Oral granuloma in a pediatric patient with chronic graft-versus-host disease:A case report
Atsushi Uesugi,Fumihiko Tsushima,Takeshi Kuroshima,Jinkyo Sakurai,Hiroyuki Harada,Oral and Maxillofacial Surgery,Tokyo Medical and Dental University,Tokyo 113-8549,Japan
Makoto Kodama,Human Pathology,Tokyo Medical and Dental University,Tokyo 113-8510,Japan
Abstract BACKGROUND Oral mucositis is often observed with graft-versus-host disease (GVHD); however,the occurrence of oral granuloma is rare. The rapid increase in granulomatous lesions should be distinguished from malignant tumors in patients with GVHD because malignant diseases can develop in those patients. This case is the youngest pediatric patient with granuloma associated with GVHD.CASE SUMMARY The patient was a 1-year and 5-mo-old girl who presented to our department for the management of oral nodules. At the age of 5 mo,she was diagnosed with primary immunodeficiency disease,cord blood transplant was performed at 11 mo and bone marrow transplant at 1 year of age. After transplantation,GVHD and oral mucositis developed,and tacrolimus was administered. Interestingly,nodules appeared on the lower lip and buccal mucosa,which spontaneously disappeared. Then,a new nodule appeared on the left lateral border of the tongue. Resection was performed and the histopathological diagnosis was granuloma. The origin of these nodules were considered to be the fibroblasts activated under inflammation caused by GVHD because the calcineurin inhibitor tacrolimus acted on their proliferation.CONCLUSION It is very important to distinguish oral granulomatous lesions from malignancies if GVHD is present at the base and if immunosuppressive agents and steroids are being administered.
Key Words: Oral granuloma; Graft-versus-host disease; Bone marrow transplantation;Primary immunodeficiency disease; Tacrolimus; Case report
INTRODUCTION
Although hematopoietic stem cell transplantation can be used to treat and prevent complications caused by primary immunodeficiency disease (PID),graft-versus-host disease (GVHD) can complicate recovery. Oral lesions are frequently observed in association with GVHD,typical findings include lichen planus-like mucosal changes,damage to the salivary glands,and trismus due to sclerosis. However,the occurrence of oral granuloma with GVHD is rare. Here,we report the case of a pediatric patient who developed GVHD after bone marrow transplantation (BMT) for PID and subsequently developed granuloma in the oral mucosa.
CASE PRESENTATION
Chief complaints
A 1-year and 5-moh-old girl presented to our department for the management of oral nodules.
History of present illness
At 5 mo of age,the patient was diagnosed with PID upon sustaining a severe respiratory syncytial virus infection. At 11 mo of age,she received umbilical cord blood transplant but developed hemophagocytic syndrome,and the transplant failed to engraft. At 1 year of age,BMT was performed using the bone marrow from her HLA semi-matched father.In preparation for receiving BMT,she received fludarabine(× 3 d),melphalan (× 1 d),anti-thymocyte globulin (× 2 d),and etoposide (× 2 d beginning at 3 d prior to the scheduled procedure). In an effort to prevent GVHD,tacrolimus (FK506) was administered at 1 d prior to the procedure followed by methylprednisolone for 1 d and methotrexate for 4 d (on days 1,3,6,and 11) after BMT. Nonetheless,acute GVHD with oral mucositis developed on day 21; she was treated with additional FK506 and prednisolone. At 44 d after BMT,GVHD and oral mucositis had resolved somewhat. However,at day 64,a nodule transiently appeared in the lower lip mucosa; another nodule appeared in the buccal mucosa. The patient at 1 year and 5 mo of age was referred to our department for ongoing care.
Physical examination

Figure 1 Oral mucositis of the lip and buccal region. There were no findings suggesting lichen planus. A:A pedunculated nodule 8 mm × 5 mm in size and a sessile nodule 2 mm × 2 mm in size in the lower lip mucosa (arrow); B:The left buccal mucosa was grayish-white with a bleeding nodule (arrow).

Figure 2 One month after the first visit,all lesions spontaneously reduced. A and B:Oral nodules in the lower lip mucosa had disappeared 1 mo after the first visit.
