Long-term outcomes of staged recanalization for concurrent chronic total occlusion in patients with ST-segment elevation myocardial infarction after primary percutaneous coronary intervention
Kong-Yong CUI, Fei YUAN, Hong LIU, Feng XU, Min ZHANG, Wei WANG, Ming-Duo ZHANG,Yun-Lu WANG, Dong-Feng ZHANG, Xiao ZHANG, Jin-Fan TIAN, Shu-Zheng LYU,#
1Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University and Beijing Institute of Heart, Lung and Blood Vessel Diseases,Beijing, China
2Department of Anesthesiology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
3Department of VIP Clinic, Beijing Anzhen Hospital, Capital Medical University, Beijing, China
Abstract Background In patients with acute ST-segment elevation myocardial infarction (STEMI) who undergo primary percutaneous coronary intervention (PCI), approximately 10% are concomitant with a chronic total occlusion (CTO) in a non-culprit vessel. However, the impact of staged CTO recanalization on prognosis in this cohort remains disputable. This study aimed to compare the long-term outcomes of staged CTO recanalization versus medical therapy in patients with STEMI after primary PCI. Methods Between January 2005 and December 2016, a total of 287 patients were treated with staged CTO-PCI (n = 91) or medical therapy (n = 196) after primary PCI in our center.The primary endpoint was major adverse cardiovascular and cerebrovascular event (MACCE), defined as a composite of all-cause death,nonfatal myocardial infarction (MI), stroke or unplanned revascularization. After propensity-score matching, 77 pairs of well-balanced patients were identified. Results The mean follow-up period was 6.06 years. Overall, the incidence of the primary endpoint of MACCE was significantly lower in staged CTO-PCI group than that in medical therapy group in both overall population (22.0% vs. 46.9%; hazard ratio(HR) = 0.48, 95% CI: 0.29-0.77) and propensity-matched cohorts (22.1% vs. 42.9%; HR: 0.48, 95% CI: 0.27-0.86). In addition, staged CTO-PCI was also associated with reduced risk of the composite of cardiac death, nonfatal MI or stroke compared with medical therapy in both overall population (9.9% vs. 26.5%; hazard ratio (HR) = 0.39, 95% CI: 0.19-0.79) and propensity-matched cohorts (9.1% vs. 22.1%;HR: 0.40, 95% CI: 0.16-0.96). After correction of the possible confounders, staged CTO-PCI was independently associated with reduced risks of MACCE (adjusted HR: 0.46, 95% CI: 0.28-0.75), the composite of cardiac death, nonfatal MI or stroke (adjusted HR: 0.45, 95% CI:0.22-0.94) and all-cause mortality (adjusted HR: 0.32, 95% CI: 0.13-0.83). Moreover, the results of sensitivity analysis were almost concordant with the overall analysis. Conclusions In patients with STEMI and a concurrent CTO who undergo primary PCI, successful staged recanalization of CTO in the non-culprit vessels is associated with better clinical outcomes during long-term follow-up.
Keywords: Concurrent chronic total occlusion; Long-term outcome; Staged recanalization; ST-segment elevation myocardial infarction
1 Introduction
In patients with acute ST-segment elevation myocardial infarction (STEMI) who are treated with primary percutaneous coronary intervention (PCI), approximately 10% are concomitant with chronic total occlusions (CTOs) in non-culprit vessels.[1,2]As the most severe manifestation of coronary artery disease, CTO is associated with increased morbidity and mortality in STEMI patients.[3,4]However,the impact of CTO recanalization in these patients continues to be debated. Several observational studies with short-term or midterm follow-up period demonstrated that successful staged PCI of CTO lesions could yield better clinical outcomes in STEMI patients after primary PCI,[5-8]whereas the prospective, randomized, multicenter EXPLORE (Evaluating Xience and left ventricular function in PCI on occlusiOns afteR STEMI) study did not find a beneficial effect of CTO-PCI with respect to left ventricular function and major adverse cardiac events, not even a trend.[9-11]Therefore, we conducted this study to assess the long-term impact of staged CTO recanalization in real-world STEMI patients who underwent primary PCI.
2 Methods
2.1 Study design and population
This was a single-center, retrospective, observational study. From January 2005 to December 2016, patients with acute STEMI who underwent primary PCI and had a concurrent CTO in a non-culprit artery in our center were consecutively enrolled. The ethical committee of Beijing Anzhen Hospital approved the study (No. 2012001) and all patients were informed of the study plan, yet written informed consent was waived due to retrospective enrollment. Besides,patient records were anonymized and de-identified before database merging and analysis. STEMI was defined as typical chest pain ≤ 12 h, elevated cardiac enzyme levels and significant ST-segment elevation of ≥ 0.1 mV in at least two leads or a new left bundle branch block. CTO was defined as a coronary obstruction with Thrombolysis in Myocardial Infarction flow grade 0 with or without anterograde or retrograde filling through collateral vessels.[12]
Of the 4,090 STEMI patients who referred to coronary angiology, 362 patients with CTO received primary PCI successfully. For this analysis, patients who refused study participation (n= 2), had a history of coronary artery bypass surgery (n= 2), or died before discharge (n= 13) were excluded. In addition, we did not include patients who had two CTOs (n= 10) or a side-branch CTO (n= 17) and those who subjected to coronary artery bypass surgery after primary PCI (n= 31).
2.2 Study procedures
All patients received loading doses of aspirin (300 mg),clopidogrel (600 mg) or ticagrelor (180 mg) before primary PCI. Culprit vessel was ascertained by the evaluation of electrocardiographic changes, echocardiographic and angiographic findings. Primary PCI as well as the use of heparin, thrombus aspiration, and glycoprotein IIb/IIIa inhibitor was in compliance with the current guidelines and the operators’ routine practice.[13,14]After the procedure, aspirin(100 mg/day) and clopidogrel (75 mg/day) or ticagrelor(180 mg/day) were prescribed at the same time every day.Staged CTO-PCI was often performed within 90 days after primary PCI, which was determined by the physicians and/or patients. All the CTOs were first attempted with the anterograde approach using dedicated coronary wires and devices, otherwise retrograde approach would be applied.Success of CTO-PCI was defined as a residual stenosis <30% with TIMI grade 3 flow. Of note, patients with failed PCI or initial medical therapy were assigned to medical therapy group.
