Clinical observation of sinew-regulating bone-setting manipulations plus exercise therapy for chronic non-specific low back pain
Yao Meng-li (姚梦莉), Chen Zhao-hui (陈朝晖), Zhang Wen-di (张文娣), Xu Han (徐寒), Wang Ting-ting (王婷婷),Hu Rong-ting (胡荣庭)
1 Graduate School, Anhui University of Chinese Medicine, Hefei 230038, China
2 College of Acupuncture-moxibustion and Tuina, Anhui University of Chinese Medicine, Hefei 230038, China
Abstract
Keywords: Bone Setting and Tuina; Bone Setting Manipulation; Massage; Exercise Therapy; Low Back Pain; Visual Analog Scale; Pain Measurement; Electromyography
Non-specific low back pain (NLBP) refers to a series of symptoms mainly including pain and discomfort in the lumbosacral region, with or without lower-limb symptoms.It is termed chronic NLBP (CNLBP) when the duration is over 3 months[1].Epidemiological study showed that 60%-80% of adults experienced low back pain, and NLBP accounted for 85%, significantly affecting people’s quality of life[2-3].Currently,conservative treatment is usually applied for CNLBP.Study showed that comprehensive rehabilitation training produced more significant efficacy[4].We have used sinew-regulating bone-setting manipulations plus exercise therapy to treat CNLBP since 2018 following our supervisor.The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria of this study were developed by referring to theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[5]andSinew Injury Science of Traditional Chinese Medicine[6]: a history of chronic strain or recurrent low back pain; tenderness in one side or both sides of the low back, sacroiliac region or buttocks,nodules may be palpated, without positive signs of nervous system, with or without lower-limb symptoms;limited range of motion of the low back, symptoms could be aggravated by bending over or fatigue but curbed after rest; X-ray examination could show abnormal changes such as lumbar vertebral hyperosteogeny and loss of physical curve, and specific or nerve root pathological changes were excluded by CT or MRI examination.
1.2 Syndrome differentiation criteria of traditional Chinese medicine (TCM)
The TCM syndrome differentiation criteria were made based on theGuiding Principles for Clinical Study of New Chinese Medicines[7]andClinical Terminology of Traditional Chinese Medical Diagnosis and Treatment[8].
Main symptoms: Dull pain in low back, limited motor function, released by hot application.White watery tongue coating, dark purple tongue body which may present ecchymosis, sinking and slow or stagnant pulse.
Secondary symptoms: Flaccid or aching low back and knees.
The pattern of stagnation due to cold and damp could be diagnosed when there presented the main symptoms with or without secondary symptoms.
1.3 Inclusion criteria
Conformed to the diagnostic criteria and the TCM syndrome differentiation criteria; aged between 20 and 55 years old; disease duration ≥3 months; signed the informed consent form.
1.4 Exclusion criteria
A history of back surgery or thoracolumbar spine fracture; low back pain caused by other problems,including lumbar spine fracture, lumbar intervertebral disc herniation, lumbar spinal stenosis, lumbar spondylolisthesis, scoliosis, etc.; severe osteoporosis,lumbar tuberculosis or intraspinal tumor; blood system diseases; serious primary diseases of cardiocerebrovascular system, liver, kidney, etc.; mental diseases; infectious skin diseases or skin damage in the region to-be-treated; pregnant or lactating women;spinal damage or spinal cord injury with unclear diagnosis; patients undergoing other treatments.
1.5 Dropout criteria
Patients with poor compliance or adding other treatments without approval; lost to revisit or quit on one’s own, including those responding well to treatment but failed to complete the whole study;severe adverse reactions or events that interrupted the treatment; medical history was not fully told at recruitment or sudden attack of other diseases during the study.
1.6 Statistical methods
The SPSS 23.0 software was used for data analyses.Measurement data meeting normal distribution and homogeneous of variance were expressed as mean ±standard deviation (±s) and processed byt-test.Measurement data not meeting normal distribution or homogeneity of variance and ranked data were analyzed using non-parametric test.Enumeration data were analyzed by Chi-square test.Atα=0.05,P<0.05 indicated statistical significance.
1.7 General data
A total of 65 CNLBP patients were recruited from the Sinew Injury Outpatient of the First Affiliated Hospital and Guoyitang Clinic of Anhui University of Chinese Medicine between January 2018 and May 2019.The 65 patients were divided into 2 groups by the random number table method, with 33 cases in the treatment group and 32 cases in the control group.The two groups each had 2 dropouts during the study.There were no significant differences in the general data between the two groups (P>0.05), suggesting the comparability (Table 1).The clinical study process is shown in Figure 1.
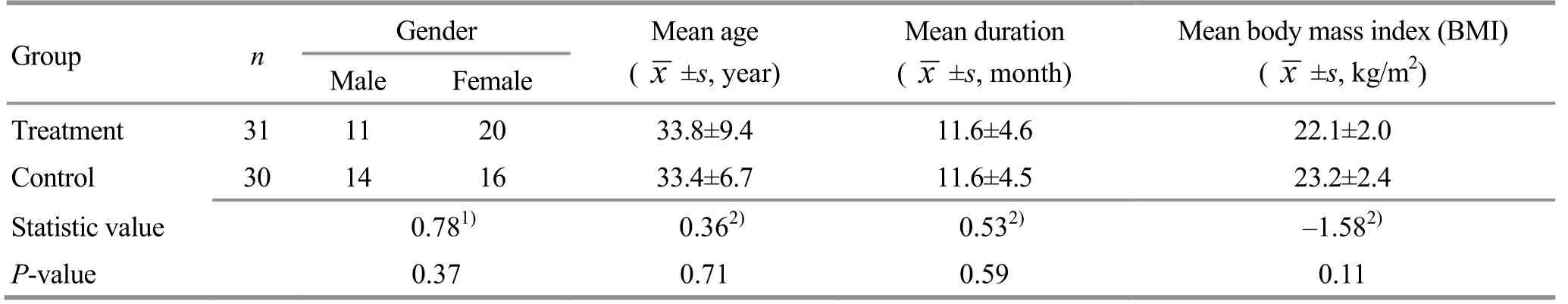
Table 1.Comparison of the general data

