Gastrointestinal discomforts and dietary intake in Chinese urban elders: A cross-sectional study in eight cities of China
Ai Zhao, Mei-Chen Wang, Ignatius Man-Yau Szeto, Li-Ping Meng, Yan Wang, Ting Li, Yu-Mei Zhang
Abstract BACKGROUND Gastrointestinal (GI) discomforts are common in the elderly population; however,whether such discomforts are associated with dietary intake has not been studied.AIM To evaluate GI discomforts in Chinese urban elders and the associated factors.METHODS The gastrointestinal symptom rating scale (GSRS) was used to identify GI discomforts in 688 elders from eight cities of China. The semi-quantitative food frequency questionnaire and one time of 24 h dietary recall were used to access the food intake, identify dietary pattern, and calculate the nutrients intake.RESULTS About 83% of studied elders experienced at least one of GI discomforts in the past 6 mo; dyspepsia was the most commonly reported (66.7%), followed by reflux(44.8%), abdominal pain (35.9%), constipation (35.8%), and diarrhea (34.7%).Female gender, lower education level, and lower family income were associated with a higher GSRS score. Participants who were diagnosed with a GI-related disease had a higher score of constipation, but a lower score of reflux. Chronic diseases were positively associated with certain GI discomforts. Three dietary patterns were identified by the method of principal component analysis, which were characterized as high intake of salt and tea; more frequent intake of tubers,fruits, aquatic products, and soybeans; and high intake of cereal, vegetables, and meat, respectively. However, no associations between dietary patterns and GSRS score were found. The elders with a higher GSRS score had significantly lower intake of bean products. The elders whose GSRS score was ≥ 21 and 18-20 decreased their bean production intake by 7.2 (0.3, 14.3) g/d and 14.3 (1.2, 27.3)g/d, respectively, compared with those who had a GSRS score ≤ 17. There were no differences in other food categories, calories, or nutrients intake among elders with different GSRS scores.CONCLUSION GI discomforts are common in Chinese urban elders. GI discomforts might be associated with the choice of food.
Key words: Gastrointestinal discomforts; Nutrition; Dietary intake; Nutrients; Elderly population
INTRODUCTION
According to the China aging development report (2013), China’s aging population is the largest in the world[1]. By 2016, the number of people aged 60 years and above had reached 230 million-constituting one fifth of the world’s elderly population[2]. In China, the average life expectancy at birth is 76 years old (74 years for men and 79 years for women), which means by 2050, China’s elderly population is expected to reach 400 million[1,2]. The increase in age-related diseases and the consequent rise in health care costs have burdened the society, families, and individuals[3].
Aging is a natural and inevitable biological process, and along with it come a number of physiological, immunological, and cellular changes. One of the most significant changes occurs in the gastrointestinal (GI) tract, which may contribute to increased GI symptoms[4-6]. One recent New Zealand study reported that 20% of elderly participants had lower GI disorders as measured by the gastrointestinal symptom rating scale (GSRS)[7]. Meanwhile, some studies showed that certain GI discomforts, such as constipation, were highly prevalent in the elderly; the prevalence of constipation was over 30% in Chinese elders[8]. Troublesome GI symptoms could be both psychologically and socially debilitating and have a huge impact on frail elderly people[9].
The elderly tend to be more prone to nutritional deficiencies[6]. Multiple agingrelated factors may contribute to malnutrition; these include oral health problems,depression, social activity changes, and GI discomforts[10,11]. One systematic review demonstrated that constipation and general health decline in physical function were risk factors for malnutrition in older people[12]. In addition, age-related changes in GI hormones might influence the regulation of appetite and could contribute to inadequate regulate food intake; however, little research indicates that GI discomforts affect food and nutrients intake[13]. Could GI discomforts limit food choices and lead to impaired nutrient intake? Understanding the effects of GI discomforts on elders’dietary intake is vital to developing dietary solutions that prevent malnutrition.Therefore, the aims of this study were to assess the prevalence of GI discomforts in Chinese elders and explore the potential associations between GI discomforts and dietary intake.
