Severe hyperlipemia-induced pseudoerythrocytosis - Implication for misdiagnosis and blood transfusion:A case report and literature review
Xi-Chen Zhao,Bo Ju,Na Wei,Jian Ding,Fan-Jun Meng,Hong-Guo Zhao
Xi-Chen Zhao,Bo Ju,Na Wei,Department of Hematology,The Central Hospital of Qingdao West Coast New Area,Qingdao 266555,Shandong Province,China
Jian Ding,Department of Clinical Laboratory,The Central Hospital of Qingdao West Coast New Area,Qingdao 266555,Shandong Province,China
Fan-Jun Meng,Hong-Guo Zhao,Department of Hematology,The Affiliated Hospital of Qingdao University,Qingdao 266000,Shandong Province,China
Abstract BACKGROUND Severe hyperlipemia(SHLE)has an impact on the results of many kinds of laboratory tests.Complete blood count(CBC)examination by automated blood cell counter(ABCC)is a quick and convenient measurement for screening abnormalities of blood cells that are triggered by various pathogenic insults in disease diagnosis and for monitoring changes in the treatment of existing hematological conditions.However,CBC results are frequently affected by many intrinsic and extrinsic factors from blood samples,such as in the setting of hypergammaglobulinemia and certain anticoagulants.SHLE could also affect CBC results.CASE SUMMARY A 33-year-old Chinese male presented with painful foot numbness and abdominal pain.He was initially misdiagnosed as having a myeloproliferative neoplasm(MPN)because of the marked abnormalities in CBC examination by the ABCC.Morphological evaluation of the bone marrow smears and biopsy showed no evidence of MPN.Gene mutations in Breakpoint cluster regions-Abelson murine leukemia viral oncogene homologue 1(BCR-ABL1),Janus kinase 2(JAK2),calreticulin(CALR),myeloproliferative leukemia virus(MPL),and colony-stimulating factor 3 receptor(CSF3R)were negative.Having noticed the thick chylomicron layer on blood samples and the dramatically fluctuating CBC results,we speculated that the fat droplets formed by shaking the blood samples in the setting of SHLE were mistakenly identified as blood cells due to the limited parameters of ABCC.Therefore,we removed a large part of the chylomicron layer and then reexamined the CBC,and the CBC results,as we expected,differed significantly from that of the sample before the chylomicron layer was removed.These significant differences had been validated by the subsequently repeated laboratory tests by measuring dual blood samples that the chylomicron layer was removed in one sample and was not in another,and comparing the CBC results.Computerized tomography reexamination of the upper abdomen revealed an exudative lesion surrounding his pancreas.After intensive consultation,definitive diagnosis was made as recurrent pancreatitis,hyperlipemia and pseudoerythrocytosis.CONCLUSION SHLE may become a potential cause of misdiagnosis of hyperlipemia-related diseases as MPNs and the resultant mistreatment.It may also lead to the misinterpretation of transfusion indications in patients with hematological disorders who critically need blood transfusion for supportive treatment.
Key Words:Case report;Hyperlipemia;Fat droplet;Pancreatitis;Pseudoerythrocytosis;Blood transfusion indication
INTRODUCTION
Severe hyperlipemia(SHLE)has a significant impact on the results of many kinds of laboratory tests.Complete blood count(CBC)examination by automated blood cell counter(ABCC)is an important measurement for screening abnormalities of blood cells that are triggered by various pathogenic factors in disease diagnosis and for monitoring changes in the treatment of existing hematological conditions.However,CBC results are frequently affected by many intrinsic and extrinsic factors in blood samples,such as in the setting of hypergammaglobulinemia and certain anticoagulants.SHLE can also affect the CBC readings.Here,we report a recurrent pancreatitis patient who was initially misdiagnosed with myeloproliferative neoplasm(MPN)due to mistaken readings by the ABCC,but he was finally diagnosed with SHLE-induced pseudoerythrocytosis.It is speculated that the fat droplets in blood samples of individuals with SHLE are mistakenly identified as blood cells due to the limited parameters of ABCC.This phenomenon may become a potential cause of misdiagnosis of hyperlipemia-related diseases as MPNs and the resultant mistreatment,as reported in this paper.It may also lead to the misinterpretation of indications for blood transfusion in patients with hematological disorders who critically need blood transfusion as supportive treatment,such as in retinoic acid treatment for patients with acute promyelocytic leukemia and in L-asparaginase treatment for patients with acute lymphoblastic leukemia.