2.3 Data collection and patient follow-up
Demographics, cardiovascular risk factors, clinical characteristics, angiographic and procedural details were collected from hospital databases and recorded in a computerized database. Follow-up information was partly obtained from the review of hospital charts, clinical visit or telephone interviews, which were conducted by trained reviewers. The follow-up period was extended through December 31, 2018 to ensure that all patients had an opportunity for at least 2 years’ follow-up information. The primary endpoint was major adverse cardiovascular and cerebrovascular event (MACCE),defined as a composite of all-cause death, nonfatal myocardial infarction (MI), stroke or unplanned revascularization.Secondary outcomes included all-cause death, cardiac death,nonfatal MI, stroke, unplanned revascularization and a composite of cardiac death, non-fatal MI or stroke. All deaths were considered to be cardiac-related unless a non-cardiac origin was documented. Diagnosis of MI was made according to fourth universal definition of myocardial infarction.[15]Stroke was defined as a new focal neurological deficit lasting > 24 h, which was confirmed by neurologists based on both clinical and radiographic criteria.[16]Unplanned revascularization was repeat PCI or coronary artery bypass grafting of CTO or non-CTO vessels excluding staged PCI. All the events were carefully verified and adjudicated by independent clinicians.
2.4 Statistical analysis
Categorical variables were expressed as frequencies(percentages), and the differences between the two groups were compared using the chi-square test or Fisher’s exact test. Continuous variables were expressed as mean ± SD or median (interquartile range), and were compared using the Student’sttest and Mann-WhitneyUtest according to different distributions. The Kaplan-Meier method was used to plot time-to-event curves, and differences were assessed using log-rank test. To find predictors of clinical events,Cox proportional hazard model analysis was conducted to evaluate adjusted hazard ratios (HRs) with 95% confidence intervals (CIs). Variables in Table 1 withP≤ 0.1 at the univariate analysis were entered into the model.
To adjust for confounders, we compared the differences of clinical outcomes between the two groups in a propensity-matched population. Patients who received successfulCTO recanalization were matched 1: 1 with patients randomly selected from the medical therapy group with no replacement, on the basis of the nearest neighbor in terms of Mahalanobis distance with a caliper of 0.02. The propensity score was estimated with a logistic regression model with the variables of age, male, current smoking, diabetes mellitus, previous MI, previous PCI, previous stroke, peripheral vascular disease, time from symptom onset to PCI, access site of PCI, Killip class III/IV, number of diseased vessels,culprit vessel of left anterior descending coronary artery(LAD), CTO located in LAD, use of thrombus aspiration,no-reflow phenomenon, use of intra-aortic balloon pump,use of glycoprotein IIb/IIIa inhibitor, use of angiotensinconverting enzyme inhibitors or angiotensin receptor blocker,and use of β-blocker.
