Testosterone is a surrogate and proxy biomarker for severity of late-onset preeclampsia: A cross-sectional study
Thabat J. Al-Maiahy, Ali I. Al-Gareeb, Hayder M. Al-kuraishy
Department of Pharmacology, Toxicology and Medicine, College of Medicine Almustansiriya University, P.O. Box 14132 Baghdad, Iraq
ABSTRACT Objective: To find the association between testosterone serum levels and severity of late onset pre-eclampsia.Methods: This case-control study involved 34 patients with preeclampsia and 24 healthy control pregnant women matched for gestational and maternal age. The recruited pregnant women were divided into two groups: the pre-eclampsia group (34 pregnant women with pre-eclampsia) and the control group (24 healthy pregnant women). Lipid profile, blood urea, serum creatinine,proteinuria, total serum testosterone, sex hormone binding globulin and free androgen index were evaluated. Moreover, body mass index and blood pressure profile were measured.Results: There were high systolic and diastolic blood pressures in the pregnant women with late-onset pre-eclampsia when compared with healthy pregnant women (P<0.01). Total serum testosterone was higher in women with pre-eclampsia compared with healthy pregnant women (P=0.001). The free androgen index was higher in women with pre-eclampsia compared with healthy pregnant women (P=0.001). Sex hormone binding globulin level was low in women with pre-eclampsia compared with healthy pregnant women (P=0.001). High total serum testosterone was significantly correlated with all measured variables (P=0.001), except for body mass index and pulse pressure (both P=0.070). Smoking habit was low in those patients compared with healthy pregnant women.Meanwhile, total serum testosterone serum level was significantly correlated with number of cesarean sections (r=0.86, P<0.01) and nulliparty (r=0.56, P<0.01).Conclusions: Late onset pre-eclampsia in pregnant women is associated with high serum levels of total serum testosterone, free androgen index, low sex hormone binding globulin, low smoking habit with positive history for nulliparity and caesarean sections that are correlated with high blood pressure profiles. Therefore,high total serum testosterone which is correlated with most of risk factors of late-onset pre-eclampsia is regarded as a proxy biomarker reflecting the severity of late onset pre-eclampsia.
KEYWORDS: Pre-eclampsia; Testosterone; Free androgen index
1. Introduction
Pre-eclampsia is a serious pregnancy-related complication accounting for 4%-8% of all pregnancies which is linked with maternal and fetal mortality[1]. Pre-eclampsia is described by hypertension and proteinuria after 20 weeks of gestation, which,if developed before 34 weeks of gestation is called early-onset pre-eclampsia and when developed after 34 weeks of gestation is called late-onset pre-eclampsia. Both subtypes share interrelated and overlapped clinical features of different maternal and fetal outcomes. Maternal pre-eclampsia predisposes pregnant women for future metabolic and cardiovascular disorders due to pre-eclampsia induced-endothelial dysfunction and inflammatory changes[2].
The pathogenesis of pre-eclampsia is linked with trophoblastic neovascularization and placental dysfunction, which encourage lipid peroxidation and oxidative stress. Alongside, oxidative stress escorts vascular endothelial damage that aggravates vasospasm and systemic hypertension. In pre-eclampsia, there are disturbances in the invasion of cytotrophobalstic cells into uterine spiral arterioles leading to placental ischemia and hypoxia,which cause the release of different mediators that initiate vasoconstriction and systemic hypertension[3].
The main cause of pre-eclampsia is not well elucidated, although different previous studies implicated testosterone hormone as a causative factor in the pathogenesis of pre-eclampsia as the placentas of women with pre-eclampsia expressed high density of testosterone receptor. Similarly, high testosterone in women with polycystic ovary syndrome augments the risk and incidence of pre-eclampsia in future pregnancy[4]. An animal model study by Sathishkumar et al[5] illustrated that pregnant rats with high testosterone levels developed similar features of pre-eclampsia including hypertension, proteinuria, placental ischemia and endothelial dysfunction since high testosterone serum levels during pregnancy is correlated with placental dysfunction.
