Corrections in alpha angle following two different operative approaches for CAM-type femoral acetabular impingement - Ganz surgical hip dislocation vs anterior mini-open
Emanuel C Haug, Wendy M Novicoff, Quanjun Cui
Emanuel C Haug, Wendy M Novicoff, Quanjun Cui, Department of Orthopedic Surgery,University of Virginia School of Medicine, Charlottesville, VA 22908, United States
Abstract
Key words: Alpha angle; Femoroacetabular impingement; Ganz surgical hip dislocation;Anterior mini-open
INTRODUCTION
The pathology for femoroacetabular impingement (FAI) may be noted in the acetabulum, the head- neck junction of the proximal femur, or a combination of the two. It can be seen in all age groups and there is new evidence suggesting occurrence in younger patients than previously seen, as well as, specific sex-dependent characteristics between males and females[1-3].
The mechanism by which FAI occurs is generally classified into three categories.Type I describes a CAM-type impingement where the femoral head and neck region creates asphericity, the head-neck offset is reduced, with increased alpha angle. This region may be covered by hyaline cartilage and could be developmental in origin due to incomplete separation of the growth plates of the femoral head and the trochanter.This physeal growth abnormality has been shown to cause the non-spherical contour with lateral epiphyseal extension[4]. An adolescent growth spurt and a known history of a slipped capital femoral epiphysis can also predispose a person to this type of asymmetry. As with many orthopaedic conditions, musculoskeletal injury may also contribute to the alteration of the shape of head and neck region and cause this CAM-type impingement effect. Ultimately, and largely regardless of predisposing etiology,this abnormal impingement type mechanism leads to secondary osteoarthritis of the hip joint. The reason for this is that the structural abnormality leads to chronic abutment of the femoral neck and the rim of acetabulum in flexion and internal rotation of the hip joint. This causes atypical and increased compression and shear forces which results in chondral lesions, labral tears and osteoarthrosis[1]. Therefore,early detection and removal of the asphericity alleviates this mechanical mismatch and oftentimes significantly improves the patient’s symptomatology. To this end,various techniques (i.e., arthroscopic procedures ranging to more extensive open methods) have been well described in today’s literature and are broadly accepted and employed in everyday practice[5-8].
Type II impingement is consistent with a pincer mechanism. This is generally defined by over-coverage of the femoral head and neck by the acetabulum. The acetabular socket is abnormally deep or retroverted while the femoral neck is generally normal. An anteroposterior (AP) pelvis radiograph can demonstrate such signs to a good extent. This increased coverage inherently limits motion of the hip joint and, at extremes of motion, causes the neck to impinge on the acetabular labrum and socket. Over time, this is known to lead to degenerative cleavage in the labrum and circumferential cartilage damage[1]. In this case, treatment is aimed at resecting the prominent acetabular rim to allow for impingement free range of motion. As with type I, there are various surgical techniques described for type II pathology depending on surgeon’s individual comfort level.
The third and last general type of FAI is more common than the isolated type I or II lesions, and it is a combination of both the cam and pincer pathology. Thus, the surgical treatment for the type III mechanistic mismatch is aimed to address the femoral neck region along with the acetabular rim. Traditionally, whenever both intra- and extra-articular pathology and deformity need to be addressed, the open hip dislocation offers satisfactory exposure and access[9].
To determine and qualify the presence of Cam type morphology, a radiographic calculation of the alpha angle is most often employed. It provides reliable information for operative planning and helps to monitor the progress in the immediate postoperative period and on subsequent follow up. While generally calculated on standard radiographs, the researchers described this angle on magnetic resonance imaging as well[10,11]. The angle is subtended by a line drawn in the middle of the femoral neck to the center of the head and a line drawn from the center of the femoral head to a point where head extrudes the perfect circle drawn around it[12]. The crosstable lateral radiograph with the femur in 15 degree of internal rotation and a Dunn view in flexion evaluate the aspheric morphology appropriately. The frog lateral views also provide comparable information[13,14]. It is worthy to mention that this pathology may be missed on a cross-table view with femur in external rotation, as well as, on direct AP radiographs[10].
An appropriately measured angle affords a reliable metric to assess the postoperative correction, irrespective of the technique utilized, and helps to correlate impingement free motion[11]. To our knowledge, the correlation of alpha angle improvement has not been compared between various operative techniques,especially the extensile traditional and modern anterior mini-open approach.
