Malignant solitary fibrous tumor of the pancreas with systemic metastasis:A case report and review of the literature
Hao Geng, Yu Ye, Yun Jin, Bai-Zhou Li, Yuan-Quan Yu, Yang-Yang Feng, Jiang-Tao Li
Hao Geng, Yu Ye, Yun Jin, Yuan-Quan Yu, Yang-Yang Feng, Jiang-Tao Li, Department of General Surgery, The Second Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou 310009, Zhejiang Province, China
Bai-Zhou Li, Department of Pathology, The Second Affiliated Hospital, College of Medicine,Zhejiang University, Hangzhou 310009, Zhejiang Province, China
Abstract
Key words: Solitary fibrous tumor; Pancreas; Malignant; Doege-Potter syndrome; Case report
INTRODUCTION
Solitary fibrous tumor (SFT), first described in 1870, was established as a pleural neoplasm by Klemperer and Rabin in 1931[1].This tumor is commonly found in serosal membranes, the dura of the meninges, and deep soft tissues.It is now recognized as a type of fibroblastic mesenchymal neoplasm of intermediate biological potential characterized by the pathognomonicNAB2-STAT6gene fusion[2].Only a few reports on malignant pancreatic SFT have been previously published.We present herein the first case of malignant pancreatic SFT with typical Doege-Potter syndrome and,hepatic and bone metastases.
CASE PRESENTATION
Primary complaints
A 48-year-old man was admitted to our hospital with 1-year history of pancreatic and liver tumors.The tumors were accidentally found when the patient went to a local hospital after a sudden incidence of fainting.It is noteworthy that he reported of recurrent incidences of hypoglycemia, however, there was no history of any endocrine disease.
History of past illness
His medical history showed that he had been treated eight times for metastatic liver tumor by transcatheter arterial chemoembolization and once by radioactive seed implantation.Five years before presentation, he had undergone an excision of a tumor of the right pterygopalatine fossa.
Physical examination
Physical examination showed no other positive findings except that the liver was enlarged and palpable.
Laboratory and imaging examinations
Laboratory investigations showed an abnormal hemogram, including hemoglobin of 123 g/L (reference range:131-172 g/L), neutrophils 72.8% (reference range:50%-70%)and lymphocytes 10.8% (reference range:20%-40%).The results of liver and kidney function were normal.The levels of serum tumor markers (CEA, CA 19-9, CA 12-5,and AFP) were all within normal limits.
Computed tomography (CT) imaging of the abdomen showed a 4.7 cm welldefined mass located in the lower posterior part of the body of the pancreas (Figure 1A).Non-uniform enhancement was observed from the arterial to portal venous phase.Meanwhile, multiple nodules and masses of various sizes were seen in the liver (Figure 1B).The largest one was located in the segment VIII of the liver with a diameter of about 15.9 cm.No obvious dilatation of intrahepatic and extrahepatic bile ducts was observed.
Pancreatic magnetic resonance (MR) imagining also confirmed a hypervascular tumor located in the body of the pancreas and multiple tumors located in the liver.Those tumors were hypointense on T1-weighted MR images and hyperintense on T2-weighted MR images.

Figure 1 Computed tomography imaging of the abdomen.
For a complete preoperative evaluation, fluorine-18 fluorodeoxyglucose positron emission tomography/CT (18F-FDG PET/CT) was performed.Images from the PET/CT revealed that both the pancreatic and the metastatic liver lesions had an increased uptake of the tracer FDG.Besides, the thoracic and lumbar vertebrae,humerus, femur, scapulae, ribs, sacrum, and pelvis also showed heterogeneous FDG uptake (Figure 2).
Further diagnostic work-up
A liver biopsy guided by B-mode ultrasound confirmed that the tumor was an SFT/hemangiopericytoma (Grade 2).
FINAL DIAGNOSIS
The patient was eventually diagnosed with a malignant SFT of the pancreas with Doege-Potter syndrome and metastases to the liver and bone.