MATERIALS AND METHODS
Ethical considerations
This study was approved by the Medical Ethics Research Board of Peking University(No. IRB00001052-15059) and performed in accordance with the Declaration of Helsinki. Written consent was obtained from the participants before the study began.
Recruitment of participants
This study is a cross-sectional study conducted in eight cities of China from March to July 2016. The strategy used to recruit and enroll subjects has been described in detail elsewhere[14]. A multistage sampling method was used to recruit participants. As a first step, two first-tier cities (Beijing and Guangzhou) and six second- or third-tier cities (Jilin, Xuchang, Wuhu, Chenzhou, Lanzhou, and Chengdu) were selected according to their demographic and socio-economic status. In the second step, we chose two communities in each first-tier city according to their economic status and also chose one community in a non-first-tier city. Based on the resident registration,participants were invited to participate via telephone call by local health workers.Those who had a disability, who had been a resident in the city for less than one year,or who had an infectious disease or mental health problem were excluded. A total of 1739 individuals were eligible and willing to participate in this study; 699 of them were more than 60 years old. Six elders reported that they had severe GI disease (e.g.,cancer, liver cirrhosis, or gastric ulcer) or that they had experienced GI surgery; they were also excluded from the analysis. Participants with gastritis, gallbladder polyp,fatty liver, and chronic diseases were not excluded. The memory and executive screening scale was performed for each elder, and no one was found to have memory problems. Another five elders’ data were not included in the analysis because missing values were found in key questions (i.e., questions related to GI symptoms and dietary intake). In the end, the data for 688 subjects were used in this study.
Data collection
Data were collected from participants by trained interviewers using an intervieweradministered questionnaire. The questionnaire covered four areas: Socialdemographic factors, previously diagnosed illness, GI discomforts, and dietary intake.
For GI discomforts, the validated Chinese version of the GSRS was used to help identify elders with GI discomforts[15]. The questionnaire contains 15 questions on GI symptoms which are grouped into five symptom-clusters: Dyspepsia, diarrhea,abdominal pain, reflux, and constipation. The symptoms in each domain are shown in Supplementary Table 1. Participants were asked to rate the frequency and severity of each symptom experienced in the past half year on a 1 to 4 Likert scale, where 1 is “no or temporary discomfort ”; 2 is “occasional discomfort that lasts for a short time”; 3 is“frequent discomfort that affects daily life”; and 4 is “continuous discomfort that severely affects daily life.” The total GSRS score ranged from 15 to 60. Currently, there is no standardized “cut-off” level for identifying severity of GI discomforts, so we ranked the GSRS score as a continuous variable. A higher score implies more severe GI discomforts.
For dietary intake, the semi-quantitative food frequency questionnaire was used to investigate how frequently food was eaten and how many of 14 food groups were included in meals in the past month. The 14 food groups were taken from the Dietary Guidelines for Chinese Residents 2016 classification, which includes: (1) Cereal; (2)Tubers; (3) Vegetables; (4) Fruits; (5) Meat; (6) Aquatic products (e.g., fish and seafood); (7) Eggs; (8) Bean products; (9) Dairy products; (10) Nuts; (11) Oil; (12) Salt;(13) Tea; and (14) Alcoholic drinks. One time of 24-h dietary recall was used to obtain the data on food intake in the past one day prior to investigation and calculate the energy and nutrient intake based on the Chinese Food Composition Table (second edition) and the nutrient composition table on the food packaging[16]. In the field work, standard bowls, plates, and spoons as well as a standard reference picture book were used to help with quantification of food consumption.
Anthropometric data of height and weight were measured in the field and used to calculate body mass index (BMI). According to China overweight/obesity medical nutrition expert consensus (2016 edition), underweight, normal weight, and overweight are defined as a BMI < 18.5, 18.5-23.9, and ≥ 24, respectively[17].