Therefore, it is possible that testosterone may play a potential role in the pathogenesis of pre-eclampsia through modulation of vascular reactivity and endothelial functions through activation of platelet aggregations and rennin-angiotensin system[6]. Besides,pre-eclampsia is associated with high free androgen index and total testosterone that induce vasoconstriction through the reduction of vasodilator prostacyclin and increase of vasoconstrictor thromboxane A2[7].
Therefore, the aim of the present study was to find the association between testosterone serum levels and the severity of late-onset pre-eclampsia.
2. Materials and methods
2.1. Study participants
A total of 68 participants were recruited in this case-control study.And selection of women with pre-eclampsia was done according to the diagnostic criteria of the American College of Obstetrician and Gynecologist[8]. Ten pregnant women with late-onset pre-eclampsia were excluded from this study due to different reasons, as revealed in the consort-flow diagram (Figure 1). Subsequent to the detailed full history concerning parity, pregnancy-related complications,cigarette smoking, current and previous pharmacotherapy, the included pregnant women (n=58) were divided into two groups after screening: the control group with 24 healthy pregnant women;the pre-eclampsia group with 34 pregnant women with late-onset pre-eclampsia.

Figure 1. Consort flow-chart of the present study.
2.2. Inclusion criteria
Pregnant women with a gestational age of 34 weeks or more with blood pressure equal or more than 140/90 mmHg without previous history of hypertension in relation to the smoking status were included. Healthy pregnant women with gestational age of 34 weeks or more were recruited as the control group. Maternal pre-eclampsia was regarded when systolic blood pressure (SBP)>140 mmHg and diastolic blood pressure (DBP)>90 mmHg with proteinuria >1 mg by dipstick; severe pre-eclampsia was considered when SBP>160 mmHg and DBP>110 mmHg with proteinuria >1 mg by dipstick. Other signs and symptoms including headache, convulsion,oliguria, visual disturbances and elevated serum creatinine were regarded as evidence of severe pre-eclampsia.
2.3. Exclusion criteria
Pregnant women with chronic hypertension, gestational hypertension, cardiovascular complications, endocrine disorders,metabolic disorders, gestational diabetes mellitus, psychiatric and mental disorders were excluded.
2.4. Assessment of biochemical parameters
Throughout scheduled visit to the consultant unit, 5 mL of venous blood from each patient with pre-eclampsia and control pregnant women was taken for the assessment of biochemical parameters, as below: Lipid profile: total cholesterol, triglyceride and high density lipoprotein (HDL) were measured by colorimetric kits. Very low density lipoprotein (VLDL) and low density lipoprotein (LDL)were measured according to the previous study[9]. Blood urea,serum creatinine and proteinuria were also assessed by biochemical calculation and the dipstick method respectively.
2.5. Hormonal assay
Serum total testosterone was estimated and measured by enzymelinked immunosorbent assay kit method (ADI-901-065, ENZO,France). Sex hormone-binding globulin (SHBG) was measured by enzyme-linked immunosorbent assay kit method (Human SHBG,MGC126834, China). Free androgen index was calculated by the specific equation according to Al-Kuraishy and Al-Gareeb method[10]:
Free androgen index = 100 × Serum total testosterone/SHBG
2.6. Assessment of blood pressure and anthropometric parameters
Blood pressure of each recruited pregnant women was measured at supine position from left arm by digital automated blood pressure monitoring two hours apart.
Pulse pressure=SBP-DBP
Mean arterial pressure = (SBP+2DBP)/3[11]
Body mass index (BMI) was calculated according to the specific equation: BMI=Body weight (kg)/Height (m2) when height was measured by graduated tape measure and body weight was measured by digital weight calculator. Gestational age was assessed by physical examination and dating from the first day of last menses in accordance with ultrasonographic imaging.
2.7. Assessment of smoking status
A full history of cigarette smoking in both pregnant women with late-onset pre-eclampsia and healthy control was evaluated.
