantify all postoperative EC; and (3) Assess the difference in costs between complicated and non-complicated patients.
Let us now look at these three points in more detail.
Quantification, registration and classification of all PC
The first step is to determine what we mean by PC. We agree with the definition of the CDC, which considers a complication to be any negative event occurring during hospitalization[5,19-21], even if it is asymptomatic or only remotely related to the initial surgical procedure[5,15]. This classification is intended to avoid subjectivity and to ensure that all observers apply the same criteria. This fact entails a series of important consequences: (1) Postoperative patients who have had complications may be classified as uncomplicated: (A) In this case PC-related EC may be attributed to the mean or median costs of patients without complications. This overestimates the costs of patients without complications and brings down the mean EC of patients with complications included in the non-complicated group; and (B) Patients with complications who are wrongly classified as non-complicated do not appear in the PC group (these complications are usually minor). This misclassification pushes up the mean or median costs estimated for particular procedures associated with PC, and erroneously underestimates the total cost of patients with complications; and (2) This leads to errors of classification of diagnosis-related groups (DRG). DRG classify patients who have similar clinical characteristics and similar treatment costs. The purpose of their use is to relate a hospital’s case load to the demand for resources and the costs incurred. Therefore, if a surgery service has a more complex case load according to DRG (as is the case when complications are recorded), this means that the hospital is treating patients who need more hospital resources and, by extension,represent a higher economic outlay. Failure to record all PC would have grave economic consequences for the management unit responsible for patient care because it would be assigned fewer resources (i.e., the amount corresponding to non-complex DRG).
Secondly, PC must be recorded thoroughly. To achieve this, physicians must be formally obliged to prospectively document all complications affecting the patient during or after surgery. But this does not usually occur. In order to record all PC,researchers must evaluate the medical and (above all) the nursing logs and, if possible, specific complications forms in the electronic medical record[5]. An external audit is mandatory: The health authorities have an essential role to play here.
Thirdly, PC must be classified according to a severity or complexity system. We recommend the CDC, published in 2004[19]. This classification system is the most used worldwide, and the article in which it was described currently has 12318 citations[22].The problem with the CDC is that it categorizes the entire postoperative period according to the most serious complication. This means that patients with two or more adverse events are underrepresented, and it has been demonstrated that between 44 and 51.5% of patients with morbidity at general surgery services have two or more complications[5,23]. To overcome this problem, in 2013 Slankamenacet al[24]developed a score that takes into account all the PC classified according to the CDC and summarizes them on a scale between 0 (without complications) and 100 (patient death). This scale, called the comprehensive complication index (CCI), has been validated both clinically[5]and from an economic perspective[14,15].
It would be reasonable to include intraoperative complications in the calculation of EC. In a systematic review of abdominal surgery, Garbenset al[25]observed that intraoperative adverse events significantly increased the total EC, although the studies were of poor quality. However, despite the fact that a clinical classification of these complications has been published[26], these events can only be reported by the surgical team; the surgeons may be fearful of the damage to their reputation of an audit (or its legal consequences) and may be tempted to conceal the complication.This means that there may be major differences and biases in the evaluation of clinical and economic results between different surgery services. In addition, even if they are not taken into account, most of the intraoperative complications that affect EC would be detected during the postoperative period. In any case sensitivity studies might shed further light on this matter.
Identification and quantification of all postoperative EC
The economic evaluation of PC may be performed from a variety of perspectives,depending on who is responsible for paying for them and the intended use of the results of the analysis. Different perspectives will consider different costs and time periods. Examples of these perspectives are the patient, the institution (e.g., the hospital), the target group for specific services (e.g., rehabilitation), the public health service, the public sector, or the sum of all these perspectives (i.e., the social perspective)[27].
ECs are not distributed equally across the hospital stay. Taheriet al[28]concluded that approximately 40% of variable costs are incurred during the first three days of admission. A reduction in length of stay of up to one full day at the end of admission reduces the total cost of care on average by 3% or less. Obviously, the occurrence of PC would change this trend.