Statistical analysis
SAS version 9.3 (SAS Institute, Inc., Cary, NC, United States) was used for statisticalanalyses. A normality test was performed prior to the analysis; values are presented as the mean ± standard deviation, median (25th, 75th), or percentage. The independent t-test and analysis of variance were used to compare GSRS scores among participants with different socio-demographic characteristics and health statuses. Dietary patterns were derived from principal component analysis with an orthogonal transformation based on the intake frequencies of 14 food groups. A combined evaluation of eigenvalue (> 1), scree plot, and interpretability of factors determined the number of components. A total of six components had an eigenvalue larger than 1, and we kept three components considering the scree plot and interpretability. Food groups with a factor loading greater than 0.25 were regarded as the food characteristic of the dietary pattern. A factor score was calculated for each individual in each dietary pattern by summing intakes of the 14 food groups weighted by factor loadings. The total GSRS score was tripartited to three groups. Nonparametric test was used to compare the factor loadings of three dietary patterns, food intake amount, and nutrient intake among elders with different GSRS scores. Ordinal logistic regression was carried out to explore the associations of dietary patterns, food intake amount, and nutrient intake with GSRS score, respectively, and to obtain the odds ratio and 95% confidence interval after adjusting for gender, education level, and family income. A Pvalue <0.05 was considered statistically significant.
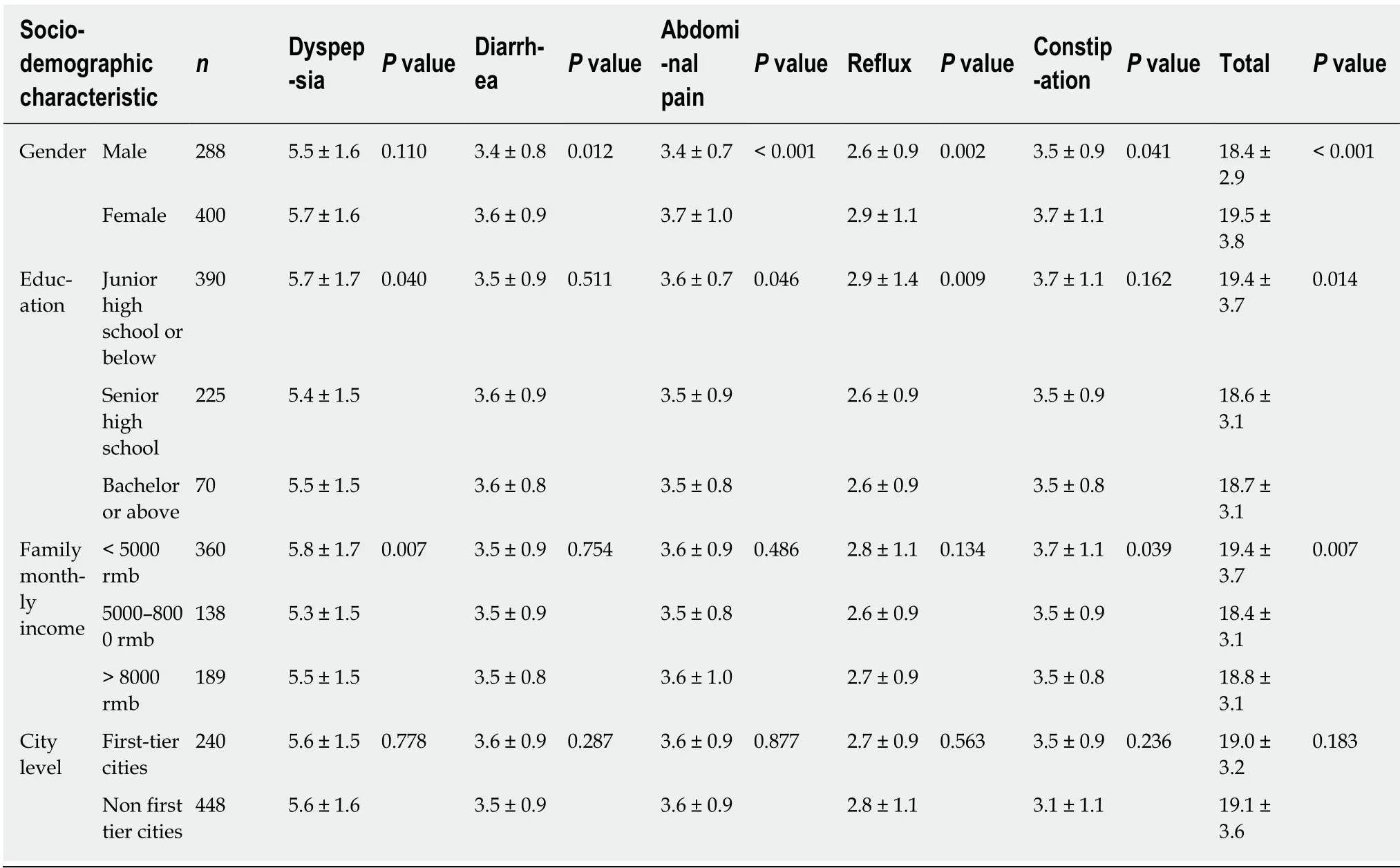
Table 1 Gastrointestinal symptom rating scale scores among Chinese urban elders with different socio-demographic characteristics(mean ± SD)
RESULTS
GI discomforts
There are 688 subjects included in the data analysis; 41.9% were male and 58.1% were female. The mean age of participants was 67.6 ± 4.2 years old and ranged from 60.0 to 81.1 years old. The main ethnicity was Han (97.8%). Over 83% of the participants experienced at least one GI discomfort in the past 6 mo. The mean score of GSRS was 19.0 ± 3.5. The rate of experiencing dyspepsia in the past 6 mo was 66.7%. For diarrhea, it was 34.7%; for abdominal pain, 35.9%; for reflux, 44.8%; and for constipation, 35.8%.