Therefore, the aims of this study were to determine (1) Change from baseline in the alpha angle on cross-table lateral radiograph (with leg in 15 degree internal rotation)after surgery; and (2) Compare radiographic corrections between the Ganz surgical hip dislocation and anterior mini-open.
MATERIALS AND METHODS
Institutional review board approval was obtained prior to commencement of the study. The institutional data of the patients who underwent surgery for FAI under a single surgeon were abstracted from a large medical center’s records ranging from 2007 to 2012. All patients with pre- and post-operative radiographs were screened.Patients with missing radiographic documentation, radiographs with insufficient quality which then precluded accurate measurement of the angle α, a diagnosed congenital condition, isolated type II pathology (Pincer), and history of prior surgery were excluded from the study.
The Ganz surgical hip dislocation[15]was performed in a lateral decubitus position.A trochanteric flip osteotomy was used to achieve an anterior approach to the hip joint. The thickness of the trochanter was kept at approximately 1.5 cm and the gluteus medius and vastus lateralis were kept intact. A Z-shaped capsulotomy was then performed in the order of anterolateral limb in line with the neck, a distal anteroinferior extension in front of the lesser trochanter and finally a curved posterolateral limb between gluteus minimus and piriformis in line with the acetabular rim. The main aim of this approach was to preserve the profundus branch of medial femoral circumflex artery (MFCA) at the time of osteotomy. This also served to protect the medial branch at the level of lesser trochanter and contact anastomosis of inferior gluteal and MFCA posteriorly during the capsulotomy. Next, the femoral head was dislocated from the acetabulum and the pathology was assessed.Depending on extent of damage and viability, the labrum was either debrided or repaired. Then, the cam lesion was shaved carefully with a 5-mm diameter high-speed burr in order to more accurately restore the normal femoral neck morphology. The bone was removed to a safe level of a 4-5 mm depth until an impingement free range of motion was achieved in 90 degrees of flexion and 10-15 degrees of internal rotation[11]. This was assessed intraoperatively prior to closure. The deep capsule was first closed in interrupted fashion. The trochanter was then reattached and held down with two small fragment screws and, finally, the skin was closed with subcutaneous absorbable sutures.
The second group in this study underwent an anterior mini-open approach. A partial anterior approach to the hip, the “Heuter Approach," also called the “Short Smith-Pete” because it follows the interval of the formal Smith- Petersen distal to the anterior superior iliac spine, was used for access to the capsule and femoral neck[16-18].All patients were positioned supine with a small well-padded bump under the pelvis.The incision was commenced slightly lateral and inferior to anteriorsuperior iliac spine and then continued distally for 3-5.5 cm. The dissection was carried down to the capsule via the intramuscular (sartorius and tensor fascia lata) and internervous planes (femoral and superior gluteal nerves). Care was taken to avoid injury the branches of lateral cutaneous nerve to thigh, and the ascending branch of lateral femoral circumflex was ligated wherever necessary. Capulotomy was carried out in line with the femoral neck with hip in flexion and then extended proximally around the acetabular rim while taking care to avoid damage to the cartilage and labrum.Blunt reactors are placed around the neck to expose the hip joint. To address the abnormal bony morphology, we employed similar steps as described above for the formal surgical hip dislocation. Then, a standard layered closure from deep to superficial was performed with the skin re-approximated in a sub-cuticular fashion.
To compare the differences in the alpha angles between the two surgical approaches, and to determine if age or gender were associated with the choice of surgical approach, two-samplet-tests and Chi-square analyses were employed,depending on the nature of the variables. All statistical analysis was done using SPSS Version 21.
TraumaCad® software (Voyant Health, Petach-Tikva, Israel) was utilized to measure the alpha angle[11,12].
RESULTS
A total of 79 patients met the inclusion and exclusion criteria and had available records from the 5-year study period. Forty-seven males (mean age of 35.3, range 16-53) and 32 females (mean age 36.7, range 16-60) were enrolled. Forty-seven patients underwent the anterior mini-open approach, and 32 underwent the Ganz surgical hip dislocation. Pre-operatively, all patients were symptomatic and showed clinical and radiological features of impingement without significant degenerative changes. There were no significant differences in age between the two surgical groups or in pre- and post-operative alpha angles based on patient gender.
