Suspected SARS-CoV-2 infection with fever and coronary heart disease: A case report
Jin-Ru Gong, Jia-Sheng Yang, Yao-Wei He, Kang-Hui Yu, Jia Liu, Rui-Lin Sun
Jin-Ru Gong, Jia-Sheng Yang, Yao-Wei He, Jia Liu, Rui-Lin Sun, Department of Pulmonary and Critical Care Medicine, Guangdong Second Provincial General Hospital, Guangzhou 510317,Guangdong Province, China
Kang-Hui Yu, Department of Radiology, Guangdong Second Provincial General Hospital,Guangzhou 510317, Guangdong Province, China
Abstract BACKGROUND The coronavirus disease 2019 (COVID-19) is an emerging infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).Suspected cases accounted for a large proportion in the early stage of the COVID-19 outbreak. The deviation of the nucleic acid test by throat swab (the current gold standard of COVID-19) caused by variation in sampling techniques and reagent kits and coupled with nonspecific clinical manifestations make confirmation of the suspected cases difficult. Proper management of the suspected cases of COVID-19 is crucial for disease control.CASE SUMMARY A 65-year-old male presented with fever, lymphopenia, and chest computed tomography (CT) images similar to COVID-19 after percutaneous coronary intervention. The patient was diagnosed as having bacterial pneumonia with cardiogenic pulmonary edema instead of COVID-19. This was based on four negative results for throat swab detection of SARS-CoV-2 nucleic acid using reverse transcriptase-polymerase chain reaction assay and one negative result for serological antibody of SARS-CoV-2 with the serological assay. Additionally, the distribution of ground-glass opacities and thickened blood vessels from the CT images differed from COVID-19 features, which further supported the exclusion of COVID-19.CONCLUSION Distinguishing COVID-19 patients from those with bacterial pneumonia with cardiogenic pulmonary edema can be difficult. Therefore, it requires serious identification.
Key Words: COVID-19; Suspected case; Nucleic acid test; Serological antibody detection;Ground-glass opacities; Case report
INTRODUCTION
In December 2019, a novel coronavirus disease (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, Hubei Province, China[1]. It spread quickly to other provinces of China and overseas[2]. A total of 59804 confirmed cases, 1365 death, and 13435 suspected cases were reported in China by February 12, 2020[3]. A “suspected case” is defined as a patient with epidemiological history with any two clinical features [fever or respiratory symptoms,leukopenia or lymphopenia, chest imaging of patchy shadows or ground-glass opacities (GGO)] or having no epidemiological history but with the above three clinical manifestations[4]. However, these symptoms (like fever, cough,etc.) are not unique because they are found in many other infectious diseases.In addition,lymphopenia could be seen in patients with an impaired immune system. The deviation of the nucleic acid test by throat swab (the current gold standard of COVID-19) caused by variation in sampling techniques and reagent kits and coupled with nonspecific clinical manifestations make confirmation of the suspected cases difficult.Management of the suspected cases during the epidemic period prevents further spread and preserves healthcare resources. Here, we present the diagnosis and treatment of a suspected case of COVID-19 during the epidemic period.
CASE PRESENTATION
Chief complaints
A 65-year-old man was admitted to the cardiovascular internal medicine department with chest pain for 9 d. He presented with fever, cough, and chest tightness after percutaneous coronary intervention for 4 d.
History of present illness
Acute retrosternal pain occurred in the patient 9 d ago. An emergency percutaneous coronary intervention therapy was performed on the patient due to the abnormally elevated levels of troponin and ST-segment when presented at the cardiovascular internal medicine department that day. The patient had suffered a transient loss of consciousness due to ventricular fibrillation after percutaneous coronary intervention.Four days ago, the patient incurred fever, cough with white sticky sputum, and chest tightness. Moreover, the patient had a maximum body temperature of 38.2 °C and chest computed tomography (CT) images that were similar to COVID-19. The patient was therefore transferred to the infectious isolation ward with a possible diagnosis of COVID-19 on the 4thd of fever onset (Figure 1).
History of past illness
The patient’s medical history included hypertension, lacunar infarction, and history of aortic aneurysm surgery.
Personal and family history
He had no history of living in Wuhan, the epidemic area, or exposure to patients with COVID-19. Social history was negative for tobacco, alcohol, or substance abuse. No obvious family history.