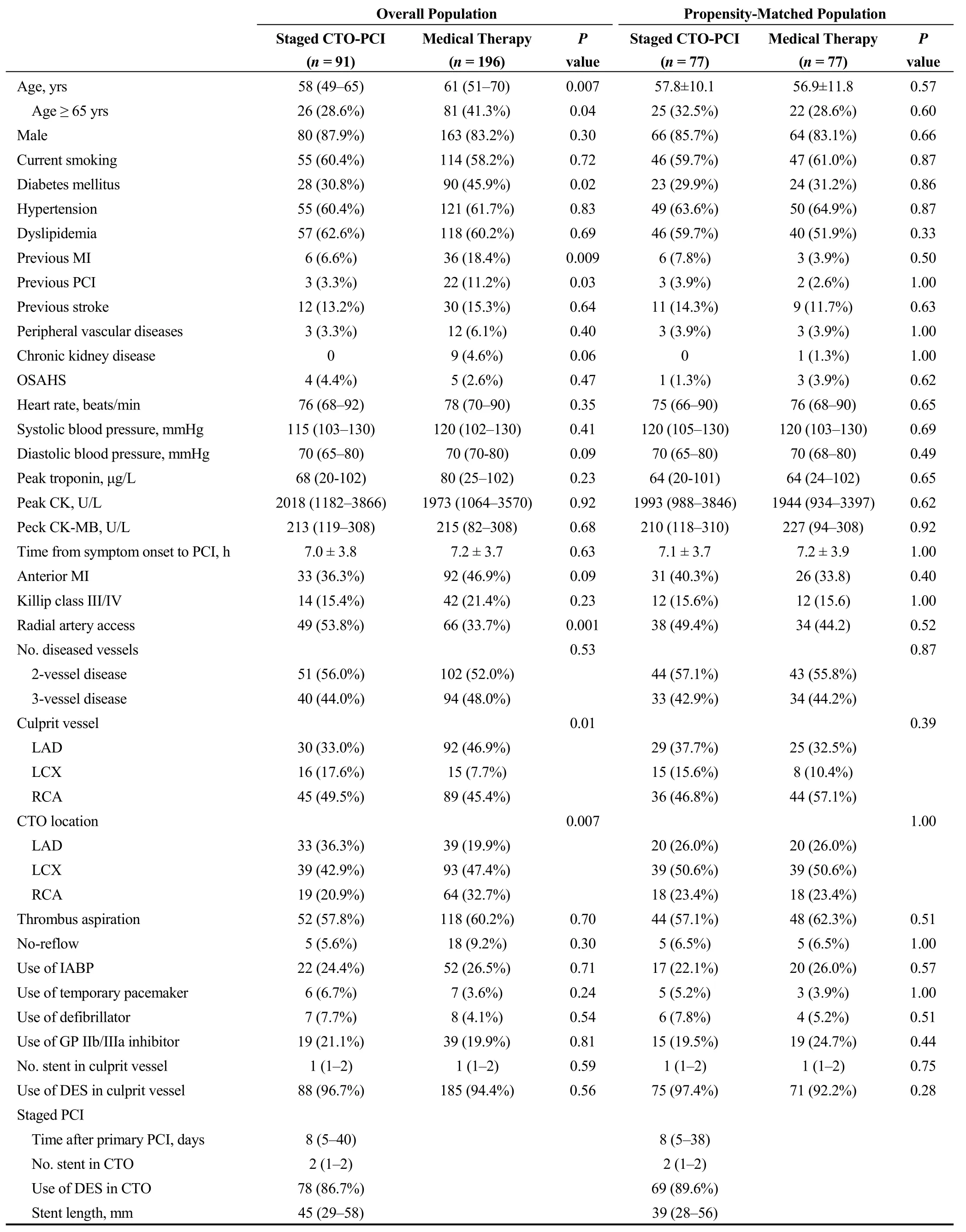
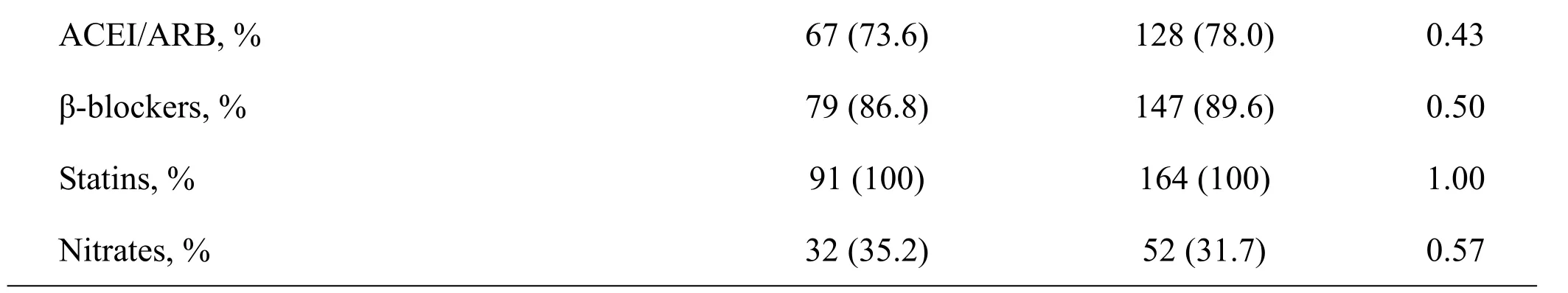
Table 1. Baseline patient and procedural characteristics before and after propensity score matching analysis.

Table 1. Cont.
Besides, eight prespecified subgroup analyses were performed for the primary endpoint among the overall population. To assess the robustness of the results, long-term outcomes of patients undergoing staged CTO-PCI were compared with those receiving initial medical therapy. All statistical analyses were conducted using SPSS 23.0 (SPSS Inc., Chicago, Illinois, USA) and STATA 12.0 (StataCorp,College Station, Texas, USA). A two-sidedPvalue of <0.05 was considered to indicate statistical significance.
3 Results
3.1 Baseline patient and angiographic characteristics
Among the 287 STEMI patients included in our analysis,91 were assigned to staged CTO-PCI group and 196 were assigned to medical therapy group, including 32 patients who underwent failed CTO-PCI (Figure 1). Baseline patient and procedural characteristics of the overall population were summarized in Table 1. Compared with patients in medical therapy group, patients who received staged CTO-PCI were younger (58vs.61 years), less likely to had diabetes (30.8%vs. 45.9%), prior MI (6.6%vs. 18.4%), prior PCI (3.3%vs.11.2%) and a culprit vessel of LAD (33.0%vs. 46.9%),whereas transradial coronary intervention (53.8%vs. 33.7%)and CTO located in LAD (36.3%vs. 19.9%) were more commonly seen in these patients. After propensity scorematching, 77 pairs of well-balanced patients were identified(Table 1).
3.2 Unadjusted outcomes
There was no periprocedural death, MI, cardiac tamponade or emergency cardiac surgery during staged CTO-PCI.The mean follow-up period was 6.06 years. The incidence of the primary endpoint was significantly lower in the staged CTO-PCI group than that in the medical therapy group (22.0%vs. 46.9%; HR = 0.48, 95% CI: 0.29-0.77;Table 2 and Figure 2A). Moreover, this finding was consistent across all prespecified subgroups (Figure 3). Additionally, successful CTO-PCI was associated with reduced risks of the composite of cardiac death, nonfatal MI or stroke(9.9%vs. 26.5%; HR = 0.39, 95% CI: 0.19-0.79; Table 2 and Figure 2B), all-cause mortality (5.5%vs. 20.9%; HR =0.28, 95% CI: 0.11-0.70; Table 2 and Figure 2C) and cardiac mortality (4.4%vs. 16.8%; HR = 0.27, 95% CI:0.10-0.76; Table 2) compared with conservative treatment.No difference was found between the two groups regard as the other secondary outcomes (Table 2).