TREATMENT
In order to improve the quality of life of the patient and control the growth of the mass, a distal pancreatectomy, involving the body and tail and splenectomy, was performed after a multidisciplinary discussion, and the metastatic neoplasm in the left lateral lobe of the liver was also resected.
OUTCOME AND FOLLOW-UP
On gross examination, the pancreatic specimen measured 15 cm × 6 cm × 2 cm, which contained two well-circumscribed non-encapsulated masses.The larger lesion measuring 6.5 cm × 5 cm, had a soft fleshy cut surface containing hemorrhagic and necrotic areas (Figure 3A).Another metastatic lesion located in the left lobe of the liver measured 14 cm × 12 cm × 4 cm with a pale-yellow cut surface (Figure 3B).All the resection margins were free of tumor.On histopathological examination, it was found that the tumor was composed of abundant heterogeneous spindle cells (Figure 4A).A localized area of necrosis (Figure 4B) was visualized and there were 4-5 mitotic figures (Figure 4C) per 10 high-power fields (HPFs).Immunohistochemical (IHC)analysis of the resected tumor revealed that the tumor cells were diffusely positive for STAT6 (Figure 4D), CD34, CD31, Bcl-2, cell proliferation marker Ki-67, PHH-3, and D2-40, and negative for glial fibrillary acidic protein, S100, smooth muscle actin(SMA), Desmin, delay of germination 1, CD117, and receptor tyrosine kinase.The proliferation index of Ki-67 was observed to be above 10%.The patient's postoperative recovery was uneventful.Furthermore, a transcatheter arterial chemoembolization procedure was also performed to eliminate the residual tumor of the right liver, and postoperative follow-up at 6 mo demonstrated good results(Figure 5).
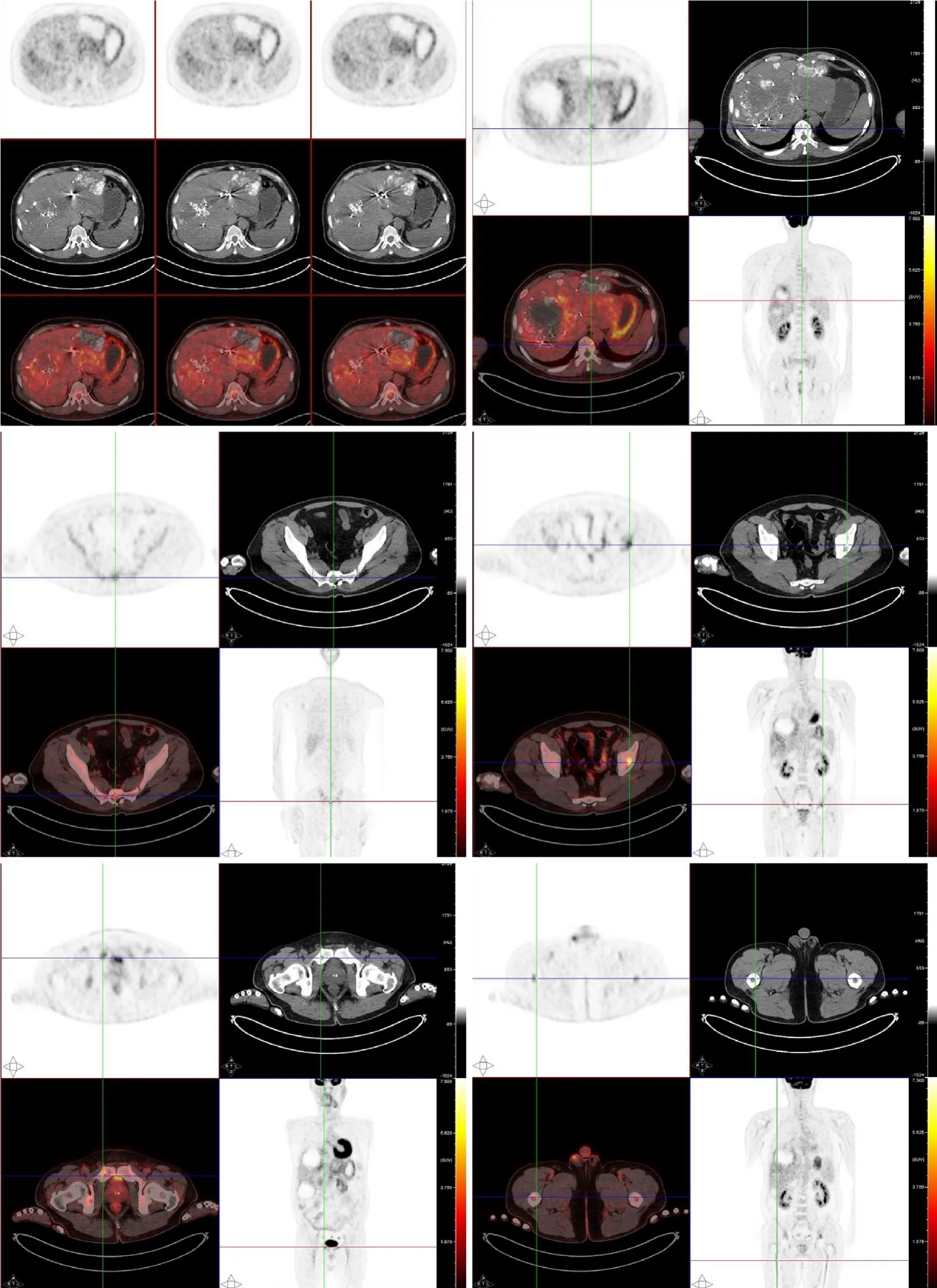
Figure 2 Systemic fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography scan.
DISCUSSION
SFTs are now considered to occur anywhere in the body, but the pancreatic fibrous tumor is still rarely recorded in the literature:only 22 cases have been reported since 1999 (Table 1).The vast majority of the cases presented with benign features, and only one case was defined as being malignant, based on its histological features[3].The case we present here, to our knowledge, is the first malignant pancreatic SFT with clinical and pathological evidence of liver and bone metastases.