Physical examination
The temperature was 37.5 °C, heart rate 80 bpm, respiratory rate 21 bpm, blood pressure 112/72 mmHg, and oxygen saturation was 96%. The patient had harsh breath sounds and scattered moist rales during auscultation of both lower lungs. We considered this to be either lung inflammation or heart failure. The cardiac and digestive portions did not show abnormalities.
Laboratory examinations
Blood analysis showed lymphopenia was 0.76 × 109/L, elevated neutrophils count: 6.8× 109/L (normal range < 6.4 × 109/L), normal white blood cell count, and normal hematocrit and platelet count. Routine stool and urine test results were normal.Biochemical assessment of the blood demonstrated normal liver and kidney function but increased levels of hypersensitive troponin I: 1.64 ng/mL (normal range < 0.12 ng/mL) and N-terminal pronatriuretic peptide: 2860 pg/mL (normal range < 125 pg/mL). There was an increase in C-reactive protein (CRP): 114.6 mg/L (normal range< 8 mg/L), procalcitonin (PCT): 0.26 ng/mL (normal range < 0.05 ng/mL), and Ddimers: 3.32 μg/mL (normal range < 0.5 μg/mL). CD3, CD4, and CD8 T-lymphocyte counts declined simultaneously. Two real-time reverse transcriptase-PCR results for the SARS-CoV-2 nucleic acid tests by throat swab were negative. Electrocardiogram revealed the acute anterior and inferior myocardial infarction. Two-dimensional transthoracic echocardiography revealed ultrasound changes of acute myocardial infarction, a cardiac ejection fraction of 35%, and mild pulmonary hypertension.
Imaging examinations
Initial imaging evaluation with chest X-ray on the day of fever onset showed increased lung markings with bilateral opacification mainly in the inner and middle belts of the lung, and the hilar shadow was enlarged and thickened (Figure 2A and 3A). On the 3rdd after fever onset, the chest CT scan confirmed multiple flaky ground-glass shadows in the right lung, left upper lung, and the left lower lung (Figure 4A1, B1, C1, and D1).Thickened blood vessels and fibrous stripes were seen in some lesions of the right lung. The diagnosis of COVID-19 could not be excluded based on these CT scan findings.
FINAL DIAGNOSIS
The final diagnosis of the presented case was bacterial pneumonia with cardiogenic pulmonary edema.
TREATMENT
Considering the CT findings, the lung lesion was primarily characterized as viral pneumonia. The patient was given 0.2 g three times daily oral Arbidol, an empiric oral antiviral therapy during in-hospital treatment. In addition, 2 g QD Ceftriaxone and 0.4 g QD Levofloxacin were prescribed due to increased PCT, CRP, and neutrophil counts.The patient received 20 mg twice daily oral furosemide and secondary prevention of coronary heart disease due to elevated NTproBNP and acute myocardial infarction.
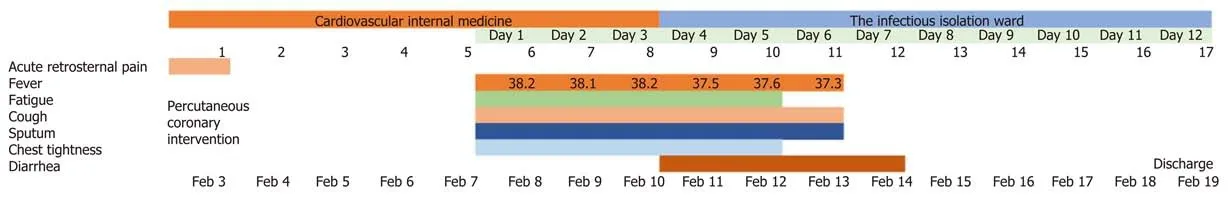
Figure 1 Symptoms and maximum body temperatures according to day of fever and day of hospitalization, February 3 to February 19,2020.
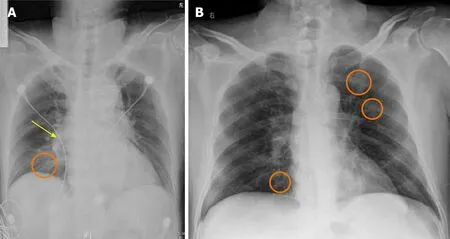
Figure 2 Orthotopic chest radiograph images of bacterial pneumonia with cardiogenic pulmonary edema and coronavirus disease 2019(a confirmed patient from our institution). A: Enhanced lung markings with opacification mainly in the inner and middle belts of the right lung (orange circle)and enlarged and thickened hilar shadow (yellow arrow); B: Multiple bilateral areas (orange circles) of patchy shadows with normal lung hilum.