Association of socioeconomic characteristics, demographic characteristics, and health status with GI discomforts
As shown in Table 1, females had a higher total GSRS score and a higher score of all symptoms’ clusters. Participants with a lower education level had a higher total GSRS score and higher scores of dyspepsia, abdominal pain, and reflux. Meanwhile,participants with lower family income had significantly higher total GSRS scores and higher dyspepsia and constipation scores. The total GSRS score and each symptom cluster’s score did not differ significantly between participants who live in the firsttier cities and those who live in non-first tier cities.
Considering health status, which is shown in Table 2, the total GSRS scores and all clusters’ score did not differ among participants with different BMI statuses. The subjects who were previously diagnosed with GI related disease (gastritis, gallbladder polyp, and fatty liver) were more likely to have higher constipation scores, but lower reflux scores. Participants with hypertension scored higher on reflux, while those diagnosed with diabetes had higher constipation scores. The participants with diagnosed dyslipidemia had a significantly higher total GSRS score and higher scores of dyspepsia, diarrhea, abdominal pain, and reflux.
Dietary intake among participants with different GSRS scores
Three dietary patterns were identified by the method of principal component analysis.The first dietary pattern was characterized by high intake of salt and tea. The second pattern was characterized by more frequent intake of tubers, fruits, aquatic products,and soybeans. The last pattern was associated with high intake of cereal, vegetables,and meat. These three diet variables accounted for total 33.5% of the variance in diet.The factor loadings for the first three factors are shown in Supplementary Table 2.Table 3 shows the factor loadings for the three food patterns among participants with different GSRS scores. There were no significant associations between the dietary pattern factor loadings and GSRS score.