CASE PRESENTATION
Chief complaints
Painful foot numbness for 2 mo and abdominal pain for 2 d.
History of present illness
A 33-year-old Chinese male was referred to the emergency department for complaints of painful foot numbness for 2 mo and abdominal pain for 2 d,with the absence of fever,chills,headache,dizziness,cough,expectoration,vomiting,diarrhea,and abnormalities in the urine and feces.Upon physical examination,except for moderate tenderness in his left upper abdomen,no other abnormalities were found.His CBC showed the following results:white blood cell(WBC)count,11.65 × 109/L;absolute neutrophil count(ANC),8.85 × 109/L;red blood cell(RBC)count,4.59 × 1012/L;hemoglobulin(Hb)value,225 g/L;and platelet(Plt)count,229 × 109/L.Serum amylase level was 33 U/L.Computerized tomography(CT)examination of his abdomen revealed the presence of adiposis hepatica,without other abnormalities.Ultrasonic inspection of his viscera revealed no obvious abnormalities in the liver,gallbladder,bile duct,pancreas,spleen,kidneys,ureter,or bladder.He was prescribed an antibiotic treatment with etimicin,and his abdominal pain was not relieved.The next day,reexamination of his CBC and serum amylase showed the similar results.He was thought to have erythrocytosis,and his abdominal pain was thought to result from a thrombotic event in the mesenteric vessels,which was probably due to the increased blood viscosity and enhanced Plt activities.So he was admitted to the hematology department.
History of past illness
He had a history of acute pancreatitis 2 years previously.
Physical examination
His height was at 176 cm;body weight 76.0 kg.His body temperature was at 37.2 ˚C;breathing rate 22 bp per min;heart rate 86 bp per min;blood pressure 126/78 mmHg.Upon physical examination,except for the bruise-looking appearance and moderate tenderness in his left upper abdomen,no other abnormalities were recorded.Conspicuous mucocutaneous plethora,hemorrhage,jaundice and exanthemata were not presented.No significant signs of nervous system,respiratory system,cardiovascular system,urogenital system and skeletal musculature system were found.
Laboratory examinations
On admission,the CBC showed as follows:WBC,8.97 × 109/L;ANC,6.66 × 109/L;hematocrit(Hct),37.6%;RBC,4.15 × 1012/L;Hb,204 g/L;mean corpuscular volume(MCV),90.5 fL;mean corpuscular hemoglobin(MCH),41.9 pg;mean corpuscular hemoglobin concentration(MCHC),463 g/L;and Plt,218 × 109/L.Urinalysis showed ketone bodies 3+,blood 1+,protein 3+,and glucose 3+.Examination of the coagulation profile and biochemical test could not be performed due to SHLE.The tests for hepatitis virus A,B,C,and E and a series of tumor markers were negative.Serum testosterone level was 175 ng/L.Morphological evaluation of the bone marrow(BM)smears and biopsy showed no evidence of MPN.Cytogenetic analysis of BM culture reported a normal karyotype of 46,XY[25].Gene mutations inBreakpoint cluster regions-Abelson murine leukemia viral oncogene homologue 1(BCR-ABL1),Janus kinase 2(JAK2),calreticulin(CALR),myeloproliferative leukemia virus(MPL),colony-stimulating factor 3 receptor(CSF3R)were negative.These laboratory tests did not meet criteria for the diagnosis of MPN.
Further investigation of the abnormalities in CBC examination
Having noticed the thick chylomicron layer and dramatically fluctuating CBC results,we speculated that the fat droplets formed by shaking the blood samples in the setting of SHLE were mistakenly identified as blood cells due to the limited parameters of ABCC.Therefore,we removed a large part of the chylomicron layer and then reexamined the CBC and biochemical tests.The CBC showed:WBC,8.34 × 109/L;ANC,6.43 × 109/L;RBC,3.37 × 1012/L;Hb,118 g/L;and Plt,164 × 109/L.Biochemical tests showed:Triglycerides(TGs),3.96 mmol/L;total cholesterol(TC),9.74 mmol/L;and low density lipoprotein(LDL),5.67 mmol/L.