Figure 1.Clinical flow chart
2 Methods
2.1 Treatment group
2.1.1 Sinew-regulating bone-setting manipulations[9]
Sinew-regulating manipulations: With the patient taking a prone position, the physician first applied Gun-rolling, Dian-digital pressing and Rou-kneading manipulations to relax the back muscles (Figures 2-Figure 4).Then, Dian-digital pressing and Rouniankneading and twisting were applied to nodules in the low back and legs (painful nodules in paravertebral muscles, gluteus maximus, gluteus medius, gluteus minimus, and iliotibial tract, etc.).Afterwards, patient took a supine position with hips and knees bent.The physician then used Rou-kneading and Bo-plucking manipulations to relax psoas muscle of the affected side(Figure 5).Then, tender points were searched along the muscle regions of Foot Taiyang, Foot Shaoyang and Foot Shaoyin meridians (the medial and lateral sides of thighs and the posterior side of calf), and were relaxed and unblocked.The sinew-regulating manipulations lasted for 10-15 min and should be performed gently with moderate force.
Bone-setting manipulations: When patient lied on the lateral side, the physician applied oblique Ban-pulling manipulation, i.e.when the patient lied on the healthy side with the hip and knee of this side straight on the bed, and the hip and knee of the affected side bent, the physician stood facing to the patient, with one hand placing on the patient’s shoulder and the other hand on his buttocks, pushing the patient’s upper body and buttocks till the maximum range in opposite directions, and then the physician exerted a sudden opposing force.Click sounds usually could be heard (Figure 6).Afterwards, the patient turned to the other side, i.e.the healthy side on the top,and the Ban-pulling manipulation was performed again.The oblique Ban-pulling of low back can relax and unblock the adhesion of soft tissues, release spasm and cease pain, and correct the facet joint disorders.
Finishing manipulation: Gun-rolling and Sandispersing manipulations were applied to relax the low back, lasting for 2-3 min (Figure 1 and Figure 7).