The food intake among participants with different GSRS score is shown in Table 4.In single factor analysis, a higher GSRS score was associated with lower meat intake;however, this association disappeared after adjusting for potential confounding variables. In multivariate analysis, the GSRS score was negatively associated with the bean product intake amount. A marginal association was found between dairy product intake and GSRS score (P = 0.052).
Based on participants’ 24-h dietary recall, calories and nutrient intake were calculated. Table 5 shows the calories and nutrient intake among different GSRS score groups. In both the single factor analysis and the multivariate analysis, there were no significant associations between calories or nutrient intake and GSRS scores.
DISCUSSION
This study focused on GI discomforts in the elderly population of China. To the best of our knowledge, this is the first study to describe the associations of GI discomforts with dietary patterns and food and nutrient intake in Chinese elders. The current study revealed that GI discomforts are common in Chinese elders, and it is associated with food intake.
Episode of GI discomforts
The prevalence of some GI discomforts in the aging population is striking[18,19]. We found that 83.3% of the participants experienced at least one episode of the GI discomforts in the past 6 mo; this supports previous findings. For different symptom clusters, dyspepsia was the most common discomfort. However, advanced age has not been identified as a predictor of dyspepsia in previous studies[19]. This difference might be due to how dyspepsia was diagnosed. In previous studies, diagnosed functional dyspepsia or uninvestigated dyspepsia was identified according to the RomeI-III criteria[20,21]. In contrast, our study focused on the symptoms of dyspepsia identified by the GSRS. There are four symptoms (borborygmus, abdominal distension, eructation, and excess gas production) in the cluster of dyspepsia. Excess gas production (45.6%) and eructation (32.4%) were the most frequent symptoms identified among studied elders. It is also worth noting that over one third of the studied population had experienced diarrhea, abdominal pain, reflux, and constipation. These conditions were reported more frequently among elders and have a considerable impact on health expenses and quality of life[22-24].