The overall angle correction achieved by both methods is shown in Figure 1. The mean pre-operative alpha angle for the Ganz surgical hip dislocation group was 88.0 degrees (SD 12.3) and 99.4 degrees (SD 7.2) for the anterior mini-open group. Mean post-operative angles were 49.9 degrees (SD 4.3) for the Ganz surgical hip dislocation and 43.8 (SD 4.3) degrees for the anterior mini-open group (Table 1). There was a statistically significant difference in patient’s pre-operative and post-operative angles(P= 0.000) with both surgical approaches.
DISCUSSION
With a progressively better understanding of the abnormal femoroacetabular morphologies which can ultimately lead to secondary cartilage and labrum damage,mechanistic impingement has been recognized as one of the leading causes for early degeneration of the hip joint[1]. The impingement mainly occurs when a patient flexes their hip joint past 90 degrees in an internal rotated and adducted position. This then leads to abutment of the femoral neck to the antero-superior and lateral parts of theacetabulum. Clinical signs for the rare postero-superior pathology could be elicited by using a reverse maneuver. The basic radiological investigations for anterior pathology include AP pelvis, cross-table lateral, frog lateral, and Dunn views.
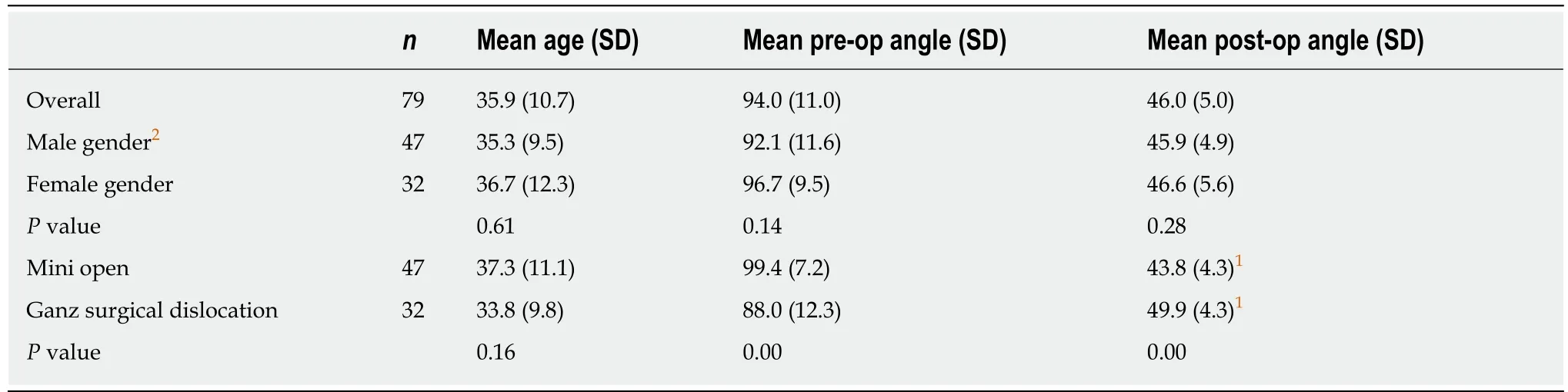
Table 1 Comparison of age and alpha angles for gender and surgery approach
The mean alpha angles range from 42 to 74 degrees between asymptomatic and symptomatic patients[12]. It is worth noting that even in the asymptomatic young population there is a 14 % prevalence of CAM-type morphology when abnormal angle is considered > 50.5 degrees[19]. The significance of this is still largely unknown.Neumannet alidentified impingement free range of motion at an angle with a mean value of 43 degrees (range, 34-60)[11]. They concluded that the value of measurement determined in their study could be considered as a normal limit, which consequently is lower than the currently accepted angle of 50-55 degrees. When surgery is contemplated, the aim is to alleviate patient symptoms and achieve pain free range of motion.
Currently, it is not fully understood if surgical intervention will ultimately prevent progression of osteoarthrosis of the hip joint, however, it is believed that early detection and treatment should mitigate the presumed destructive forces[20]. This notion is supported by many short to mid term reports of good to excellent results regarding the effectiveness of the surgical procedure and possible slowing down of the pathological cartilage destruction process[6,7,11,21-26].
There are many approaches and techniques described for surgical management and more are rapidly evolving. Current review of evidence suggests that all widely used techniques have, at least, comparable mid term results[8,18,22,26-28].