Figure 2.Gun-rolling manipulation

Figure 3.Dian-digital pressing manipulation

Figure 4.Palm Rou-kneading manipulation

Figure 5.Finger Rou-kneading manipulation

Figure 6.Oblique Ban-pulling manipulation in lateral position

Figure 7.San-dispersing manipulation
The manipulation therapy was conducted once every other day with 7 sessions as 1 treatment course for a total of 1 course.
2.1.2 Exercise therapy
The exercise therapy regimen was developed by referring to the relevant references[10].
First, lumbodorsal muscle strength training.Flying swallow: patient took a prone position, with one hand grasping the wrist of the other side over the lumbosacral region.Taking the lumbodorsal muscles as the support, patient lifted the lower limbs and upper body simultaneously till the maximum range, with the chin drawn in and the nape and the rest part of the spine aligned, to open the chest and adduct the scapulae (Figure 8).To avoid holding the breath, patient was taught to count aloud to 10 s and then slowly go back to the original position.The upper body should lift starting from the low back, then chest and neck while dropping down starting from the neck, then chest and low back.Bilateral bridge: patient took a supine position with hands across in front of the chest and hips and knees bent.Patient then lifted the abdomen and stretched the hips till the maximum range, and then went back to the original position after maintaining for 10 s (Figure 9).Unilateral bridge: patient took a supine position with hands across in front of the chest and one knee bent (usually starting from the affected side).Taking the back and neck as the support, patient lifted the abdomen and stretched the other side of lower limb, lasting for 10 s.Patient could bend the elbows apposing to the bed for keeping stability, but the attention should be laid more on the low back and hips.Two legs performed this movement alternately(Figure 10).

Figure 8.Swallow flying pose

Figure 9.Bilateral bridge

Figure 10.Unilateral bridge
Second, abdominal muscle training.Straight leg raising: in a supine position, with two hands across over the abdomen, the patient held the legs straight together and lifted them up till 60-70°.Patient was told to count aloud till 10 s and then drop down the legs.Patient should repeat the movement after a 3-5 s interval (Figure 11).For patients with excessive lumbar curvature, the above exercises might cause lumbosacral pain.In this case, patients could put a thin cushion or a folded towel under the low back.

Figure 11.Straight leg raising
Third, strength training of the lateral trunk.Lateral bridge: patient lied on one side, with the elbow bent and supporting on the bed and in one line with the shoulder joint.Shoulders were not allowed to shrug.Taking the elbow and the lower foot as the support,patient lifted the buttocks till the maximum range and went back to the original position after keeping for 10 s(Figure 12).