Until now, there is no one comprehensive definition of malignant SFTs.According to the previous literature, abdominal pain is the most common presentation of clinical syndrome in a pancreatic SFT (10/22 cases, 45.45%), followed by an incidental abdominal mass (8/22 cases, 36.36%) and obstructive jaundice.Infrequently, patients may present with paraneoplastic syndromes.The clinical manifestations were commonly refractory and recurrent hypoglycemia, which is the main clinical characteristic of Doege-Potter syndrome.Increased secretion of a pro-hormone form of the insulin-like growth factor II has been confirmed to be the primary mechanism of hypoglycemia according to a study[4].Hanet al[5]reported that SFTs with Doege-Potter syndrome were often malignant.Our case showed typical features of Doege-Potter syndrome at the onset of disease and also the malignant features.However,these symptoms were non-specific.
Radiologically, homogeneous enhancement of the lesion in the arterial phase to portal venous phase on CT as well as low T1 signal intensity and high T2 signal intensity on magnetic resonance imaging can be observed in most of the cases[2].The non-typical feature makes it difficult to distinguish SFTs from the other soft tissue tumors[6].Particularly, it was reported that a malignant and larger tumor may present with hemorrhage, calcifications, cystic areas and so on[2].A non-uniform enhancement was observed in the image examinations of our case that showed similar features.
Furthermore, although a higher FDG uptake on18F-FDG PET/CT may be a sign of a malignant SFT, the diagnostic utility is still debatable due to its imperfect sensitivity[7].However, in our case, the18F-FDG PET/CT was useful in the differential diagnosis of benign and malignant SFTs and evaluation of clinical significance.Thus,18F-FDG PET/CT examination is still a recommendation for the full evaluation of suspicious malignant tumors.
Recently, theNAB2-STAT6fusion gene was found to express a unique molecular feature in 100% of SFT cases[8].Thus, compared with other conventional IHC markers like CD34, STAT6 has been proved to be more sensitive (98%) and specific (85%) for SFT.Furthermore, a previous study reported that a higher risk of SFT aggressive behavior may be associated with specificNAB2-STAT6fusion variants[9], which could be a biomarker for identifying the distinct molecular feature of malignant SFTs.