2.8. Data analysis
The data were presented as mean±standard deviation (mean±SD)and unpaired Student’s t-test was used to determine the differences.Data analysis was done by using SPSS (IBM SPSS Statistics for Windows version 20.0, 2014 Armonk, NY, IBM, Corp, USA). The level of significance was regarded when P<0.05.
2.9. Ethics approval
The study was approved by the Ethical Committee of Biomedical Research of Al-Mustansiriyia University of Medicine with approval number 45AR 3/2/2019. Informed and written consents were obtained from all participants.
3. Results
3.1. Demographic characteristics of pregnant women with pre-eclampsia
In this case-control study, there were insignificant differences in age, BMI, gestational age and smoking status in pregnant women with pre-eclampsia compared with healthy pregnant women (the control) (P>0.05). Pregnant women with pre-eclampsia illustrated high proportion of nulliparity 82.35% compared with 8.33% in healthy pregnant women, which was reversed for the multiparty.Pregnant women with pre-eclampsia showed a higher incidence of cesarean section compared with healthy pregnant women(P=0.001). The rate of complications was high in pregnant women with pre-eclampsia compared with the healthy pregnant women(P<0.01). Other characteristics were described in Table 1.
3.2. Lipid profile and blood pressure changes in maternal pre-eclampsia
In the women with maternal pre-eclampsia, there were significant changes in lipid profile compared with healthy pregnant women(P<0.01) except for VLDL and triglyceride (P=0.560, P=0.060 respectively). The level of proteinuria was significantly higher in pregnant women with pre-eclampsia compared with healthy pregnant women (P<0.01). As well, blood urea and serum creatinine were significantly higher in pregnant women with preeclampsia when compared with healthy pregnant women (P<0.01).Moreover, SBP, DBP, and mean arterial pressure were significantly higher in patients with pre-eclampsia compared with healthy pregnant women (P<0.01). Also, there was a significant difference in pulse pressure between pregnant women with pre-eclampsia and healthy pregnant women (P<0.01) (Table 2).
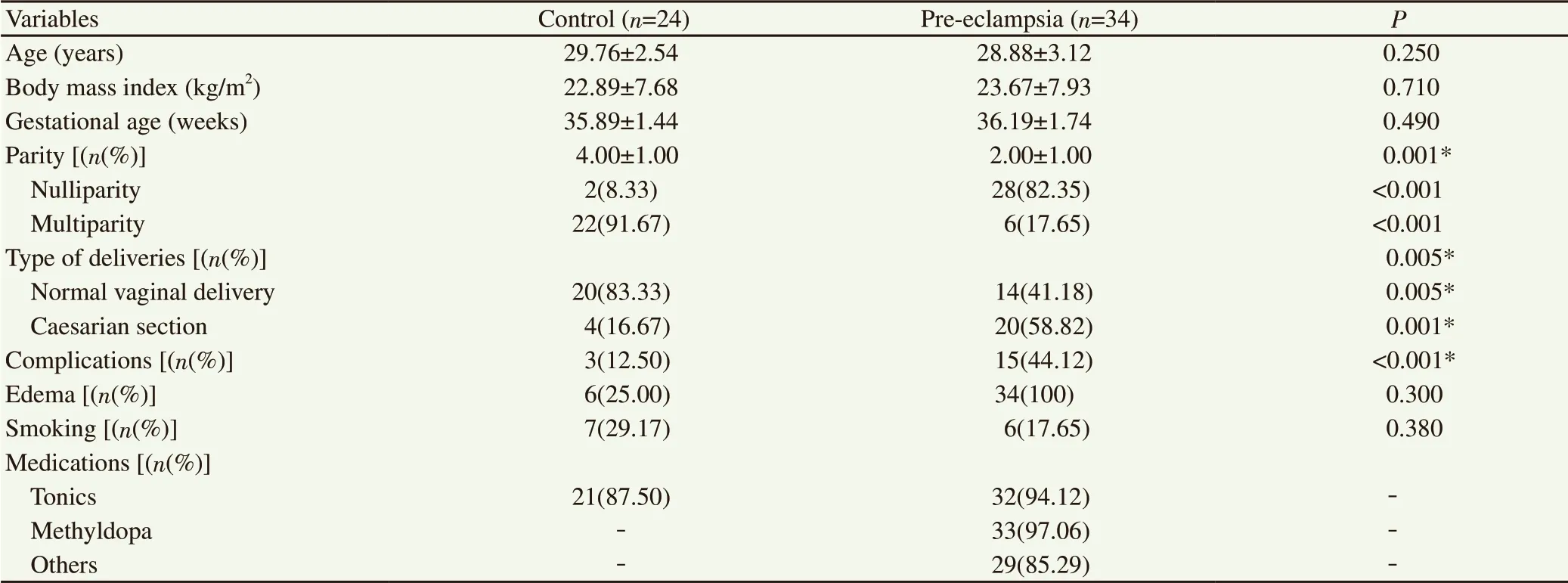
Table 1. Demographic and obstetric data of the present study.