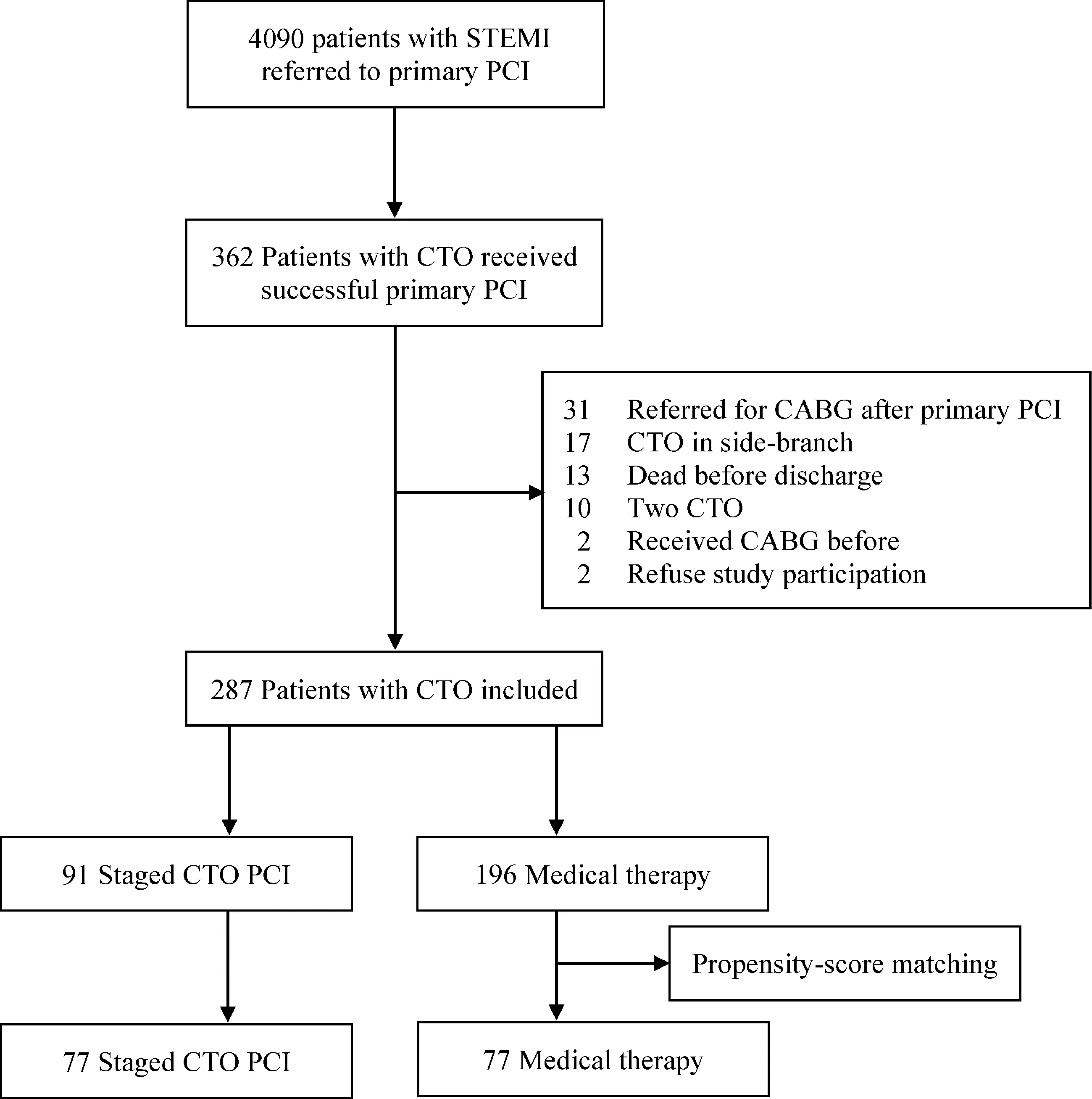
Figure 1. Flow diagram of patient selection. CABG: coronary artery bypass grafting; CTO: chronic total occlusion; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction.
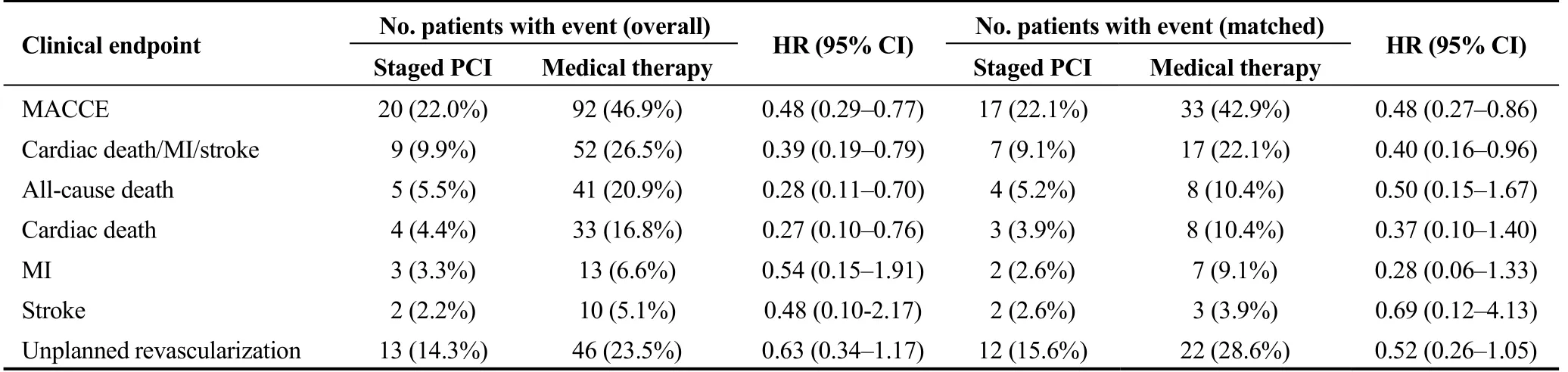
Table 2. Long-term outcomes in overall population and propensity-matched population.