On presentation,the patient had bleeding oral mucositis in the lip and buccal regions.There were no findings suggestive of lichen planus. Pedunculated nodules 8 mm × 5 mm in size and 2 mm × 2 mm in size were identified in the lower lip mucosa. The left buccal mucosa was grayish-white in color,with several easily bleeding nodules(Figure 1). The platelet count on this first visit was below the normal limits at 5 × 104/μL. However,1 mo after the first visit,all lesions spontaneously reduced (Figure 2).After 1 mo,GVHD recurred with oral mucositis. Her condition improved in response to elevated doses of both FK506 and prednisolone; however,GVHD-related gastrointestinal symptoms,mainly diarrhea and bloody stool,still persisted.Approximately 1 mo later,a nodule was detected on the left border of her tongue.Upon return to our department,an elastic soft,pedunculated nodule 12 mm × 10 mm in size was found on the left tongue border; this was diagnosed as a benign tumor(Figure 3). As her platelet count had sufficiently recovered (to 18.5 × 104/μL),the nodule was resected under general anesthesia. The procedure included 3-mm margins and excision into the muscle layer.
Pathological examination
The tumor pathology was notable for granulation tissue consisting of capillaries and fibroblasts accompanied by moderate infiltration with inflammatory cells,including neutrophils. No malignancy was reported nor were there any inclusion bodies suggestive of cytomegalovirus (CMV) infection (Figure 4). A deoxyribonucleic acid test to detect CMV was performed on the excised tissue,but the results were negative.
FINAL DIAGNOSIS
The final diagnosis of the presented case was granuloma of the tongue caused by calcineurin inhibitor used for the treatment of oral GVHD.
TREATMENT
After the excision,follow-up was performed without additional treatment.
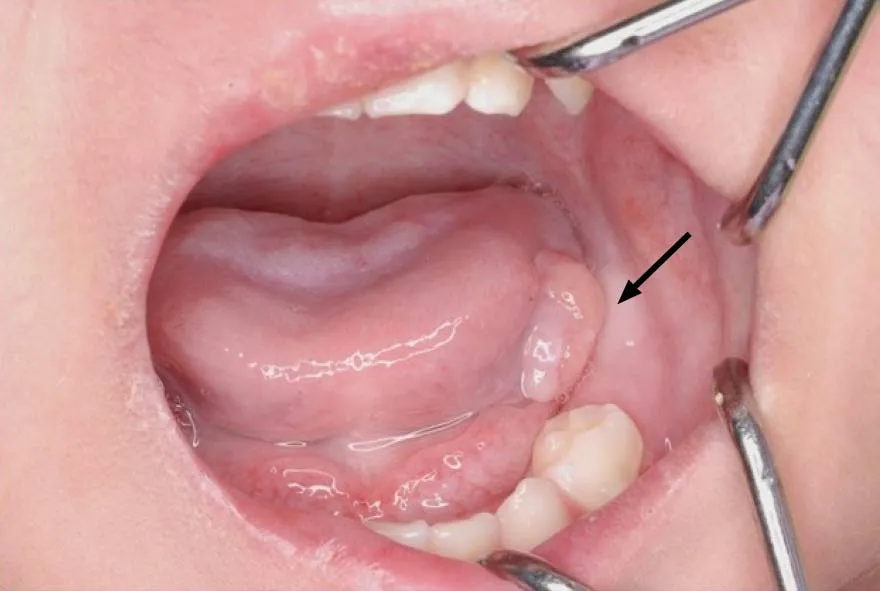
Figure 3 An elastic,soft,pedunculated nodule 12 mm in diameter was detected on the left tongue margin (arrow).
OUTCOME AND FOLLOW-UP
There was no recurrence of the lesion up to 1 year and 5 mo after the excision(Figure 5). However,the patient subsequently died due to an infection associated with PID.
DISCUSSION
GVHD associated with hematopoietic stem cell transplantation can be classified as acute or chronic. In this patient,GVHD developed 21 d after BMT and as such was diagnosed as acute GVHD. After several rounds of gastrointestinal symptoms,the diagnosis transitioned to chronic GVHD.