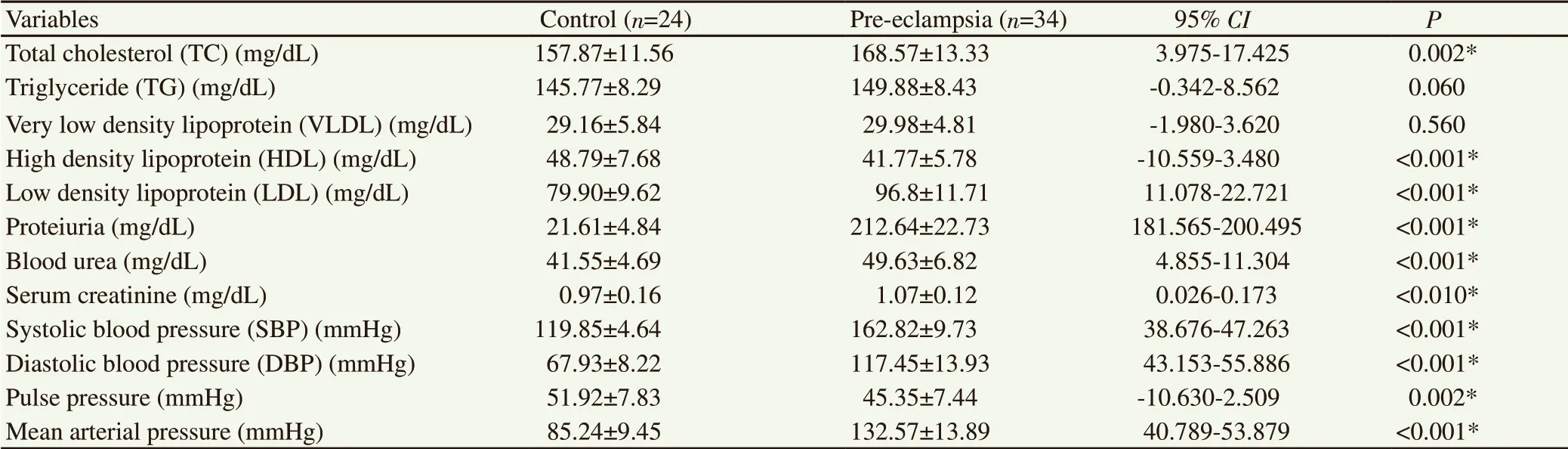
Table 2. Lipid profile and blood pressure changes in maternal pre-eclampsia compared with the control.
3.3. Serum testosterone level in pregnant women with pre-eclampsia
Regarding serum testosterone levels, serum total testosterone was significantly higher in pregnant women with pre-eclampsia compared with healthy pregnant women (P<0.01) (Figure 2A).Similarly, free androgen index was significantly higher in pregnant women with pre-eclampsia compared with healthy pregnant women (P<0.01) (Figure 2B). On the other hand, sex hormone binding globin (SHBG) level was significantly lower in pregnant women with pre-eclampsia compared with healthy pregnant women (P<0.01) (Figure 2C).