The Ganz surgical hip dislocation for correction of FAI remains the gold standard and has been reported with good results[15,20,22,24]. However, in recent times, there has been an inclination towards more minimally invasive and potentially less morbid procedures such as the anterior mini-open approach which provides ease of access to the joint with lower risks of incidental destruction of the crucial blood supply[7,23].Additionally, it bears mention that as hip arthroscopy continues to evolve,arthroscopic CAM lesion debridement has begun to gain acceptance and popularity[8,20,27,29]. Previous studies with only relatively short-term arthroscopic outcomes data were largely confounded with heterogeneous outcome measures[27].However, more recent studies have shown that patients with FAI undergoing hip arthroscopy experience improvement in pain, quality of life and improvement in function[28,30]. Furthermore, several studies have shown that arthroscopic CAM lesion debridement have a similar functional outcome compared to open surgical approaches[31,32]. Interestingly, to this date no study has shown the correction of the alpha angle in hip arthroscopy, however, a recently published study by Briggset al[33]concluded that while the alpha angle is of importance in preoperative evaluation and diagnosis of FAI, the post operative angle does not correlate with functional outcome or development of osteoarthritis based on patient symptoms.
As for the anterior mini-open approach, there are additional early rehabilitation benefits in comparison to formal hip dislocation as no osteotomies are performed and no hardware is used to re-attach the greater trochanter. At our institution, we used the Ganz surgical hip dislocation approach until early part of the year 2010 and then gradually transitioned to the mini open approach based on good results reported by various studies[7,23]. This transition period, has given us an opportunity to compare our results between the two approaches. By measuring the alpha angle on a plain radiograph, the morphology was closely monitored in the patient’s post-operative follow up period.

Figure 1 A 31-year-old male with bilateral hip femoroacetabular impingement with left hip treated using Ganz surgical hip dislocation while right hip treated through anterior mini-open approach.
We noted that for pre-op measurements, mini open cases had significantly larger alpha angles. Additionally, for post-op measurements, mini-open cases also had significantly smaller angles. So the Ganz surgical hip dislocation did not lead to as large of a change in the alpha angle as compared to the mini-open approach.However, with both approaches we were able to achieve impingement free motion of the hip joint. There were no significant differences in age between the two surgical groups or pre- and post-operative alpha angles based on gender. The overall angle correction achieved by both methods is shown in Table 1. In each case, we achieved alpha angles with impingement-free range of motion.
Using the anterior mini-open approach, when the deformity is in the anterosuperior and antero-lateral part of the head and neck region, the hip is rotated under direct visualization and the bony prominence is shaved with high-speed burr. The labral damage can also be addressed by either debridement or repair. This leads to the assumption that the mini open method should be a more desirable approach.However, it is not without limitations. In the instance of circumferential pathology, it is quite challenging to dislocate the hip and access becomes a limiting factor. On the other hand, the more extensile approach can deal with circumferential pathology in a significantly more desirable manner. Prior studies have reported significant improvement in patient function with no significant risk of avascular necrosis of the femoral head with Ganz surgical hip dislocation[11,15]. However, this approach also carries potential complications. These have been noted to include a bony non-union of the greater trochanter osteotomy site, heterotrophic ossification, and a slow abductor muscle recovery leading to delayed rehabilitation and return to activity.
There are a few limitations to our study. It is a retrospective review of patient records and radiographs. The data would have been more informative if the study was done in a prospective, randomized fashion. Pre-operative magnetic resonance arthrograms were obtained in many of our cases where the pathology was suspicious but the patients had a mixed clinical picture. A combination of radiographs and CT or MRI scans, pre- and post-operatively, could have led to more precise alpha angle measurements and subsequently strengthened the findings. However, this comes at a significantly added cost, radiation exposure, and time factor. Ultimately, it is unlikely that this diagnostic approach would significantly change the findings acquired on plain radiographs which remain a cost-effective and an easily accessible tool for diagnosis of FAI. Lastly, including arthroscopic debridement in our case series would have allowed us to comparatively assess its power of alpha angle correction, however,this approach was not performed at our institution during the data collection phase of this study.
In conclusion, the alpha angle was adequately corrected to the level of impingement free motion with both the anterior mini-open approach and the Ganz surgical hip dislocation. Additionally, the mini-open approach led to an overall greater radiographic improvement.