Typical oral lesions associated with GVHD include mucosal lichenoid changes,damage to the salivary glands,and trismus secondary to sclerosis[1]. In this patient,oral mucositis mainly comprised granulomatous nodules.
Wooet al[2]reported on non-gingival soft tissue granulomatous lesions in patients who developed GVHD after BMT. The features are as follows:(1) A non-gingival soft tissue nodule that exhibits rapid growth,raising malignancy concerns; (2) The presence of a certain degree of oral chronic GVHD in the tissues around the nodule;and (3) The presence of a certain degree of systemic GVHD,for which the patient was being treated with cyclosporin A (CsA)[2].
Among the explanations for these observations,when oral mucositis is caused by GVHD,the fibroblasts of the oral mucosa are activated,and lesions can result from the actions of CsA,which has a proliferative impact on fibroblasts[2,3].
In the present case,granulomatous nodules were detected in the non-gingival oral mucosa within a short time after the onset of GVHD. Initially,nodules were identified on the lower lip and left buccal mucosa; however,they spontaneously disappeared.Later,a nodule emerged at the left tongue border and was surgically removed. Prior to the appearance of these nodules,exacerbation of oral GVHD was observed.

Figure 5 We observed no recurrence of the lesion at 1 year and 5 mo after the procedure.
In this case,FK506 was administered in an attempt to prevent and later treat GVHD instead of CsA. FK506 is a calcineurin inhibitor with a similar mechanism of action as CsA. CsA promotes fibroblast proliferation and collagen and glycosaminoglycan synthesis and likewise suppresses their degradation,resulting in connective tissue growth[4].
To our knowledge,15 cases of transplant-related calcineurin inhibitor-induced oral inflammatory nodules with chronic and oral GVHD have been reported[5-7](Table 1).The age at transplant was between 11 mo and 50 years,and the present case was the youngest. There were 12 cases where CsA was used as a calcineurin inhibitor and 3 cases where FK506 was used.
On the other hand,Terasawaet al[8]reported the case of a patient with GVHD with a nodule on the lower lip associated with CMV infection. In this case,we examined the nodule that tested negative for CMV. However,it is possible that CMV was involved in generating the earlier lesions that spontaneously disappeared. In Table 1,only four cases,including our case,checked for CMV. Therefore,it is necessary to consider CMV infection when examining the presence of granulomatous nodules with GVHD.
Based on our findings,our conclusion is that the tongue granuloma reported in this patient is most likely the result of fibroblast activation during recovery from oral GVHD exacerbated by the proliferative actions of the calcineurin inhibitor FK506.
Patients with GVHD have a high risk of developing secondary tumors typically within 5 to 10 years following BMT[9]. Furthermore,immunosuppressive agents and steroids administered prophylactically are also risk factors of secondary cancers.Therefore,it is necessary to follow-up with patients who develop GVHD to detect any malignancies as early as possible.
CONCLUSION
We experienced a rare case of granuloma on the tongue of a pediatric patient with GVHD. The differential diseases include malignant tumor and CMV infection.However,these diseases do not have unique clinical features and can only be differentiatedviahistopathological examination and quantitative deoxyribonucleic acid testing of the diseased tissue. In particular,if GVHD is present at the base and if immunosuppressive agents and steroids are being administered,it is extremely important to distinguish it from malignant tumors.