It seems reasonable to assess EC until a specific time after patient discharge.Frequently, part of the costs of the care is transferred to the outpatient setting, in particular in patients who are discharged early. So, how long after the operation should EC be assessed? Ideally, all PC should be considered until the patient recovers from the consequences: Imagine a patient with a brain injury that leads to a definite tetraplegia. So, in the best-case scenario, all EC should be considered throughout the patient's life, although this may be impossible to achieve.
As noted by Drummondet al[27]in other economic evaluations, the follow-up time depends on the perspective applied. From the hospital's perspective, we think that the time period should be a minimum of 90 d, or preferably when the patient is able to return to work or their normal activities. However, in the case of certain PC such as a reconstruction of the intestine after an anastomosis dehiscence, this period could be lengthened. If the calculation is made from the perspective of other health agencies,the follow-up period might be for example one year, while from the perspective of the patient and/or family it might be considerably longer, even the entire lifetime[27]. So,the study should indicate the follow-up time used and why.
Table 1 summarizes the different EC included in the literature which we believe should be taken into account in the economic evaluation of PC.
Given that most evaluations of PC-related EC have been carried out from the perspective of the hospital[4], we would like to make some recommendations. It has been argued that taking micro costs into account (i.e., each component of the resources used per patient)[27]is expensive. We do not share this view; with the electronic medical record, the investment for determining these costs is minimal but these costs are still assigned equally, independently of the individual cost. Some examples are: (1)The pharmacy costs associated with each patient are recorded electronically at almost all hospitals; (2) The cost of consumables used during surgical interventions (sutures,gauze, endostaplers, meshes) is very easy to calculate using a barcode reader and to incorporate into the medical record. In advanced surgery this EC is very high.However, operating room EC are usually assessed according to the time taken,regardless of the intervention, and not according to the material consumed; and (3)The cost of diagnostic tests, if they are assigned a unit cost. Consumables should also be individualized.
Specific measurement of each patient’s use of these resources is essential to distinguish between the costs of patients with and without PC. Not taking them into account creates an obvious bias[15]. In addition, we believe that the practice of adjusted the number of stays by DRG is inappropriate[29].
Since the economic evaluation of PC involves the comparison of two clinical evolutions, any costs that are common to both do not need to be quantified; we are interested only in differential costs and results, rather than totals. Any preoperative EC, including the EC of the initial or index surgery or PC caused by postoperative cancer treatments, should be excluded from the analysis.
To determine the cost of PC related to a specific procedure, the operations compared should be as similar as possible in terms of complexity and the patients compared should also be similar in terms of severity. The use of the Charlson morbidity scale can be particularly useful[30].
Table 2 describes the recommendations to be followed in the assessment of EC associated with PC and the data we think should be described in the economic study.
Assessment of the differences in costs between complicated and non-complicated patients
Finally, to determine the EC of PC, the postoperative EC of patients with PC shouldbe subtracted the postoperative EC of patients without PC. That is, costs in patients with and without complications should be compared. If the PC are classified according to the CDC and/or the CCI we can calculate the costs associated with each grade of the CDC or score on the CCI in any patient[15].

Table 1 Types of costs to consider in the economic evaluation of postoperative complications
DISCUSSION
We believe that studies of EC associated with PC should ideally take into account the costs described in Table 1 and the recommendations and clarifications in Table 2.Researchers should specify the ones they use. Some principles have been previously published in the CHEERS statement[31].
In the best-case scenario, it would be possible to compare PC and their associated EC in different surgical procedures and in different hospitals at regional or globallevel. This would indicate the specific problems of each service and procedure, allow the introduction of improvements, and determine quality and efficiency benchmark services. But for this to be possible, care must be taken to measure the same phenomenon with the same tools: That is, assessing the complexity of the procedure and the severity of the patient, the concept of complication, the classification system,the evaluation perspective, the level of the hospital, and so on (Table 2).