To determine whether the erythrocytosis was truly caused by SHLE,we drew dual blood samples,measured them(the chylomicron layer was removed in one sample and was not in another)at the same time,and then compared the CBC results.As we expected,there was a significant difference in the CBC results.While the CBC readings in the sample without removing the layer showed WBC,10.94 × 109/L;ANC,8.86 × 109/L;RBC,4.26 × 1012/L;Hb,208 g/L;and Plt,287 × 109/L;the readings in the sample in which a large part of the layer was removed showed WBC,4.34 × 109/L;ANC,2.88 ×109/L;RBC,3.69 × 1012/L;Hb,114 g/L;and Plt,215 × 109/L.Subsequently,the repeated tests using this method yielded the similar results(listed in Table 1),confirming the contribution of SHLE to the formation of pseudoerythrocytosis.
Imaging examinations
On 5thday of hospitalization,CT reexamination revealed an exudative lesion surrounding the pancreas,in accordance with the diagnosis of pancreatitis.
FINAL DIAGNOSIS
After intensive consultation with specialists in gastroenterology,ultrasonography and radiology,a definitive diagnosis was made as recurrent pancreatitis,hyperlipemia and pseudoerythrocytosis.
TREATMENT
After the definitive diagnosis of recurrent pancreatitis,hyperlipemia and pseudoerythrocytosis was made,he was transferred to the gastroenterology department and was treated for his pancreatitis according to guidelines for diagnosis and treatment of chronic pancreatitis(Nanjing,2018).
OUTCOME AND FOLLOW-UP
This patient was treated in the gastroenterology department for his pancreatitis,and the serum level of TGs,TC,and LDL gradually decreased.Along with the decreasing serum level of TGs,TC,and LDL,the results of CBC examination were normalized with the exception of a mild anemia.
DISCUSSION
MPNs,including chronic myelogenous leukemia,8P11 myeloproliferative syndrome,chronic eosinophilic leukemia,polycythemia vera(PV),essential thrombocythemia,primary myelofibrosis,chronic neutrophilic leukemia,systemic mastocytosis,and chronic basophilic leukemia,are clonal diseases resulting from the uncontrolled proliferation of hematopoietic stem and progenitor cells without obvious differential arrest and dysplasia,leading to the hypercellular BM and the increased periphery blood(PB)cell counts.Diagnosis and classification of MPNs are primarily based on the morphological examination of the BM and PB cells.These seemingly normalappearance blood cells are caused by gain of function reciprocal translocations and mutations in genes encoding receptor tyrosine kinases or their c-Jun N-terminal kinase-signal transducer and activator of transcription(JNK-STAT)-associated signal pathway components.Constitutive activation of the JNK-STAT signaling pathway is responsible for excessive and autonomous blood cell production[1-3].MPN-associated fusion genes caused by the recurrent rearrangements frequently involved the genes ABL1,platelet-derived growth factor receptor-α(PDGFR-α),PDGFR-β,and fibroblast growth factor receptor-1,whereas MPN-associated gene mutations frequently involved the genes JAK2,CALR,MPL,CSF3R,and the stem cell growth factor receptor gene CD117[1-7].
In this paper,we described a pancreatitis patient who was at first misdiagnosed as erythrocytosis(presumptive diagnosis of PV)because of the markedly elevated Hb level at presentation due to the mistaken readings of the ABCC in the evaluation of complete blood cells,but he was eventually diagnosed with SHLE-induced pseudoerythrocytosis.The purpose of reporting this patient and the diagnostic process is for the doctors to call attention to the comprehensive and objective evaluation of theCBC results on ABCC,especially in the setting of SHLE,a very common laboratory finding in clinical practice.