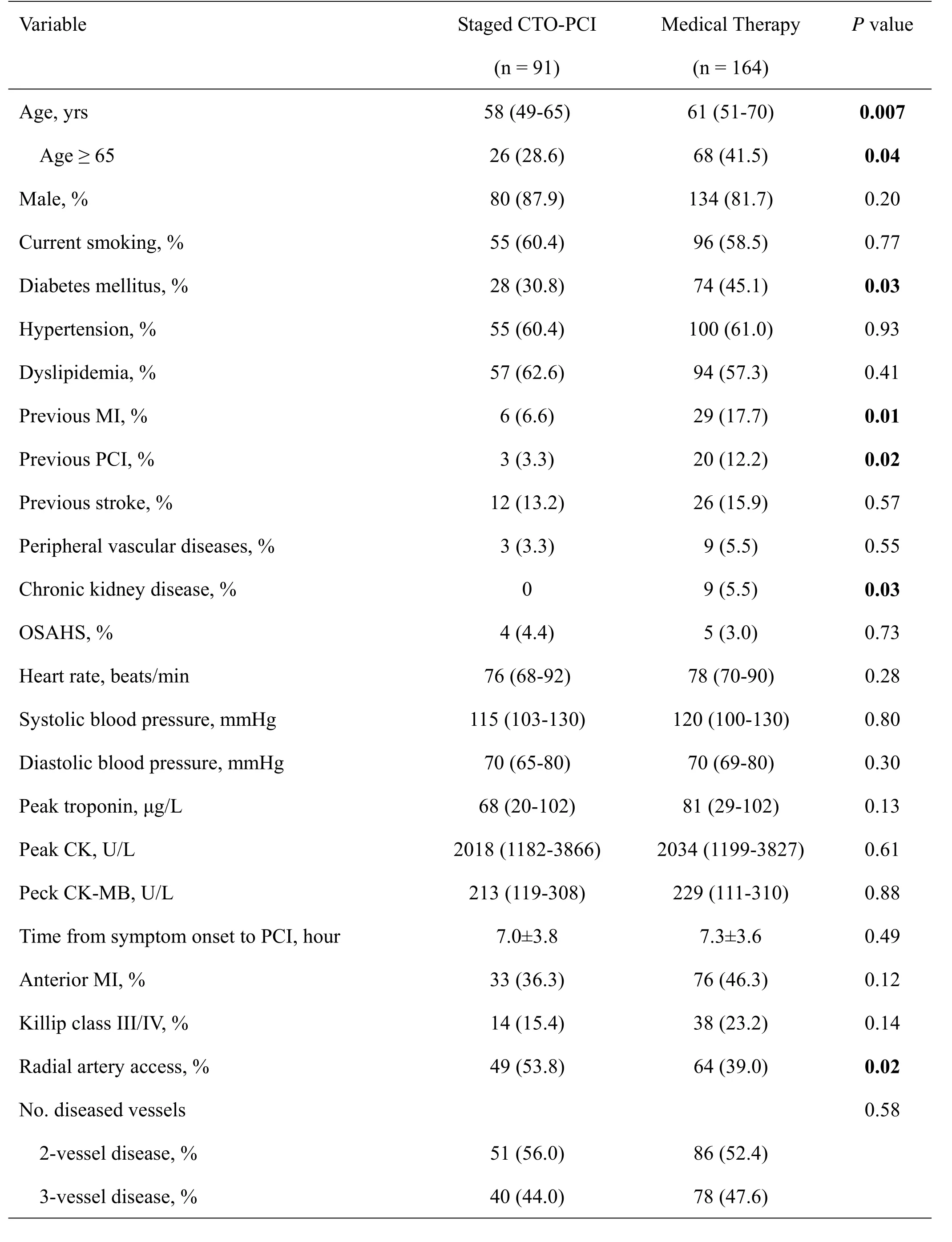
3.3 Cox proportional hazards regression analysis
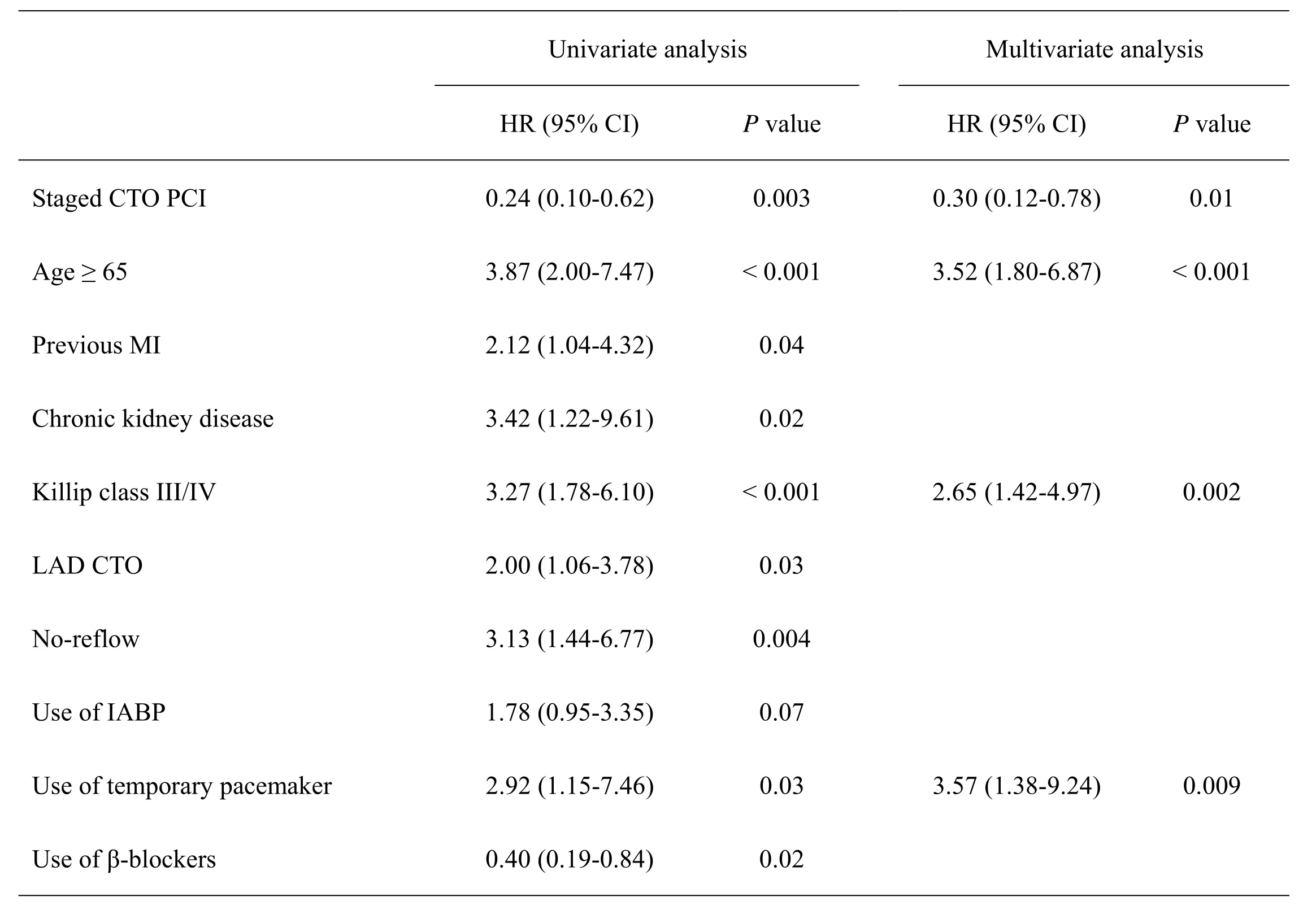
After correction of the possible confounders, staged CTO-PCI was independently associated with reduced risk of the primary endpoint of MACCE (adjusted HR = 0.46,95% CI: 0.28-0.75,P= 0.002; Table 3). Besides, other independent predictors for the primary endpoint were current smoking (P= 0.04), chronic kidney disease (P= 0.01), systolic blood pressure (P= 0.02) and use of temporary pacemaker (P= 0.03). Furthermore, staged CTO recanalization was also a significant predictor of lower risks of the composite of cardiac death, nonfatal MI or stroke (adjusted HR = 0.45,95% CI: 0.22-0.94,P= 0.03; Table 4) and all-cause mortality(adjusted HR = 0.32, 95% CI: 0.13-0.83,P= 0.02; Table 5).