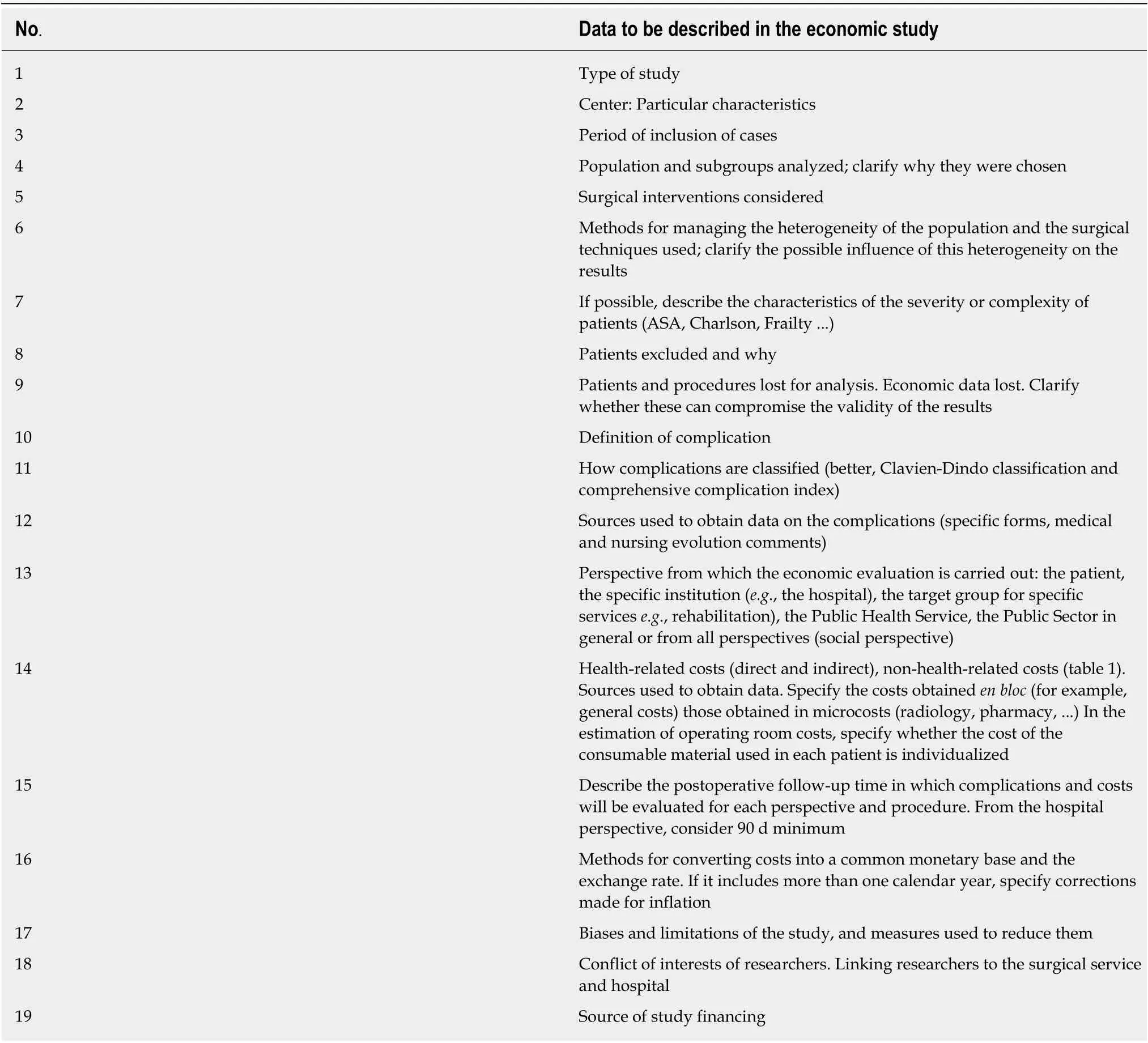
Table 2 Recommendations for the economic evaluations of costs associated with postoperative complications of surgical procedures
Once the PC associated with a surgical procedure at a particular service have been identified, the introduction of a protocol aimed to allow early diagnosis and treatment of complications can help bring down morbidity and mortality rates and can also prove cost-effective[11].
Obviously, without access to results expressed as real and audited PC of the various surgical interventions, it is impossible to consider the centralization of complex surgical procedures or the accreditation of surgical units or of training courses[3]. When these results are available, efficiency studies can be performed.