In the present study, serum total testosterone illustrated an insignificant correlation with lipid profile and blood pressure variables in the healthy control pregnant women (P>0.05). In pregnant women with pre-eclampsia, high serum total testosterone was significantly (P<0.01) correlated with all measured variables except for BMI and pulse pressure (both P=0.070) (Table 3).
3.4. Cigarette smoking in pregnant women with late-onset pre-eclampsia
Regarding the smoking status, 6(17.65%) of patients with late-onset pre-eclampsia were active smokers compared with 28(82.35%) non-smoker patients, which were significantly differed(P=0.001). In the control group, 7(29.17%) of healthy controls were active smokers compared with 17(70.83%), which was not significantly differed (P=0.06). The active smoker patients in lateonset pre-eclampsia were not significantly differed compared with healthy control (P=0.64), as well, non-smoker patients in lateonset pre-eclampsia were not significantly differed compared with the non-smoker controls (P=0.30) (Figure 3).
3.5. Types and number of delivery and testosterone serum levels in pregnant women with late-onset pre-eclampsia
High serum total testosterone level in pregnant women with lateonset pre-eclampsia was significantly correlated with number of caesarean sections (r=0.86, P<0.01) and nulliparity (r=0.56,P<0.01) compared with insignificant correlations in healthy controls. Therefore, high serum total testosterone was correlated more with caesarean section than nulliparity in the pregnant women with late-onset pre-eclampsia (Figure 4).

Figure 2. Serum total testosterone level (A), free androgen index (B), and sex hormone binding globulin (SHBG) level (C) in pregnant women with preeclampsia compared with healthy control pregnant women.
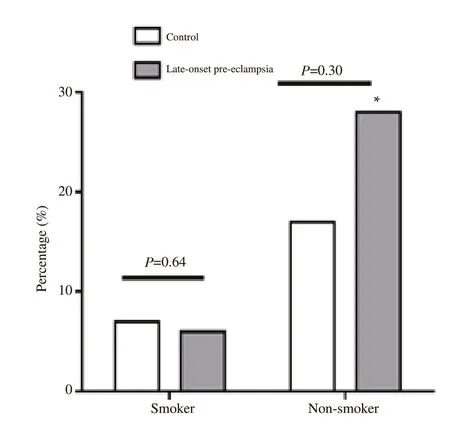
Figure 3. High percentage of non-smoking in patients with late-onset preeclampsia. *P<0.01 compared to smokers patients in late-onset pre-eclampsia.

Figure 4. Correlations of testosterone serum levels with nulliparity and cesarean sections in pregnant women with late-onset pre-eclampsia.
4. Discussion
Pre-eclampsia is a new onset of systolic and diastolic hypertension with proteinuria after 20 weeks of gestation. Pre-eclampsia which is mainly associated with overweight and nulliparity, as revealed in the present study since most of the recruited pre-eclamptic pregnant women were nulliparous and overweight. Likewise, the majority of pre-eclamptic pregnant women gave a history of cesarean section over that of normal vaginal delivery as supported by the study of Cho et al[11] that illustrated cesarean section in the first pregnancy provokes the incidence of pre-eclampsia due to vascular injury and uterine damage which account for abnormal placentation and poor trophoblastic invasion.
Indeed, all of the recruited pregnant were late-onset severe preeclampsia as hypertension profile was high more than 160/110 mmHg with significant proteinuria. In addition, both pulse pressure and mean arterial pressure were higher compared with healthy pregnant women. It has been reported that mean arterial pressure predicts the severity and complications of pre-eclampsia[12].
The results of the present study strongly suggest a significant association between high LDL and low HDL levels with the severity of pre-eclampsia since there is a negative correlation between HDL and severity of pre-eclampsia. Moreover, Nahar et al showed that hyperlipidemia in early pregnancy is linked with increased risk of pre-eclampsia[13].