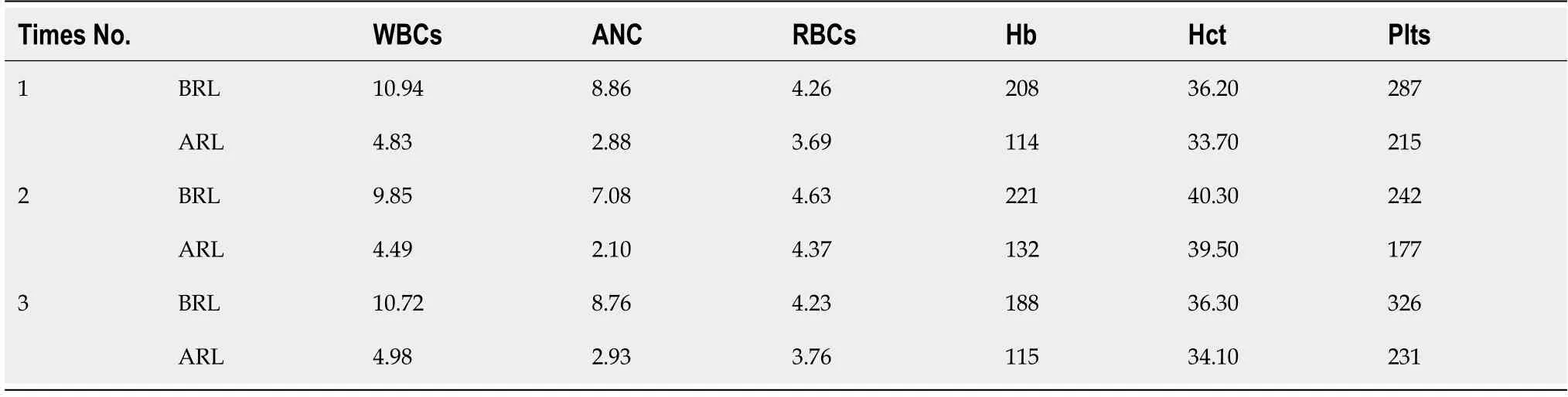
Table 1 Complete blood count results before and after removing the chylomicron layer
The World Health Organization diagnostic criteria for PV is based on the elevated Hb(>16.5 g/dL in men or >16.0 g/dL in women)or Hct(>49% in men or >48% in women)levels,with the prominent erythroid,granulocytic and megakaryocytic proliferation in BM biopsy,incorporating the presence of JAK2V617F or JAK2 exon 12 mutation[2,3].In clinical practice,the elevated Hb level is the most commonly used parameter for the diagnosis and grading of anemia and erythrocytosis.In this patient,the markedly elevated Hb level at presentation(up to 225 g/L = 22.5 g/dL)strongly indicated the possibility of the presence of PV.However,the following laboratory investigations,including morphological examination,cytogenetic and molecular analysis,did not meet criteria for the diagnosis of any kind of MPN.
The CBC profile in this patient revealed a noteworthy feature:WBCs,ANCs,Hb,MCH,and MCHC were all increased to some degree,with the presence of markedly elevated Hb and MCHC level,but the absence of a paralleled increase in RBCs and Hct was the most prominent feature.The dramatically fluctuating and obviously discrepant CBC results among Hct,RBCs,Hb,MCV,MCH,and MCHC were easily identified.In addition,there was a conspicuous chylomicron layer floating on the surface of the blood samples.Having noticed these,we removed a large part of the chylomicron layer and then evaluated the CBC readings.After removing a large part of the chylomicron layer,WBCs,ANC,Hb,MCH,MCHC,and Plt were all decreased to varying degrees.We presumed that the erythrocytosis was the result of fatty droplets that are mistakenly identified as blood cells due to the limited parameters of ABCC.So a laboratory investigation was performed by drawing dual blood samples,measuring them(the chylomicron layer was removed in one sample and was not in another)at the same time,and comparing the CBC results.As we expected,there was a significant difference in the CBC results.This laboratory investigation provided strong evidence to conform the contribution of SHLE to the markedly elevated Hb and MCHC levels in CBC examination in this patient.
Hyperlipemia,one of the essential compartments of metabolic syndrome,combination of genetic background and environmental factors in its pathogenesis,is a common laboratory finding in biochemical tests.SHLE could be the complication of various diseases mainly involving diseases in the cardiovascular system,endocrine system,liver,pancreas and kidneys,in which hyperlipemia may the consequence of metabolic abnormalities and play an essential role in the pathogenesis of targeted tissue damages[8-21].In the genetically predisposed individuals,systemic inflammatory conditions and dietary regimen may be the major environmental factors to influence the lipid metabolism and insulin resistance[22-27].SHLE sometimes occurs in the natural history or in the treatment of certain hematological diseases,such as in tyrosine kinase inhibitor treatment for patients with MPNs,retinoic acid treatment for patients with acute promyelocytic leukemia and L-asparaginase treatment for patients with acute lymphoblastic leukemia[28-32].It is well known that SHLE have an unexpected impact on many kinds of laboratory tests,making the diagnostic process more complicated and perplexed.SHLE may also affect the CBC results on the ABCC.