Figure 12.Lateral bridge
During the exercises, the physician should always remind patients to count aloud for avoiding holding the breath.Otherwise, palpitations and chest tightness might happen.The training load should be tailored according to patient’s own condition and they should not feel tired the next day after exercises.The above exercises were performed with 10 times as 1 set, 3 sets a day, and 7 d as 1 course of treatment.The therapeutic efficacy was evaluated after 2 courses.
2.2 Control group
2.2.1 Exercise therapy
The exercise therapy was same as that for the treatment group.
2.2.2 Median-frequency electrotherapy
Ecm99-IIA medium-frequency electrotherapy apparatus (Beijing Yujian Rehabilitation Medical Appliances Co., Ltd., China) was adopted for electrotherapy.After topical sterilization with 75%alcohol, four electrodes (two groups) were applied to the lumbosacral or lumbodorsal region crosswise.The current intensity should be within the patients’endurance.The treatment was conducted once a day,20 min each session and 14 sessions as 1 course of treatment, for a total of 1 course.
3 Observation of Therapeutic Efficacy
3.1 Observation items
3.1.1 Pain intensity score
The two groups were measured by visual analog scale(VAS)[11]before and after treatment for pain intensity.A 10-centimeter-long black line was drawn on a piece of paper, with the two ends marked no pain (0) and extreme pain (10).Patients were told to select a point on the line to indicate their pain level.The VAS score was the distance between 0 and this point.
3.1.2 Detection of lumbar muscle endurance[12]
Static muscle endurance measurement: The patient took a prone position with two legs together and hands under the head.Taking the anterior superior iliac spine as the boundary, the upper body suspended out of bed while the lower limbs were fixed.During measurement,patients were told to lift the upper body as possible as they can.It’s the best that the shoulders, iliac crest and lateral malleolus were at the same level.The maintaining time was recorded by a stopwatch.
Dynamic muscle endurance measurement: The patient took a prone position on a treatment bed (at a 30° angle downwards) with the legs fixed together and hands across in front of the chest.Taking the anterior superior iliac spine as the boundary, the low back exerted a force to lift the body till parallel to the ground and then back to the initial position.Patients should complete the task at 25 times/min until they were no longer able to perform this movement.The number of times of completing this movement was recorded.
3.1.3 Detection of surface electromyography(sEMG)[13]
Flex Comp Infiniti 10-channel sEMG apparatus(Thought Technology Ltd., Canada) and BioGraph Infiniti software were adopted to measure the sEMG.Biering-Sorensen testing (BST) was conducted to collect the sEMG values of erector spinae and multifidus at static isometric contraction once before and after treatment, with the median frequency (MF), which is closely associated with the muscle fatigue, as the evaluation parameter.The room temperature was controlled around 24 ℃ and humidity 70%-80% during the test[13].
3.1.4 Lumbar dysfunction measurement
Oswestry disability index (ODI) was used to estimate the lumbar function[11]from 10 sections: pain (pain intensity), activities of daily living (personal care, lifting,walking, sitting, standing and sleeping), social activities(social life and traveling), sex life.Each section was scored 0-5 points, 0 standing for no pain and 5 for intensive pain that work and living abilities were greatly affected.The highest score was 50 points (100%) and the lowest score was 0 point (0%).The higher the score,the worse the dysfunction.
3.2 Criteria of efficacy evaluation
The therapeutic efficacy was evaluated based on theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[5].
Recovered: Low back pain disappeared, and there were no problems standing up, squatting, bending or walking.
Improved: Low back pain was basically released, and lumbar function was substantially improved, though pain still occurred after fatigue.
Invalid: There were no improvements in symptoms and signs.
3.3 Results
3.3.1 Dropouts
Two patients in the treatment group quit on their own; in the control group, 1 patient withdrew halfway and 1 patient added other treatments without approval.Finally, 31 cases in the treatment group and 30 cases in the control group were enrolled for statistical analyses.
3.3.2 Comparison of therapeutic efficacy
After treatment, the total effective rate was 90.3% in the treatment group versus 66.7% in the control group,and the between-group difference was statistically significant (P<0.05), (Table 2).

Table 2.Comparison of the clinical efficacy (case)
3.3.3 Comparison of the VAS score
The VAS score dropped in both groups after treatment (bothP<0.05), and was lower in the treatment group than in the control group with statistical significance (P<0.05).The result suggested that the two treatment protocols both could reduce the pain intensity in CNLBP patients, while the treatment group produced more significant efficacy than the control group (Table 3).
Table 3.Comparison of the VAS score (±s, point)

Table 3.Comparison of the VAS score (±s, point)
Note: Compared with the same group before treatment, 1)P<0.05; compared with the control group after treatment, 2)P<0.05
Group n Pre-treatment Post-treatment Treatment 31 5.45±1.38 1.55±0.881)2)Control 30 5.40±1.30 2.33±1.151)
3.3.4 Comparison of the lumbar muscle endurance
The endurance time at static state and the number of times at dynamic state of lumbar muscle changed significantly after intervention in the two groups (allP<0.05), and the between-group differences were statistically significant (bothP<0.05).This result indicated that the lumbar muscle endurance was improved in both groups, and the improvement was more significant in the treatment group than in the control group (Table 4).
3.3.5 Comparison of the MF of sEMG
After treatment, the MF values of sEMG of the erector spinae and multifidus changed significantly in both groups (allP<0.05), and the between-group differences were statistically significant (P<0.05).The result demonstrated that the anti-fatigue ability of lumbar muscles increased in both groups, and the improvement was more significant in the treatment group than in the control group (Table 5).
Table 4.Comparison of the lumbar muscle endurance (±s)