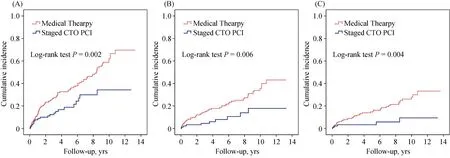
Figure 2. Kaplan-Meier event rate curves of main clinical outcomes in overall population. (A): MACCE; (B): cardiac death/MI/stroke;(C): all-cause death. CTO: chronic total occlusion; MACCE: major adverse cardiovascular and cerebrovascular event; MI: myocardial infarction; PCI: percutaneous coronary intervention.

Figure 3. Subgroup analysis for the primary endpoint in overall population. CTO: chronic total occlusion; LAD: left anterior descending coronary artery; PCI: percutaneous coronary intervention.
3.4 Propensity-matched analysis
Results of propensity-matched analysis regarding the primary endpoint of MACCE (22.1%vs. 42.9%; HR = 0.48,95% CI: 0.27-0.86; Table 2 and Figure 4A) and the composite of cardiac death, nonfatal MI or stroke (9.1%vs.22.1%; HR = 0.40, 95% CI: 0.16-0.96; Table 2 and Figure 4B) were mostly in line with the overall analysis. However,the risk of all-cause death (5.2%vs.10.4%; HR = 0.50, 95%CI: 0.15-1.67; Table 2 and Figure 4C) as well as the other secondary endpoints were comparable between the two treatment strategies.
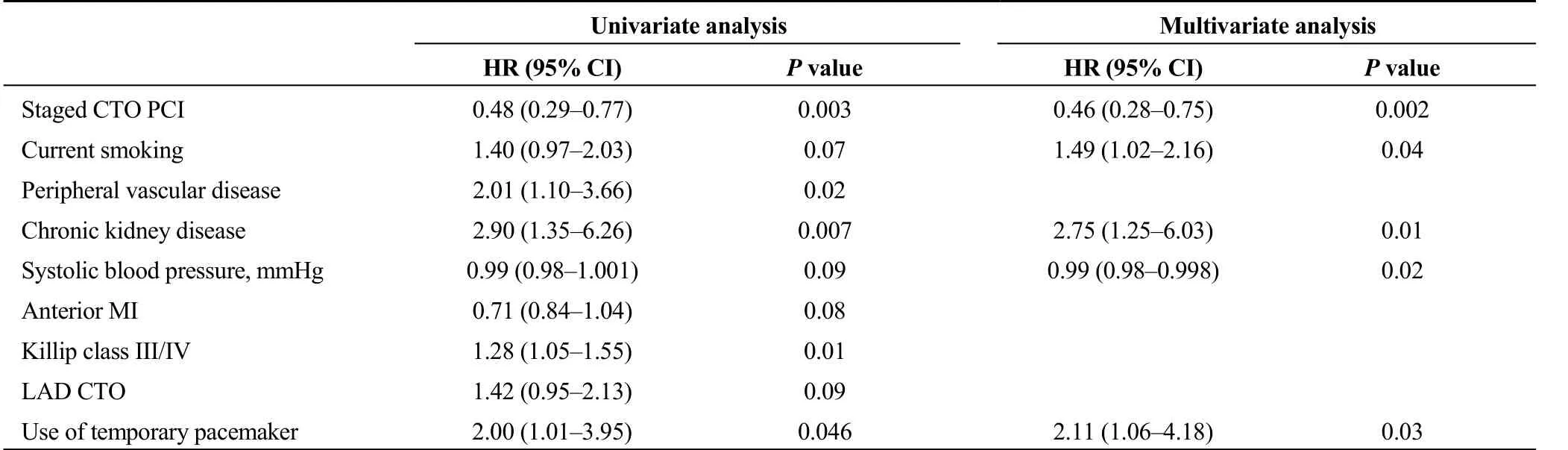
Table 3. Cox proportion hazards analysis for predictors of the primary endpoint during 6-year follow-up.