In this study, high blood urea, serum creatinine and proteinuria were associated with the severity of pre-eclampsia due to acute kidney injury which is part of distant organ damage in severe preeclampsia. Severe hypertension during pre-eclampsia leads to renal ischemia and subsequent renal impairments which cause a reduction of glomerular filtration rate and increments in blood urea, serum creatinine and uric acid[14].
The core of the present study showed a significant elevation in the testosterone serum levels in pregnant women with pre-eclampsia compared with healthy pregnant women which confirmed the study of Sharifzadeh et al that proposed an association for high testosterone and risk of pre-eclampsia[14]. During normal pregnancy, testosterone serum levels are increased by about 70%,and this increase is augmented in women with pre-eclampsia.Besides, high testosterone levels are associated with high blood pressure in pre-eclampsia, as well experimentally induced high testosterone during late pregnancy led to hypertension and proteinuria that resembles testosterone level in pre-eclampsia[15].In late-onset pre-eclampsia, testosterone levels are correlated with severity of hypertension. In addition, free testosterone and free androgen index are augmented during pre-eclampsia[16].
In the present study, most of the patients with pre-eclampsia were overweighed which may explain the high testosterone levels since obesity and overweight contribute to elevation of testosterone levels[17]. Indeed, ethnicity may play a role in testosterone inducedpre-eclampsia in African and American pregnant women that exhibit high testosterone levels during pregnancy[18]. This risk factor was excluded from the present study as all of the recruited women with pre-eclampsia were of Asian ethnicity. It has been reported that fetal gender participates in high testosterone levels in pre-eclampsia. Male fetus, but not female fetus is linked with testosterone induced-pre-eclampsia[19]. Unfortunately, fetal sex was not determined in the present study.
High testosterone levels in pre-eclampsia modulate the renin-angiotensin system by increasing the sensitivity to the vasoconstrictor effect of angiotensinⅡwhich is normally blunted during normal pregnancy and direct activation of placental angiotensinⅡreceptors. The evidence for an association between testosterone and angiotensinⅡis up-regulation of angiotensinⅡreceptors in human placenta, and blockade of angiotensinⅡreceptor by losartan reverses high blood pressure in pre-eclampsia with high testosterone, suggesting that angiotensinⅡreceptor is a cause and not an outcome of high blood pressure[20].But in the present study, angiotensinⅡlevel and angiotensinⅡreceptors were not evaluated.
During normal pregnancy, peripheral resistance is decreased due to the activation of vasodilator factors including prostacyclin,nitric oxide and endothelium-derived hyperpolarizing factor. High testosterone levels in pre-eclampsia lead to significant inhibition of nitric oxide-mediated vasodilation via inhibition of nitric oxide synthesis and release with significant reduction of endothelial nitric oxide synthase. Likewise, elevated testosterone attenuates endothelium-derived hyperpolarizing factor and prostacyclin vasodilator effects[21].
Normally, placental aromatase converts maternal androgen to estrogen. Aromatase activity is severely reduced in patients with pre-eclampsia, leading to high testosterone and low estrogen levels. The reduction in placental aromatase is due to testosterone induced-placental ischemia[22]. Similarly, Shao et al[23] illustrated that high testosterone inhibits expression of aromatase activity and estrogen receptors. Therefore, high testosterone/estrogen ratio reflects functional defects in the placental aromatase.