Table 4.Comparison of the lumbar muscle endurance (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Static muscle endurance (s)Dynamic muscle endurance (number of times)Pre-treatment Post-treatment Pre-treatment Post-treatment Treatment 31 56.19±10.91 82.74±9.061)2)19.06±4.67 24.64±4.521)2)Control 30 59.63±9.36 76.40±11.681)18.43±3.32 22.16±4.081)
Table 5.Comparison of the MF of sEMG (±s, Hz)
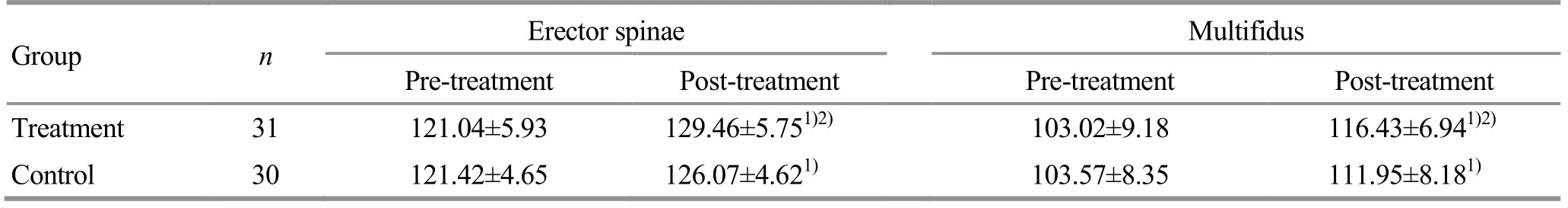
Table 5.Comparison of the MF of sEMG (±s, Hz)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Erector spinae Multifidus Pre-treatment Post-treatment Pre-treatment Post-treatment Treatment 31 121.04±5.93 129.46±5.751)2)103.02±9.18 116.43±6.941)2)Control 30 121.42±4.65 126.07±4.621)103.57±8.35 111.95±8.181)
3.3.6 Comparison of the ODI score
After treatment, the ODI score declined significantly in both groups (bothP<0.05), and was lower in the treatment group than in the control group (P<0.05).The result suggested that the lumbar function showed improvement in both groups and the improvement was more significant in the treatment group than in the control group (Table 6).
Table 6.Comparison of the ODI score (±s, %)