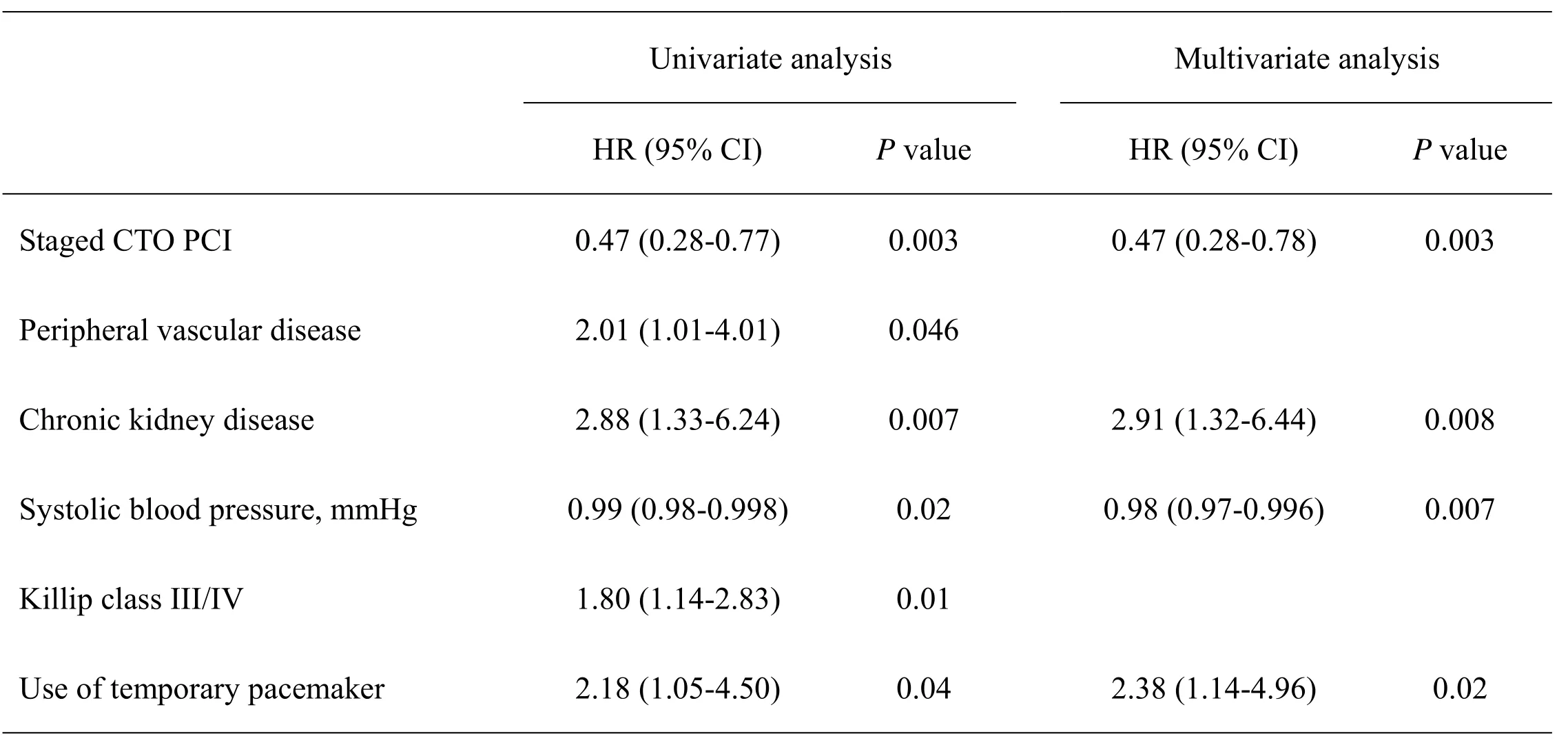
Table 5. Cox proportion hazards analysis for predictors of all-cause mortality during 6-year follow-up.

Figure 4. Kaplan-Meier event rate curves of main clinical outcomes in propensity-matched population. (A): MACCE; (B): cardiac death/MI/stroke; (C): all-cause death. CTO: chronic total occlusion; MACCE: major adverse cardiovascular and cerebrovascular event; MI:myocardial infarction; PCI: percutaneous coronary intervention.
3.5 Sensitivity analysis
Sensitivity analysis comparing patients undergoing staged CTO recanalization versus those receiving initial medical therapy was almost concordant with the overall analysis(supplemental Table S1). Staged CTO-PCI was associated with lower risks of MACCE, a composite of cardiac death,nonfatal MI or stroke, all-cause mortality and cardiac mortality at 6-year follow-up (supplemental Table S2). After adjusting potential confounders, the strategy of staged CTOPCI was independently associated with lower incidences of MACCE (adjusted HR = 0.47, 95% CI: 0.28-0.78,P=0.003; supplemental Table S3) and all-cause mortality (adjusted HR = 0.30, 95% CI: 0.12-0.78,P= 0.01; supplemental Table S4).
4 Discussion
In our center, approximately 30% of patients with STEMI and a concurrent CTO received successful CTO recanalization within 90 days after primary PCI. Actually, our study confirms and extends the results of previous observational studies with short-term or midterm follow-up period. We found that staged CTO recanalization had a beneficial effect on long-term prognosis for STEMI patients who underwent primary PCI. Notably, this finding was demonstrated by multivariable adjusted analysis, propensity score-matching analysis and sensitivity analysis. Furthermore, this effect was consistent in all predefined subgroups with no interactions found.
A growing body of evidence had demonstrated that the presence of concurrent CTO is associated with increased risk of major adverse cardiac events when compared with patients with single-vessel disease as well as multi-vessel disease without a CTO.[4]One of the possible mechanism is that patients with a concomitant CTO have a higher prevalence of cardiovascular risk factors and comorbidities. Besides, patients with CTO are prone to a larger infarct size due to acute occlusion of a donor artery to CTO if the distal coronary bed of CTO depends upon collateral blood flow from the culprit vessel.[17]Thus, these patients are often associated with reduced residual left ventricular ejection fraction, and further deterioration of left ventricular function.Worse still, revascularization of CTO remains challenging in consideration of the procedural complexity, low success rates, long procedure times, large amounts of contrast consumption, and frequent complications. In this setting, few cardiologists are willing to perform the procedure of CTO recanalization.
So far, several randomized controlled trials and guidelines have suggested the strategy of staged PCI of non-culprit lesions after primary PCI in patients who presented with STMEI and multivessel disease.[13,14,18-21]Nevertheless, as a special subgroup of multivessel disease, the impact of staged CTO recanalization on clinical outcomes remains unclear in these patients. Previous studies have indicated that staged CTO-PCI was associated with lower risks of short-term or midterm cardiac mortality and major adverse cardiac events in this population,[5-8]whereas the study conducted by Watanabe and colleagues found that the 5-year incidence of all-cause death was not significantly different between the successful CTO-PCI and the failed CTO-PCI groups with only 121 patients enrolled.[22]Furthermore, the only randomized EXPLORE trial, which assigned 304 STEMI patients to early CTO-PCI or conservative therapy groups after primary PCI, did not find statistical differences between the two strategies in terms of 1-year left ventricular ejection fraction and 3.9-year clinical outcomes.[11]However, it should be noted that the randomized CTO recanalization was performed after 5 days (mean) of primary PCI, when inflammation plays an important role during the acute setting of STEMI and the recovery, leading to larger infarct sizes and left ventricular remodeling after staged non-culprit PCI.[11]In addition, a relatively lower level of successful CTO-PCI (73%) could mask the value of CTO recanalization.