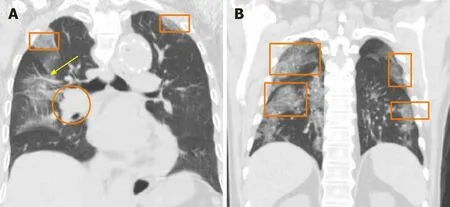
Figure 3 Orthotopic chest radiograph images of bacterial pneumonia with cardiogenic pulmonary edema and coronavirus disease 2019.A: Enhanced lung markings with bilateral opacification (orange squares), ectatic blood vessel (yellow arrow), and an enlarged and thickened hilar shadow (orange circle); B: Multiple bilateral areas (orange squares) of patchy shadows mainly located in the lateral field with normal lung hilum.
OUTCOME AND FOLLOW-UP
After 7 d of treatment, the patient’s symptoms improved significantly. He recovered from the fever, and the chest tightness and cough were relieved. Further, reexaminations of CT on the 7thd revealed a reduction in multiple ground-glass opacities in the right lung, left upper lung, and the left lower lung (Figure 4A2, B2, C2 and D2).The PCT was normal, and the CRP significantly decreased on the 7thd of illness. He was discharged on day 12 without obvious discomfort after the fever.
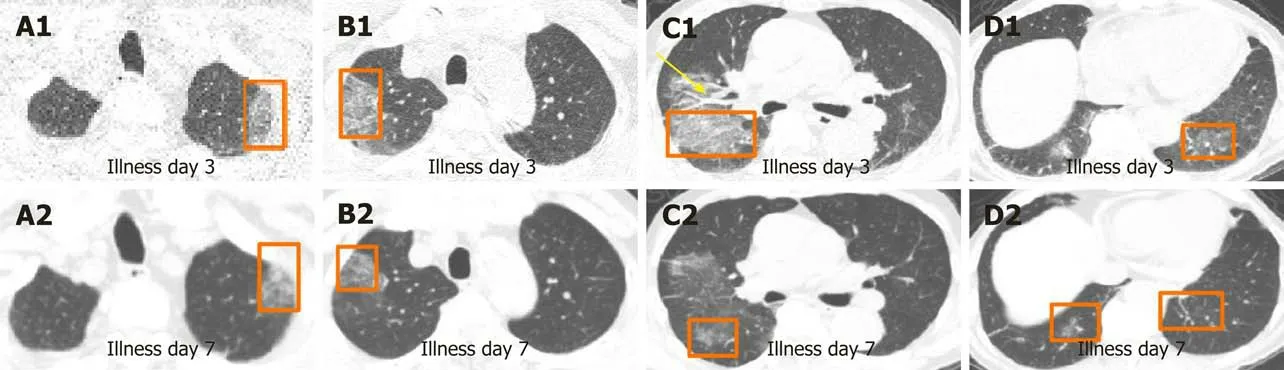
Figure 4 Unenhanced chest computed tomography images of bacterial pneumonia with cardiogenic pulmonary edema on day 3 after the onset of symptoms and day 7 after the onset of fever. A: Patchy ground-glass opacities in left upper lung (A1), ground-glass nodule in left upper lung (A2);B: Crazy-paving pattern in right upper lung (B1), ground-glass opacities in right lung (B2); C: Crazy-paving pattern and consolidation (orange square), ectatic blood vessel (yellow arrow) in right lung (C1), ground-glass opacities in right lung (C2); D: Ground-glass nodule in right lower lung, fibrous stripes in left lower lung (D1),ground-glass nodule in right lower lung, fibrous stripes in left lower lung (D2).
DISCUSSION
COVID-19 is an acute infectious pneumonia caused by a new strain of coronavirus that has not previously been identified in humans until late December 2019[5]. Evidence shows that human-to-human transmission has occurred through contact and droplets[4,6,7]. The natural and intermediate host of the SARS-CoV-2 may be horseshoe bat[8]and pangolin[9], respectively. The SARS-CoV-2 belongs to a cluster of betacoronaviruses, and it shares 76.4% genome sequence homology to SARS-CoV[10].The SARS-CoV-2 binds to the angiotensin-converting enzyme 2 (ACE2), a similar receptor to SARS-CoV[10], to infect the host. However, the affinity of ACE2 binding to SARS-CoV-2 is 10 to 20 fold than that of SARS-CoV[11]. The basic reproduction number of SARS-CoV-2 was higher than that of SARS-CoV[12,13], which meant stronger human transmission than SARS. Fever, fatigue, dry cough, expectoration, poor appetite, and myalgia were the common symptoms of COVID-19, whereas dizziness, vomiting,abdominal pain, diarrhea, rhinobyon, and conjunctival congestion were rare conditions of the disease[14,15]. Most COVID-19 patients have leukopenia and lymphopenia and elevated CRP but normal PCT[4]. About 86.4% of these patients have abnormal chest CT images. About 85.4% of COVID-19 cases are mild[16], but some progress rapidly and cause multiple organ failure. Additionally, the overall mortality rate of COVID-19 is 1.4%, where the mortality rate for ICU patients ranges from 5% to 61.5%[15,17].