Predictors associated with GI discomforts
Elderly women had significantly higher GSRS scores than men. This indicates that elderly women have experienced more severe GI discomforts. Similar findings were also reported in studies of dyspepsia, constipation, and reflux[18,20,25,26]. One of the explanations is that menopause-induced hormonal changes may cause increased susceptibility to mucosal injury and may disturb tissue repair in the digestive tract[27].
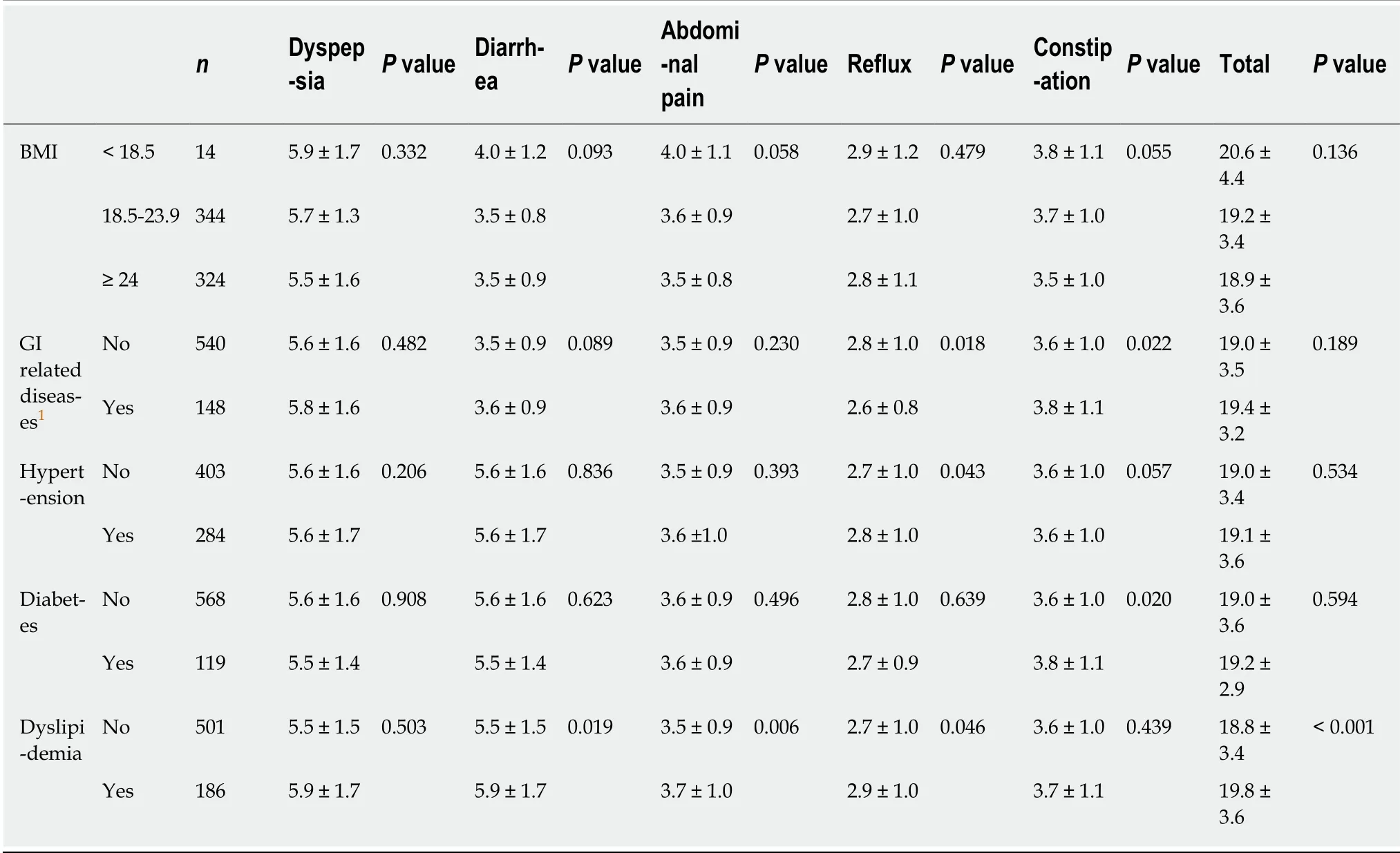
Table 2 Gastrointestinal symptom rating scale scores among Chinese urban elders with different health status (mean ± SD)
Also, previous research indicates that women are more likely to be aware of their health than men[28]. In addition, although men engage in risky health behaviors more often than women do, the socioeconomic gradient tends to be stronger in men than in women[29]. In this study, we also found that lower education level was associated with higher GSRS scores of dyspepsia, abdominal pain, and reflux, while lower family income was associated with higher scores of dyspepsia and constipation.Socioeconomic circumstances shape the motivations and means of individuals to maintain a healthy lifestyle[30]. Socioeconomically-disadvantaged individuals may be less motivated; as a result, they may be more likely to engage in unhealthy behaviors,which in turn results in GI discomforts[31].
In this study, digestive system diseases, including gastritis, gallbladder polyp, and fatty liver were recorded. We found that previously diagnosed digestive system disease contributed to lower reflux scores and higher constipation scores. We suspect that drug therapy and behavior changes used to treat diagnosed digestive system disease might lead to less severe reflux in participants; however, our study did not permit us to establish causality. One review demonstrated that for constipation, nonalcohol-related fatty liver led to an increase in irritable bowel syndrome[32]. In this study, the majority of recorded digestive system diseases were fatty livers. The link between non-alcoholic fatty liver disease and irritable bowel syndrome or constipation should be carefully evaluated in future research.