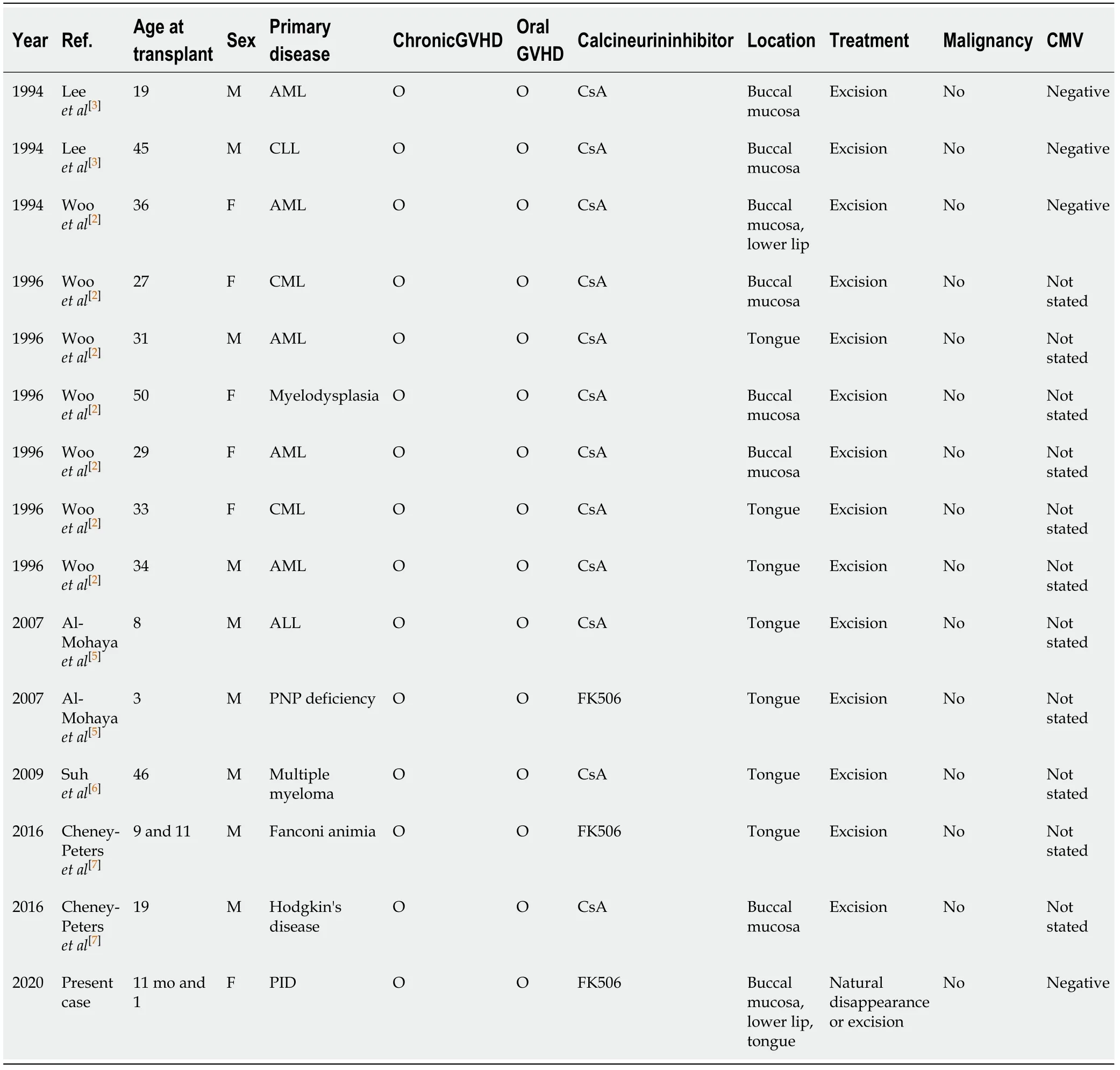
Table 1 Cases of transplant-related calcineurin inhibitor-induced oral inflammatory nodules with chronic and oral graft-versus-host disease
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Mari Tanaka from the Department of Pediatrics,Tokyo Medical and Dental University,for her kind of this case.
 World Journal of Clinical Cases2020年22期
World Journal of Clinical Cases2020年22期
- World Journal of Clinical Cases的其它文章
- COVID-19:A review of what radiologists need to know
- Holistic care model of time-sharing management for severe and critical COVID-19 patients
- Bioequivalence of two esomeprazole magnesium enteric-coated formulations in healthy Chinese subjects
- Osteoprotegerin,interleukin and hepatocyte growth factor for prediction of diabetes and hypertension in the third trimester of pregnancy
- High serum lactate dehydrogenase and dyspnea:Positive predictors of adverse outcome in critical COVID-19 patients in Yichang
- Risk factors analysis of prognosis of adult acute severe myocarditis