The 65-year-old male, who had no epidemiologic history, but had fever, cough,lymphopenia, and CT images of multiple patchy GGOs, was a suspected case of COVID-19 according to the Diagnosis and Treatment of Pneumonia Caused by 2019-nCoV (version 5)[4]. The patient underwent a series of COVID-19 tests as recommended. Throat swab tests for the SARS-CoV-2 nucleic acid test were performed four times using the real time reverse transcriptase-PCR assay, and the results were negative. Based on the Chinese standards of Pneumonia Caused by 2019-nCoV, the patient could have been discharged from the hospital[4], but he was hospitalized for 1 wk at the cardiovascular internal medicine department before admission to the isolation ward. A misdiagnosis of COVID-19 can result in serious adverse consequences, such as cross infection among patients and healthcare workers.Additionally, several studies have found as high as 20% false-negative rates of the COVID-19 real time reverse transcriptase-PCR test[18-20]. Other detection methods were therefore recommended.
Another study suggested that on day 5 of the onset, the immunoglobulin (Ig) G and IgM of SARS-CoV-2 could be detected in the blood of almost all patients, while the detection rate of SARS-CoV-2 nucleic acid in throat swabs was only in 25% of the patients[21]. We collected blood samples of our patient to detect the IgM and IgG of SARS-CoV-2 on day 8 of onset, and the results were negative. We thus excluded the diagnosis of the novel coronavirus pneumonia in terms of etiology. Besides, the patient was an elderly man with underlying cardiovascular diseases such as acute myocardial infarction, cardiac insufficiency, and hypertension. According to the early warning model for predicting mortality in viral pneumonia (MuLBSTA score, which contains six indexes, including multiple infiltrations, lymphocytopenia, bacterial coinfection,smoking history, hypertension, and age[22]), our patient was at a high risk of death.Some studies have confirmed that COVID-19 cases in older patients with underlying comorbidities, including cardiovascular or cerebrovascular disease, have a higher rate of becoming critically ill or dying[5,14,17]. However, after antibacterial strategy, diuretic treatment, and secondary prevention of coronary heart disease, there was a significant improvement in fever, cough, and chest tightness on day 7. Therefore, the 65-year-old male patient was excluded from COVID-19 diagnosis based on the disease progression.
Chest CT scan is valuable and helpful in the diagnosis of COVID-19, and its diagnostic sensitivity was 97% in the epidemic area. A study involving 63 patients suggested that the imaging characteristics of COVID-19 included GGO (85.7%),ground-glass nodules (22.2%), patchy consolidation (19%), fibrous stripe (17.5%), and irregular solid nodules (12.7%)[23]. The predominant CT feature of COVID-19 was GGO, which was gradually followed by crazy-paving pattern and consolidation. In the first 2 wk, the lesions were increased and consolidated. After 2 wk, the lesions were absorbed, leaving a wide range of GGO and subpleural consolidation shadow[24]. The CT images of our 65-year-old suspected case of COVID-19 showed that there were multiple patchy GGOs, ground-glass nodules, crazy-paving pattern, and consolidation in bilateral lungs, which were typical features of COVID-19. However, the GGO of this patient, which was confirmed to be associated with cardiogenic pulmonary edema,was mainly in the parahilar regions and gravitational distribution. The lesions of COVID-19 are mainly distributed in the subpleural area (Figure 2B and 3B) because the SARS-CoV-2 mainly attacks type II alveolar epithelial cell[25].