ARTICLE HIGHLIGHTS
Research background
Femoroacetabular impingement (FAI) is a predisposing factor for secondary osteoarthritis of the hip joint. The two extensively described impingement mechanisms of FAI are CAM and Pincertype deformities. Regardless of predisposing etiology, this abnormal impingement type mechanism leads functional decrease of the patient and to secondary osteoarthritis of the hip joint. Early detection and removal of the asphericity alleviates this mechanical mismatch and oftentimes significantly improves the patient’s symptomatology. Various techniques (i.e.,arthroscopic procedures ranging to more extensive open methods) have been well described in today’s literature and are broadly accepted. This study is significant since it shows statistically significant decreases in alpha angle were noted for both surgical techniques, the Ganz surgical hip dislocation vs anterior mini-open with larger decreases seen in the anterior mini-open group
Research motivation
Ultimately abnormal impingement type mechanisms can lead to symptomatic patients and to secondary osteoarthritis of the hip joint. Early detection and removal of the asphericity alleviates this mechanical mismatch. FAI and successful treatment has become a main focus of todays research focus. There are many surgical approaches to treat FAI. Finding effective surgical management to correct this deformity radiographically and improving functional outcome of the patient remains a challenge and requires further investigation.
Research objectives
The main objectives remains to find a successful way to address deformities of the acetabulum and proximal femur that lead to FAI. For this study the objectives were to evaluate the change from the baseline in the alpha angle on cross-table lateral radiograph after surgery and to compare radiographic corrections between the Ganz surgical hip dislocation and the anterior mini-open approach.
Research methods
This is a retrospective study assessing seventy-nine patients identified in a 5-year period. These patients had preoperative radiographic evidence of FAI and underwent surgery by a single surgeon at our institution, a tertiary care center. Patients with missing radiographic documentation, radiographs with insufficient quality which then precluded accurate measurement of the angle α, a diagnosed congenital condition, isolated Pincer deformity, and history of prior surgery were excluded from the study. Either the Ganz surgical hip dislocation or the anterior mini open approach was used. Postoperative radiographic evaluation of the alpha angle between the two surgical methods was done and corrected for age and gender using twosample t-tests and chi-square analyses.
Research results
Statistically significant decreases in alpha angle were noted for both surgical techniques, with larger decreases seen in the anterior mini-open group. It is not fully understood if surgical intervention will ultimately prevent progression of osteoarthritis of the hip joint, however, it is believed that early detection and treatment should mitigate the presumed destructive forces.This study therefore shows that both surgical approaches provide a valid option for correcting the alpha angle which is implicated in FAI.
Research conclusions
Statistically significant decreases in alpha angle were noted for both surgical techniques, with larger decreases seen in the anterior mini-open group. While we do not know whether there is a difference in functional outcome of the patient, both surgical approaches provide a valid treatment option successfully decrease the alpha angle in patients with FAI.
Research perspectives
It remains difficult to design studies around surgical treatment options and radiographic findings do not necessarily correlate with clinical and functional outcome emphasizing the importance of investigating functional outcome of the patient. Future research should focus on arthroscopic vs open alpha angle reduction for FAI as well as functional outcome and future development of secondary osteoarthritis. Ideally, randomized controlled trials comparing functional outcome and radiographic changes prevspost surgery between arthroscopic vs open treatment vs no treatment would be ideal. However, this study design my not be feasible in the US.
ACKNOWLEDGEMENTS
The authors would like to thank Wojciech L Czoch, MD and Khang Lee, MD for their help in collecting data and editing manuscript.
 World Journal of Orthopedics2020年1期
World Journal of Orthopedics2020年1期
- World Journal of Orthopedics的其它文章
- Double-row repair of rotator cuff tears: Comparing tendon contact area between techniques
- National trends in total hip arthroplasty for traumatic hip fractures:An analysis of a nationwide all-payer database
- Good accuracy of the alpha-defensin lateral flow test for hip periprosthetic joint infection: A pilot study in a retrospective cohort of 52 patients
- Effect of deep transverse friction massage vs stretching on football players’ performance
- Use of three-dimensional printing in preoperative planning in orthopaedic trauma surgery: A systematic review and meta-analysis
- Rapid spontaneous resolution of lumbar ganglion cysts: A case report