The training of surgeons is essential for reducing PC. Higher costs have been associated with surgeons who have performed fewer interventions[32,33]and a higher number of intraoperative complications[32].
Outside the public health structure, the payment system in place may reward the volume of services provided to the patient rather than the patient’s clinical outcome.Despite its obvious flaws, many hospitals have used this system for a long time[18].Unfortunately, today there are no economic or social incentives to reduce PC, and the reporting of the results of surgery services all over the world continues to lack transparency. In fact, it is astonishing that in the year 2019 so little should be known about a basic quality outcome of surgical services such as PC. It is an insult to science,patients and society as a whole.
We believe that PC at all surgery services should be audited in an objective and impartial manner by an external assessor. The health authorities would be able to carry out this process quickly and cheaply; using the electronic medical record, the assessment can be carried out in an average of 5 to 10 min per patient[2]. The audit should be maintained over a period of time and should be performed in all patients,not random samples. The audit of the results of the services is also likely to improve surgeons' practices due to the Hawthorne effect, though the mechanisms of this effect and its magnitudes need to be elucidated[34].
The audit can enumerate the complications associated with each surgical procedure and measure their severity, thus identifying the areas where investment in interventions and improvements is most necessary to raise quality and reduce EC.Patients must be informed of the possible outcomes of the operation they are to undergo. The results available at present are unreliable, since they are based on evaluations made by surgeons at the service. This practice underestimates the number of PC, for many reasons: the fact that the better the recording system, the worse the results; the surgeon’s sensation of personal failure; the fear of comparison with other surgeons and/or services; the fear that complex processes will be centralized, and so on. The responsibility for the fact that this audit of all surgical procedures has not been carried out so far in any surgery service in the world lies with the surgeons and the health authorities. Thorough and accurate data on the occurrence of PC will help to bring down their incidence and obviously the EC as well. In addition, it is a mandatory measure to ensure transparency.
CONCLUSION
First of all, all the PC that are associated with a particular surgical procedure must be objectively determined. This is the responsibility of the surgical community and forms part of its commitment towards its patients, society, and science as a whole. Simply recording all PC is likely to reduce their incidence, improve quality and significantly lower EC. The information obtained would help to identify the surgical techniques and clinical management practices with the best postoperative results, to implement preventive measures in order to reduce PC and select the benchmarking services that should take charge of training. Currently, surgical training is not led by the services with the best clinical results. The EC saved can be reinvested in health and/or social areas. Complications should be audited externally and impartially by the health authorities, and in a universal, permanent manner in all surgical patients. Hospitals with the best results should be rewarded economically and not according to a payment system that may favour poor outcomes. This payment would only be justified in centres of proven quality.
ECs associated with PC should also be reported in a standardized way[31].Appropriate and accurate methods should be used to track the use of resources and to estimate EC. Accounting must be accurate and detailed. Although the most frequently used perspective is that of the hospital, health authorities and health managers should bear in mind that EC associated with PC are much higher than the published figures,if the estimation includes future direct EC, non-health-related EC and indirect EC which have major repercussions for society and for patients.
Specifically, we think that recording and auditing of PC is likely will become the measure of the greatest impact on healthcare transparency, quality of care and the reduction of ECs in the coming decades.
 World Journal of Gastroenterology2020年21期
World Journal of Gastroenterology2020年21期
- World Journal of Gastroenterology的其它文章
- Tailored classification of portal vein thrombosis for liver transplantation: Focus on strategies for portal vein inflow reconstruction
- Alternative uses of lumen apposing metal stents
- lnnate immune recognition and modulation in hepatitis D virus infection
- Use of zebrafish embryos as avatar of patients with pancreatic cancer: A new xenotransplantation model towards personalized medicine
- Gan Shen Fu Fang ameliorates liver fibrosis in vitro and in vivo by inhibiting the inflammatory response and extracellular signalregulated kinase phosphorylation
- Periportal thickening on magnetic resonance imaging for hepatic fibrosis in infantile cholestasis