In addition, the patient’s CT images were characterized by thickened pulmonary vascular shadows, the typical feature of cardiogenic pulmonary edema. In patients with cardiogenic pulmonary edema, the increase of pulmonary vascular pressure,caused by cardiac insufficiency, triggers the pulmonary capillary fluid exuding into the pulmonary interstitium. However, the pulmonary edema of the novel coronavirus pneumonia is due to the disruption of the alveolar-capillary barrier with protein-rich fluid entering the interstitial spaces and alveolar cavities[26,27]. The mechanism that protein-rich edema cannot transfer to the central area might explain why the noncardiogenic edema lacks bronchial vascular bundle thickening[28]. In the patient, the lung lesions were significantly absorbed, the density was reduced, and the thickened pulmonary vascular shadows disappeared on day 7 after the onset of symptoms using the diuretic treatment. The lack of further enlarged and consolidated lesions disqualified the radiographic features of novel coronavirus pneumonia. Although the CT imaging of our suspected case could be easily confused with that of the coronavirus pneumonia, it can be further disqualified based on the distribution area of the lung lesions, the presence of vascular thickening, and the evolution of the COVID-19-related CT images (Figure 5).
This case report can provide a certain reference for the differential diagnosis of COVID-19 in the early stage and reduce panic to a certain extent. But the defect is that more cases need to be verified.
CONCLUSION
Distinguishing COVID-19 patients from those with bacterial pneumonia with cardiogenic pulmonary edema can be difficult and therefore requires serious identification. Further, serological antibody detection of SARS-CoV-2 coupled with chest CT scans can improve the differential diagnosis of COVID-19.
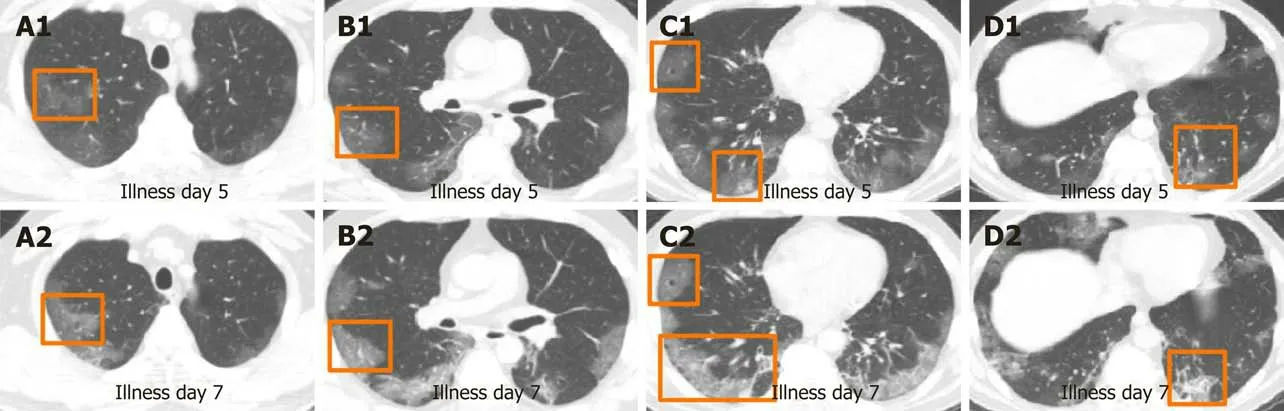
Figure 5 Unenhanced chest computed tomography images of coronavirus disease 2019 on day 5 after the onset of symptoms and on day 7 after the onset of symptoms. A: Subpleural ground-glass opacities in right upper lung (A1), subpleural ground-glass opacities in right upper lung (A2); B:Subpleural ground-glass opacities in right middle lobe (B1), segmental ground-glass opacities in right middle lobe (B2); C: Air bronchogram in right middle lobe,subpleural ground-glass nodule with halo sign in right lower lung (C1), air bronchogram right middle lobe, Crazy-paving pattern and consolidation in right lower lobe(C2); D: Subpleural ground-glass nodule and fibrous stripes in left lower lung (D1), consolidation change in left lower lung (D2).
ACKNOWLEDGEMENTS
We acknowledge the contribution of Yu KH to radiologic interpretation.
 World Journal of Clinical Cases2020年23期
World Journal of Clinical Cases2020年23期
- World Journal of Clinical Cases的其它文章
- Understanding the immunopathogenesis of COVID-19: Its implication for therapeutic strategy
- What is the gut feeling telling us about physical activity in colorectal carcinogenesis?
- Latest developments in chronic intestinal pseudo-obstruction
- Correlation between ductus venosus spectrum and right ventricular diastolic function in isolated single-umbilical-artery foetus and normal foetus in third trimester
- Clinical efficacy of integral theory–guided laparoscopic integral pelvic floor/ligament repair in the treatment of internal rectal prolapse in females
- Treatment of Kümmell’s disease with sequential infusion of bone cement: A retrospective study