The source and origin of testosterone in pre-eclampsia have remained obscure since human placenta lacks the enzyme for the synthesis of testosterone, but it is able to convert dehydroepiandrostendion into androgen. Fetal and maternal dehydroepiandrostendion may increase maternal testosterone biosynthesis at placental level[24]. As well, over-expression of CYP1A1 mRNA (which is involved in steroidogenesis) in human placenta could play a role in the elevation of testosterone in preeclampsia. But dehydroepiandrostendion level is not increased in pregnant women with pre-eclampsia, suggesting that adrenal origin of testosterone is not the main pathway of elevated testosterone[25].Furthermore, the findings of our study illustrated that a low level of SHBG in pregnant women with pre-eclampsia compared with healthy control. These results are in agreement with the study of Yu et al that confirmed the association of low SHBG with development of pre-eclampsia[26]. Usually, SHBG limits the exposure to high testosterone levels during normal pregnancy, and thus low levels of SHBG are associated with hyperandrogenism. It has been reported that low levels of SHBG are linked with the development of hypertension since SHBG reduces blood pressure via inhibition of rennin secretion and cAMP-dependent vasodilatation[27].Therefore, high testosterone and low level of SHBG in the present study may explain the mutual interaction in the development and severity of pre-eclampsia.
Moreover, there was a low percentage of active smoker patients compared with non-smoker patients, which might be a reason behind the development of late-onset pre-eclampsia and hypertensive severity. Lisonkova et al[28] reported the protective effect of cigarette smoking on the development of pre-eclampsia through inhibition of placental cytokine productions, suppression of vasoconstriction and oxidative stress by nicotine and carbon monoxide of smoking contents. As well, smoking reduces the risk of pre-eclampsia by 10%-40%[29].
Indeed, increasing smoking habits reduces testosterone levels significantly compared with non-smoker subjects in the study of Mitra et al[30]. This finding is consistence with our findings, as most of the recruited pregnant women with pre-eclampsia were non-smokers, which might explain the high level of testosterone in non-smoker pregnant women with pre-eclampsia.
Furthermore, high serum total testosterone levels were significantly correlated with a history of nulliparity and cesarean sections. Cesarean section induces anatomical and functional uterine changes such as scarring, capillary dilatations, lymphocytic infiltration and slight increase in the level of tumor necrosis factor-α[31]. These changes lead to abnormal uteroplacental circulation and induction of oxidative stress that stimulate placental testosterone production to overcome the oxidative stress and inflammatory changes[32]. Furthermore, this study showed a significant correlation between nulliparity and high serum total testosterone as reported by a previous study[33].
Finally, the present study has many limitations. First, this study was a single-center cross-sectional study that is able to explain the association not causality. Second, gender of the fetus, estrogen levels and other cytokines were not evaluated precisely. Third,dietary habit was not definitely mentioned as some diets may be involved in the pathogenesis of pre-eclampsia[34]. However, this study certainly confirmed the association between high testosterone and pre-eclampsia in spite of small sample size.
In conclusion, late-onset pre-eclampsia in pregnant women is associated with high serum total testosterone, high free androgen index, low SHBG, low smoking habit with positive history for nulliparity and cesarean sections that are correlated with high blood pressure profiles. Therefore, high serum total testosterone which is correlated with most of risk factors of late-onset pre-eclampsia is regarded as a proxy biomarker reflecting the severity of late onsetpre-eclampsia.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Acknowledgments
The authors acknowledge all staff members of post-graduated doctors for their participations in this study.
Authors' contributions
All authors contributed equally in data collection, data acquisition and analysis, data interpretations, manuscript writing, and finally that all authors approved the final version of the manuscript for publication.
 Asian Pacific Journal of Reproduction2020年1期
Asian Pacific Journal of Reproduction2020年1期
- Asian Pacific Journal of Reproduction的其它文章
- Assessment of antioxidant status of women with polycystic ovarian syndrome
- Novel genetic variants of transferrin receptor 2 exon 4 and cytokines profile of anemic and nonanemic pregnant women in Central Java, Indonesia
- Comparative proteomic analysis of mature and immature oocytes in domestic cats
- Estrogenic activity of hydroalcoholic extract of Clitoria ternatea Linn. leaves on rats
- Residual impact of 17α-methyltestosterone and histopathological changes in sexreversed Nile tilapia (Oreochromis niloticus)
- Identification of pathogenic microorganisms of repeat breeder dairy cows and a hyperimmune treatment approach