To date,there are too few reports that have documented the erythrocytosis to be complicated by hyperlipemia in that erythrocytosis was in association with the high frequency of cardiovascular events and the incitation of pancreatitis[33-38].However,it has never been recognized that SHLE can lead to the induction of pseudoerythrocytosis.The higher frequency of erythrocytosis in the context of SHLE strongly indicates that some patients may be misdiagnosed as MPNs due to mistaken readings by the ABCCs[38]as reported in the present case.The high frequency of cardiovascular events and the induction of pancreatitis in this setting may lie in the hyperlipemia-related diseases themselves which may result from the dysregulated metabolic activities and the co-existing inflammatory conditions[21-27].
The impact of SHLE on the CBC results may be overlooked because hyperlipemia patients seldom see the hematologists,and thus,this phenomenon has not been rigorously investigated.Differential diagnosis between true erythrocytosis and pseudoerythrocytosis in the setting of hyperlipemia may be simply by intellectual and comprehensive analysis of the reasonableness of each CBC results(especially by the observation whether the Hb level is in parallel to the Hct value or not)at first and by comparing the CBC results between blood samples with and without removal of the chylomicron layer subsequently by a means employed in this paper.In addition,the elevated even normal serum levels of total,LDL and high density lipoprotein cholesterol are biased to the diagnosis of hyperlipemia-induced pseudoerythrocytosis or have an co-existence of MPNs and hyperlipemia-related diseases[39-42].However,this investigation is limited by the changes in the value of blood sample,and these changes may make it difficult to interpret the true Hb concentration in patient’s blood.Another question is what concentration and components of blood lipids are able to significantly affect the CBC readings on the ABCC.So,this investigation merely provides an information that SHLE could affect the CBC results measured by ABCC,and how to correctly measure the true Hb concentration in patient’s blood warrants further investigations.
Recognizing this phenomenon helps better understand the CBC results on ABCC in the context of hyperlipemia,especially in individuals with SHLE.MPNs are clonal diseases characterized by the constitutive activation of genes in growth factor receptors or their signal pathway components,resulting in the uncontrolled proliferation of hematopoietic cells.Treatment of MPNs differ completely from that of hyperlipemia-related diseases.Therefore,the differential diagnosis between these diseases is very important as demonstrated in this case.In addition,SHLE sometimes occurs in the treatment of hematological malignancies,and this may lead to the misinterpretation of transfusion indications,which may result in serious consequences such as severe ischemic episodes and severe bleeding events.
CONCLUSION
SHLE could significantly affect the CBC results on ABCC.This phenomenon may lead to the misdiagnosis of hyperlipemia-related diseases as MPNs and the resultant mistreatment.It may also lead to the misinterpretation of transfusion indications in the treatment of hematopoietic diseases.
When a patient presents with a high level of Hb and makes a presumptive diagnosis of MPNs,it is very necessary to carefully examine the blood samples,to correctly evaluate the CBC results and to look up the biochemical tests.The appearance of a chylomicron layer in blood samples,the discrepant results in CBC examination and the elevated serum levels of TGs,TC,and LDL strongly indicate the possible diagnosis of pseudoerythrocytosis.In this setting,investigations are warranted as showed in our paper,and the underlying diseases must be diagnosed as soon as possible so as to let the patient receive prompt and proper treatments.In patients with hematological diseases in the setting of hyperlipemia,the blood transfusion indications must be adjusted according to the patient’s symptoms rather than are dependent merely on the Hb levels or the Plt counts.
ACKNOWLEDGEMENTS
The authors would like to thank Bin Li(Department Gastroenterology,The Affiliated Hospital of Qingdao University),Xiu-Shuan Feng(Department Radiology,The Central Hospital of Qingdao West Coast New Area),and Ming Bai(Department Ultrasonography,The Central Hospital of Qingdao West Coast New Area)for assistance in the analysis of laboratory and imaging examination.
 World Journal of Clinical Cases2020年19期
World Journal of Clinical Cases2020年19期
- World Journal of Clinical Cases的其它文章
- Role of monoclonal antibody drugs in the treatment of COVID-19
- Review of simulation model for education of point-of-care ultrasound using easy-to-make tools
- Liver injury in COVID-19:A minireview
- Transanal minimally invasive surgery vs endoscopic mucosal resection for rectal benign tumors and rectal carcinoids:A retrospective analysis
- Impact of mTOR gene polymorphisms and gene-tea interaction on susceptibility to tuberculosis
- Establishment and validation of a nomogram to predict the risk of ovarian metastasis in gastric cancer:Based on a large cohort