For pathologic features, grossly, the pancreatic SFTs range from 2.0-18.5 cm in diameter[10,11].Tumors are usually well-circumscribed with a fibrous pseudocapsule.The cut surface may show a wide range of patterns from firm, white to tan, and fleshy mass with hemorrhage, necrosis, or calcification usually presented in large or malignant cases[2].Histologically, a typical “patternless pattern”,i.e., various atypical spindled cells arrayed randomly within the stroma, can be seen in most cases (Table 2).People have defined malignant SFTs based upon its special histologic features:≥ 4 mitotic figures per 10 HPFs, necrosis or hemorrhage, increased cellularity, nuclear pleomorphism, and a large size (> 10 cm).The histological results of our case meet these criteria and show high-grade malignant manifestations.However, a poor correlation with patients outcomes[12]has been seen as low validity in predicting the biological features of SFTs.Therefore, pathologists treat SFT as a neoplasm of intermediate biological potential.Furthermore, complete surgical resection is the mainstay of treatment for pancreatic SFTs and good results were reported (Table 2).Unfortunately, almost no information has been provided concerning systemic treatments for malignant pancreatic SFTs.For this reason, a multidisciplinary discussion, especially with the participation of pathologists, is recommended before initiation of treatment procedures for patients with an advanced stage of the disease.

Figure 4 Photomicrographs of histologic and immunohistochemical staining.
CONCLUSION
In summary, we present a malignant pancreatic SFT with systemic metastasis and typical Doege-Potter syndrome features.The diagnosis and prognosis evaluation of malignant SFTs rely on more accurate criteria combined with clinical, IHC, and histological evidence.Furthermore, prospective studies are needed to provide greater evidence about the systemic management of malignant pancreatic SFTs.

Table 1 Clinical features of pancreatic solitary fibrous tumors

Table 2 lmmunohistochemical and histological features along with outcomes of pancreatic solitary fibrous tumors
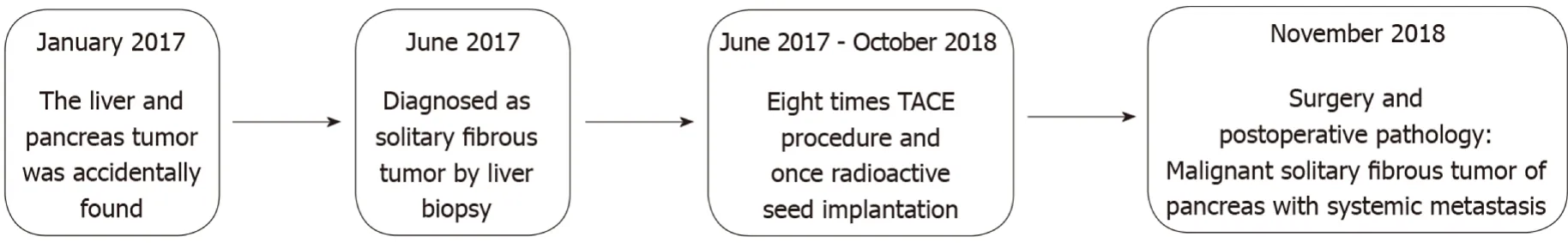
Figure 5 Timeline.
 World Journal of Clinical Cases2020年2期
World Journal of Clinical Cases2020年2期
- World Journal of Clinical Cases的其它文章
- Awareness during emergence from anesthesia:Features and future research directions
- Risk factors for adverse cardiac events in adults with fulminant myocarditis during hospitalization
- Malignant tumors associated with Peutz-Jeghers syndrome:Five cases from a single surgical unit
- Pathogens causing diarrhoea among Bangladeshi children with malignancy:Results from two pilot studies
- One-year rotational relapse frequency following conventional circumferential supracrestal fiberotomy
- LINX® reflux management system to bridge the “treatment gap” in gastroesophageal reflux disease:A systematic review of 35 studies