We found that GI symptoms were associated with chronic disease, especially for dyslipidemia. On the one hand, many drugs used for treating chronic disease (e.g.,antihypertensives, bile acid sequestrants, and biguanides) had side effects on the GI system[33]. On the other hand, chronic disease and GI disorders always share similar risk factors such as low fiber intake, depression, and lack of sufficient physical activity[33,34]. With limited evidence, some studies indicate that chronic disease might lead to certain GI disorders, and conversely, some GI disorders may lead to chronic diseases[33,35].
Dietary intake associated with GI discomforts
Many studies show that dietary habits are closely associated with GI discomforts;however, most studies only focused on constipation, and their results are inconsistent[36]. Few studies have been performed on Chinese elders. One such study conducted in Beijing found that lower intake of staple foods like fish, fruits, and vegetables was associated with constipation; however, in that study confounders werenot taken into account[37]. In our study, we explored the association between dietary patterns and GI discomforts, but found that there were no significant associations.When we considered different types of food, we found that intake of bean products was negatively associated with the severity of GI discomforts. Poor digestion of complex carbohydrates could cause GI discomforts, such as bloating and increased fecal gas production[38]. Twenty percent of carbohydrates in baked beans are malabsorbed[39]. We inferred that participants intended to reduce their bean intake due to uncomfortable GI effects. A marginal negative association was also found between dairy product intake and GI discomforts (P = 0.052). The prevalence of lactose intolerance is high in the Chinese population and increases with age[40]. It should be noted that both bean intake and dairy product intake were extremely low in this sample; in fact, it was far lower than the recommended amount[41]. We assumed that the GI discomforts were more or less associated with food choice in Chinese elders.The potential health risks caused by further reduction in the consumption of bean and dairy products in Chinese elders should be taken into consideration. Since the bean and dairy products are both the high quality source of protein, the insufficient intake of protein might lead to sarcopenia in elders[42].

Table 3 Factor loading of three food patterns among Chinese urban elders with different gastrointestinal symptom rating scale scores (n = 688)
The association between low fiber and low liquid intake and constipation has been confirmed previously; however, there is still a lack of solid data on other nutrients and for other GI discomforts[33]. Some studies with cross-sectional designs reported that reflux was positively associated with calcium, but negatively associated with protein, carbohydrates, and vitamin C intake in the adult population[43]. One study in 2017 reported no significant differences in intake of fermentable oligo-, di-, and monosaccharides as well as polyols (FODMAPs) between elders with and without GI discomforts[7]. Similarly, in this study, no association was found between nutrient intake and GI discomforts. The various food choices in the Chinese diet might contribute to this lack of association, although intake of certain food groups was lower among the participants with GI discomforts. Due to the limitations of this study, we could not determine whether inadequate nutrient intake results in GI discomfort or whether GI discomforts impedes intake of nutrients. Longitudinal studies are highly recommended and should provide a comprehensive dietary strategy for Chinese elders with GI discomforts to ensure healthy aging.
Limitation
As with any case-control studies, the limitations of case-control design are unavoidable and the results should be generalized with caution. Furthermore,although we took into account socio-demographic confounders in this analysis,imprecisely measured or unmeasured factors may have affected our findings, and in turn, the generalizability of our findings. For example, we did not examine the Helicobacter pylori status of participants, which is also prevalent in population and associated with GI disease[44], and this might limit the interpretation of these results.
Another limitation is how we measured dietary intake. We used dietary recall over the past 24 h; this may not adequately capture participants’ daily nutrient intake level,and consequently, may not be suitable for evaluating insufficient or excessive intake of certain nutrients. Since this study focused on elderly population, variation innutrient intake on workdays and holidays was negligible.

Table 4 Dietary intake amount among Chinese urban elders with different gastrointestinal symptom rating scale scores (n = 688)
In addition, the participants being studied were selected from urban areas, which had a higher socio-economic status and usually had more food choices. Results might differ among elders in rural areas. Further studies are needed in different populations.