Similar to the results of most observational studies, the present study demonstrated that staged CTO-PCI could lower the long-term risks of MACCE, the composite endpoint of cardiac death, nonfatal MI or stroke and all-cause mortality. The clinical benefit of staged CTO-PCI can partly be explained by improvement of healing process in the infarct border zone, especially when the perfusion area of the culprit vessel and the CTO are adjacent or overlapping. Another explanation is the restoration of contractile function in the CTO territory, i.e., hibernating myocardium. Luckily,the functional recovery in hibernating myocardium after revascularization is paralleled by restoration of an adequate coronary flow reserve.[23]In addition, a large majority of patients in the CTO-PCI group had a complete revascularization, which is beneficial for long-term survival.[24,25]Hence, staged CTO-PCI could improve left ventricular function, reduce ventricular remodeling and increase tolerance to future ischemic events. Furthermore, it was associated with a decreased incidence of ventricular arrhythmias due to an ischemia-induced prolongation of the QT interval.[26]
Our results should be interpreted with caution in the context of several important limitations. Firstly, the single-center, nonrandomized nature of the study limited the ability to control unmeasured confounding factors. Although we used multivariable adjusted analysis and propensity-matched analysis, it was hard to account for all the confounding factors and selection bias. In clinical scenarios,sick patients are less likely to receive staged CTO-PCI unless they have refractory angina due to the present of CTO. Secondly, since the sample size was relatively small in the present study, we acknowledged that our results may be affected by type I and II errors. Thirdly, participants were collected across a 12-year time span. During this time, PCI was subject to change in stent type, interventional techniques and devices as well as antiplatelet therapies, thus potentially influencing the results. Fourthly, detailed ischemic status of the CTO territory in asymptomatic patients before recanalization was still lacking. Lastly, the high number of predictors screened might result in an overfitting. However, the propensity-matched analysis could reduce the problem of overfitting.
In conclusion, in patients with STEMI and a concurrent CTO who undergo primary PCI, successful staged recanalization of CTO in the non-culprit vessels is associated with better clinical outcomes during long-term follow-up. Staged CTO-PCI should be conducted by skilled and experienced operators given the complexity of CTO lesions. The findings warrant prospective evaluation through well-designed,large adequately powered, randomized trials with long-term follow-up duration.
Acknowledgements
The study was funded by the Ministry of Science and Technology of the People’s Republic of China, State Science and Technology Support Program (No.2011BAI11B05)and Beijing Lab for Cardiovascular Precision Medicine,Beijing, China (PXM2019_014226_000023).
Online Table S1. Baseline patient and procedural characteristics in sensitivity analysis.

Culprit vessel 0.03 LAD, % 30 (33.0) 74 (45.1)LCX, % 16 (17.6) 13 (7.9)RCA, % 45 (49.5) 77 (47.0)CTO location 0.002 LAD, % 33 (36.3) 28 (17.1)LCX, % 39 (42.9) 82 (50.0)RCA, % 19 (20.9) 54 (32.9)Thrombus aspiration, % 52 (57.8) 103 (62.8) 0.43 No-reflow, % 5 (5.6) 16 (9.8) 0.25 Use of IABP, % 22 (24.4) 41 (25.0) 0.92 Use of temporary pacemaker, % 6 (6.7) 6 (3.7) 0.36 Use of defibrillator, % 7 (7.7) 6 (3.7) 0.23 Use of GP IIb/IIIa inhibitor, % 19 (21.1) 35 (21.3) 0.97 No. stent in culprit vessel 1 (1-2) 1 (1-2) 0.58 Use of DES in culprit vessel, % 88 (96.7) 155 (94.5) 0.55 Staged PCI Time after primary PCI, days 8 (5-40)No. stent in CTO 2 (1-2)Use of DES in CTO, % 78 (86.7)Stent length, mm 45 (29-58)Minimum stent diameter, mm 2.50 (2.25-2.50)Anterograde approach, % 88 (96.7)Other vessel PCI Non-culprit vessel, non-CTO PCI, % 21 (23.1) 23 (14.0) 0.07 Complete revascularization, % 73 (80.2)Medications at discharge Aspirin, % 91 (100) 162 (98.8) 0.54 P2Y12 receptor inhibitor, % 91 (100) 164 (100) 1.00
Data were presented as median (interquartile range), mean ± standard deviation or n (%). ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; CK-MB, creatine kinase myocardial band;CTO, chronic total occlusion; DES, drug-eluting stent; IABP, intra-aortic balloon pump; LAD, left anterior descending coronary artery; LCX, left circumflex coronary artery; MI, myocardial infarction; OSAHS,obstructive sleep apnea-hypopnea syndrome; PCI, percutaneous coronary intervention; RCA, right coronary artery.

Online Table S2. Long-term outcomes in sensitivity analysis.
Online Table S3. Cox proportion hazards analysis for predictors of the primary endpoint during 6-year follow-up in sensitivity analysis.
Online Table S4. Cox proportion hazards analysis for predictors of all-cause mortality during 6-year follow-up in sensitivity analysis.
 Journal of Geriatric Cardiology2020年1期
Journal of Geriatric Cardiology2020年1期
- Journal of Geriatric Cardiology的其它文章
- Polymorphic ventricular tachycardia during phase II cardiac rehabilitation in a patient with heart failure: a case report
- “One-man” bailout technique for high-speed rotational atherectomy—assisted percutaneous coronary intervention in an octogenarian
- Aspergillus infection of pacemaker in an immunocompetent host: a case report
- Is dual therapy the correct strategy in frail elderly patients with atrial fibrillation and acute coronary syndrome?
- A meta-analysis of 1-year outcomes of transcatheter versus surgical aortic valve replacement in low-risk patients with severe aortic stenosis
- Anemia in patients with high-risk acute coronary syndromes admitted to Intensive Cardiac Care Units
