Call for accurate statistical data to solve snakebite conundrum in India
Saurabh Bhargava, Kiran Kumari, R.K. Sarin, Rajvinder Singh✉
1Department of Genetics, M.D. University, Rohtak-124001 Haryana, India
2Andhra Pradesh Forensic Science Laboratory, Mangalgiri, Guntur, Andhra Pradesh-522004, India
After a prolonged debate and discussion, the World Health Organization (WHO) relisted ‘snakebite’ under Category ‘A’ of ‘Neglected Tropical Diseases’ (NTDs) in June 2017 hoping to diminish its burden on people. Earlier, in March 2009, WHO added snakebite to its official list of NTDs but later downgraded to ‘Other Neglected Conditions’, a list reduced in importance[1,2]. Obviously, the recent inclusion of snakebite in NTDs was due to the estimation of huge toll of deaths due to snake envenomation in tropical countries as supported by the multiple reports. This inclusion will expedite the process of developing better management protocols and infusing funds for such affected countries.
However, a significant question here is whether the estimation of snakebite cases is accurate enough to publicise the authentic figures. Snakebite is a problem of resource poor tropical countries which usually lacks a solid central registry system of record keeping. Even when such record keeping is in place, yet people out there may not be aware enough for such measures and they don’t bother to register such cases. Snakebite incidences in such circumstances could definitely affect the national statistical figures of snakebite in any country.
Many scientific reports and WHO reports have suggested that India leads the chart of mortality and morbidity caused by snakebites and envenomations contributing almost 50% of world’s burden by snakebites[3,4]. However, true figures remained elusive and the estimates range from 10 000 to 50 000 annual deaths in India. These estimates are usually based on extrapolation of smaller and regional studies. Nationally representative “Million Death Study” conducted by the Registrar General of India projected 45 900 annual deaths in India due to snake envenomation on the basis of statistical data generated from randomly selected 6 671 areas from 28 states and 7 Union territories of India between 2001 and 2003[5]. The WHO in 2005 has quoted similar figures about snake envenomations in India[3]. In 2008, an international study funded by the WHO estimated the global burden of snakebites to be around 1 841 000 snakebite incidences with around 94 000 annual deaths across the world[4]. They reported around 81 000 envenoming and nearly 11 000 annual deaths due to snakebite in India.
On the other hand, the National Health Profile (NHP) maintained by the Central Bureau of Health Intelligence, Government of India reported average annual snakebite mortality of just 1 215 across India from 2010 to 2016[6]. This is the data that is quoted by the government for various purposes including policy making. The National Crime Records Bureau (NCRB) working under the Ministry of Home Affairs of Government of India reported an average 8 507 annual deaths due to snake envenomation across India during 2010-2016[7]. Data published by both, NHP and NCRB depict a huge difference in official figures of snakebites and is quite underreported than other scientific epidemiological studies.
However, a well designed field survey conducted in Tamil Nadu in India suggested that even 50 000 snake envenomed mortality is underreported, and the actual burden of snake envenomation could be even more. This extensive field survey of 28 494 people from thirty villages in state of Tamil Nadu suggested around 10 000 annual deaths from snake envenomation[8] and it was in contrast with around 3 100 snakebite deaths suggested by nationally representative “Million Death Study” conducted by the Registrar General of India, average 44 annual deaths by NHP reports during 2010-2017, and average 638 annual deaths by NCRB from 2011 to 2015.
Similarly, NCRB reported 368 deaths due to snake envenomation during 2011-2015 in the state of Haryana, whereas NHP reported only 32 deaths over same period in same region. However, another independently conducted government hospital based epidemiological profiling of the same region reported at least 130 deaths due snake envenomation in Haryana during 2011-2015[9]. Similar disparity between government records of snakebite and independently conducted surveys have been reported by researchers from West Bengal[10].
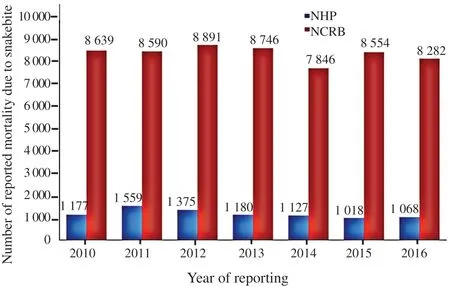
Figure 1. Number of reported mortalities due to snakebite.
Lack of consensus in epidemiological database of snake envenomations is visible amongst data of different government organizations. The disparity could have few important attributes (Figure 1). Firstly, the government data on snakebite generally remains limited to victims reporting to government hospitals and dispensaries, while it may not account for cases received at private medical infirmary. Secondly, the government data also does not include cases where medical help was never sought. The role of socio-economic factors in reporting and recording of such cases should not be deferred. Underprivileged people evade expensive snake anti-venom treatment due to financial restraints and instead prefer either a home remedy or a traditional village healer. These situations result in underreporting of snakebite incidence and thereby add to the burden of snakebite mortality and morbidity.
For better management of problem, the accurate data-basing of such medical emergencies is mandatory from all corner of the country. Accurate epidemiological findings can result in planning and implementing of region specific awareness, preventive and rehabilitative programmes. It will also streamline life saving snake anti-venom distribution. The appropriate need based distribution of antivenom can substantially reduce the burden of snakebites when there are reports pointing a huge gap in production and need of antivenoms in many regions. Inclusion of snakebites in NTDs has created a unique opportunity for government and other stakeholders of affected countries to come up with better and innovative ideas for mapping and profiling of snakebite associated mortality.
Awareness amongst poor villagers about reporting in hospitals during medical emergencies instead of traditional healers will lead to more incidences being included in national databases. This can be achieved by reducing their hospitalization expenditure by government sponsored incentivization for treatment of such neglected medical emergencies. Administration sponsored annual or bi-annual surveys should be conducted at village/block/district level to conclusively prepare epidemiological profiles. We suggest inter-ministerial and interdepartmental communication and co-operation which should result in better profiling of snakebite problem from across the country. This can be achieved using uniform indexing and classification of disease and by selecting common centres of data collection.
Thus, this correspondence suggests an administrative push for compulsive and conclusive reporting of snakebite incidences and need of refining long-term complications in generating correct data of snakebite cases.
Conflict of interest statement
Authors declare no conflict of interest. The NHP and NCRB data were accessed from datasets provided in public by respective government departments and are duly cited.
Authors’contributions
All authors contributed equally in conceptualizing the article, retrieving related literature and drafting final manuscript.
 Asian Pacific Journal of Tropical Medicine2020年4期
Asian Pacific Journal of Tropical Medicine2020年4期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Crimean-Congo hemorrhagic fever: etiology, diagnosis, management and potential alternative therapy
- Expert consensus guidelines on clinical use of Xiyanping injection for acute infectious diseases
- Provincial clustering of malaria in Iran between 2005 and 2014
- Epidemiological, molecular characterization and risk factors of human brucellosis in Iran
- Antimalarial activity of the aqueous extract of Euphorbia cordifolia Elliot in Plasmodium berghei-infected mice
- COVID-19 international outbreak and the need for a suitable estimation model: A second-order polynomial equation with constant coefficients based on imported infected cases seems inadequate