Table 6.Comparison of the ODI score (±s, %)
Note: Compared with the same group before treatment, 1)P<0.05; compared with the control group after treatment, 2)P<0.05
Group n Pre-treatment Post-treatment Treatment 31 34.67±9.94 17.42±4.541)2)Control 30 33.86±7.26 20.03±4.401)
4 Discussion
The development of CNLBP was closely related to the decreased lumbodorsal muscle endurance[14].In patients with low back pain, the coordination between motor muscles and stabilizing muscles declines, so that the normal motor pattern is broken.Several studies have found that patients with lower back pain have atrophic stabilizing muscles at the topical site, and the global motor muscles compensate to maintain the spinal stability, resulting in a higher synchronization and faster fatigue during movement[15-16].The motor muscles (consisting of erector spinae and rectus abdominis, etc.) belong to the superficial muscle group,usually covering more than two joints, with large cross-section, lots of muscle fibers, many motor units that can be activated, and stronger contractive force but shorter maintenance of contraction, leading to higher tendency of fatigue and pain.Besides, patients with low back pain usually tend to reduce workout because of pain, which will cause atrophy of the local muscles and decrease in muscle strength and endurance, thus forming a vicious circle and making the disease harder to cure.
By focusing on the above features of low back pain,this study adopted sinew-regulating bone-setting manipulations plus exercise therapy to treat CNLBP,using objective evaluation items for pain, muscle endurance and muscle fatigue degree to estimate therapeutic efficacy.The results demonstrated that sinew-regulating bone-setting manipulations plus exercise therapy produced more significant effects in increasing lumbar muscle endurance, reducing pain and improving lumbar function compared with medium-frequency electrotherapy plus exercise therapy.The possible reasons may involve the following three aspects.
First, Gun-rolling and Rou-kneading manipulations in sinew-regulating manipulations can promote blood and lymph circulation, increase metabolism, alter the ischemic and hypoxic even inflammatory conditions and release pain.Through stimulating the peripheral receptors, Dian-digital pressing manipulation can inhibit the transmission of nerve ending impulse signals and reduce pain.Ban-pulling manipulation can correct the facet joint disorders of vertebrae and restore the normal anatomical structure of spine by exerting an opposing force on the trunk and pelvis, activating blood circulation and repairing the soft tissue injuries.The final purpose of using these manipulations was to correct the position of bones, relax tendons and promote the circulation of qi and blood[17-18].
Second, the manipulations can effectively release muscle fatigue.Muscle fatigue may be related to the accumulation of lactic acid and other metabolites, and the imbalance of intracellular and extracellular Ca2+-K+concentration[19].By stimulating skin and force penetration, tuina manipulations can dilate blood vessels within a certain range, reduce local peripheral vascular resistance, increase blood flow, promote the metabolism of the accumulated products, balance Ca2+-K+concentration, and relieve muscle fatigue and pain.
Moreover, manipulations and exercise can complement each other.In treatment of chronic low back pain, exercise therapy produces outstanding effect in reducing the relapse of pain but its real-time and short-term effect in releasing symptoms is not significant.Tuina manipulations work well in making up for this weakness[20].During treatment, the peaceful and comfortable environment and gentle manipulations and kind words of the physician can help patients to relax, which also benefits the recovery of motor function.
In recent years, exercise therapy has gained much attention in treatment of low back pain and been commonly used for CNLBP[21].The exercises used in this study, swallow flying, bilateral bridge, and unilateral bridge, can not only reduce the long-term stretching strain of extensor dorsi and lumbosacral ligaments, but also stretch the tight fasciae of chest and abdomen.Lateral bridge and abdominal muscle exercise can adjust the lumbar muscles, increase the control and coordination of the body, restore the spinal stability and finally improve the lumbar function.We adopted a small-dose multi-set exercise plan, which can make muscles move in an isotonic-isometric contraction pattern (contracting-maintaining) to increase the lumbodorsal muscle strength and endurance.Repetitive and sustained exercise can stimulate the proprioceptive reflex, promote the central nervous system to regulate the core stabilizing muscles, avoid the compensation of the global motor muscles, and restore the correct movement pattern.
Although medium-frequency electrotherapy can improve blood circulation, promote the release of inflammation and swelling, regulate nerve activity and relieve pain, its action range is rather limited, with relatively same stimulation mode and amount[22], and the discomfort of electric stimulation may increase the tension of patients, which is not conducive to the full play of therapeutic efficacy and the improvement of symptoms.
The current study showed that sinew-regulating bone-setting manipulations plus exercise therapy produced more significant efficacy in improving pain,lumbar muscle endurance and fatigue, and lumbar function as well compared with medium-frequency electrotherapy plus exercise therapy.Thus, this method is worth promoting.
 Journal of Acupuncture and Tuina Science2020年1期
Journal of Acupuncture and Tuina Science2020年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Initiation mechanisms of acupuncture effect: a literature review of basic studies
- Manipulation parameter optimization in Liu’s back tuina therapy for kids’ cough variant asthma in remission stage
- Observation on therapeutic efficacy of tuina plus cupping for chronic fatigue syndrome
- Therapeutic efficacy and mechanism of heat-sensitive moxibustion for vascular dementia
- Clinical study on Jin’s three-needle therapy for post-stroke cognitive impairment
- Therapeutic efficacy and mechanism of heat-sensitive moxibustion for adjuvant treatment of depression in Parkinson disease