In conclusion, GI discomforts are common in Chinese urban elders. The GSRS score shows gender, education, and economic differences. Having a chronic disease and having a GI-related disease are associated with GI discomforts. GI discomforts are associated with the choice of food. Participants with GI discomforts have a significantly lower bean intake and marginally lower dairy product intake; however,dietary patterns and nutrient intake are not associated with GI discomforts. Future studies should determine the causality between dietary intake and GI discomforts and provide a comprehensive dietary strategy for Chinese elders.

Table 5 Energy and nutrients intake among Chinese urban elders with different gastrointestinal symptom rating scale scores (n = 688)
ARTICLE HIGHLIGHTS
Research background
China’s aging population is the largest in the world. Gastrointestinal (GI) discomforts are common in the elderly population. GI discomforts may affect the dietary behaviors and contribute to the malnutrition in elders. Likewise, the inappropriate dietary behaviors may cause GI discomforts.
Research motivation
This study was motived by the unknown status of GI discomforts in Chinese elders and its associations with elders’ nutrition. Understanding the effects of GI discomforts on elders’ dietary intake is vital to developing dietary solutions that prevent malnutrition.
Research objectives
The objectives of this study were to assess the prevalence of GI discomforts in Chinese elders and to explore the potential associations between GI discomforts and dietary intake. Based on the potential associations found in this study, future longitudinal studies should further clarify the causality and develop the appropriate dietary recommendation to Chinese elders.
Research methods
With a cross-sectional design, a multi-stages sampling strategy was used in this study to recruit 688 eligible elders from eight cities of China. The gastrointestinal symptom rating scale was used to identify GI discomforts. Dietary pattern, food intake frequencies, average intake amount of 14 food groups, and nutrient intake were evaluated based on the semi-quantitative food intake frequency questionnaire and one time of 24-h dietary recall.
Research results
This study revealed an extremely high incidence of GI discomforts (83%) in elders and dyspepsia was the most commonly reported. The socio-demographic factors were found associated with a higher rate of GI discomforts, including female gender, lower education level, and lower family income. Also, being diagnosed with GI-related disease and chronic disease were related with GI discomforts. We first reported the associations of GI discomforts with dietary patterns and food and nutrient intake in Chinese elders. A significantly lower intake of bean products and a marginally lower dairy product intake were found in elders with GI discomforts. It indicated that the food choice was more or less affected by the GI discomforts. However, the causality could not be determined.
Research conclusions
GI discomforts are common in Chinese urban elders. Female gender, lower education level, and lower family income are associated more sever GI discomforts. Having a chronic disease and having a GI-related disease are associated with GI discomforts. GI discomforts contribute to the choice of food. Participants with GI discomforts have a significantly lower bean intake and marginally lower dairy product intake, which bring potential risk of insufficient protein intake and consequently lead to the reducing of muscle. The results of this study will be helpful for providing a comprehensive dietary strategy for Chinese elders with GI discomforts to ensure healthy aging.
Research perspectives
National-wide studies, including subjects from both rural and urban areas, should be conducted to determine the GI health status in Chinese elders. Longitudinal studies are needed to clarify the causality between dietary intake and GI discomfort.
 World Journal of Gastroenterology2019年45期
World Journal of Gastroenterology2019年45期
- World Journal of Gastroenterology的其它文章
- Imaging findings of inflammatory pseudotumor-like follicular dendritic cell tumors of the liver: Two case reports and literature review
- Prognostic value of risk scoring systems for cirrhotic patients with variceal bleeding
- Irisin attenuates intestinal injury, oxidative and endoplasmic reticulum stress in mice with L-arginine-induced acute pancreatitis
- Toxoplasma ROP16I/III ameliorated inflammatory bowel diseases via inducing M2 phenotype of macrophages
- MicroRNA-760 acts as a tumor suppressor in gastric cancer development via inhibiting G-protein-coupled receptor kinase interacting protein-1 transcription
- LB100 ameliorates nonalcoholic fatty liver disease via the AMPK/Sirt1 pathway
