Targeting MYCN and ALK in resistant and relapsing neuroblastoma
Elizabeth R Tucker,Evon Poon,Louis Chesler
Division of Clinical Studies,The Institute of Cancer Research,Sutton,SM2 5NG,UK.
Abstract
Neuroblastoma,a tumor of peripheral nerve,is the most common solid tumor of young children.In high-risk disease,which comprises approximately half of patients,death from chemotherapy-resistant,metastatic relapse is very frequent.Children who relapse exhibit clonal enrichment of two genomic alterations:high-level amplification of the MYCN oncogene,and kinase domain mutations of the anaplastic lymphoma kinase (ALK) gene.Overall survival in this patient cohort is less than 15% at 3 years,and there are few options for rationally targeted therapy.Neuroblastoma patients exhibit de novo resistance to many existing ALK inhibitors,and no clinical therapeutics to target MYCN have yet been developed.This review outlines the international efforts to uncover mechanisms of oncogenic action that are therapeutically targetable using small-molecule inhibitors.We describe a mechanistic interaction in which ALK upregulates MYCN transcription,and discuss clinical trials emerging to develop transcriptional inhibitors of MYCN,and to identify effective inhibitors of ALK in neuroblastoma patients.
Keywords: Neuroblastoma,anaplastic lymphoma kinase,MYCN,therapeutics
INTRODUCTION
Neuroblastoma is a malignancy of the developing sympathetic nervous system with up to 100 UK children newly diagnosed each year.The risk stratification of neuroblastoma is highly complex and under constant review in order to identify children who may require more aggressive treatment up-front in an effort to prevent relapse,which is almost uniformly fatal.Most recently,a subgroup of ultra-high-risk patients was proposed,based upon age greater than 5 years,high serum lactate dehydrogenase and the involvement of at least one metastatic site,to enable clinicians to pick out these patients at diagnosis for early referral to novel therapeutic trials[1].However,there is also increasingly robust pre-clinical and clinical evidence of molecular subgroups which predict poor outcome,not least the ultra-high-risk patient cohort exhibiting both amplification ofMYCNand kinase domain mutations of anaplastic lymphoma kinase (ALK)[2,3].Herein we discuss the consequences ofMYCNamplification and expression of theALKtyrosine kinase both individually and concomitantly,and highlight the small molecule strategies under investigation to target these aberrations.
NOVEL THERAPEUTIC APPROACHES FOR MYCN-AMPLIFIED NEUROBLASTOMA
Amplification ofMYCNis a defining feature of high-risk neuroblastoma,which when present at diagnosis,predicts a five-year overall survival of only 50%[4].Tumors with amplification ofMYCNare also more likely to exhibit unfavorable histology,diploidy,1p deletion and 17q gain,all of which are associated with poor prognosis.Multi-modality high-risk treatment regimens for these children are contributing to improved outcomes,but it is hoped that clinical implementation of novel targeted therapeutics will have a greater impact for this group of patients.Various strategies to therapeutically down-regulate the activity ofMYCNhave been the subject of multiple preclinical studies,but few of these have progressed to tangible clinical trials[5].The development of MYCN-targeted drugs has been hindered by the complexity and variability of primary MYC structure in solution.As a result,despite being an attractive therapeutic target,there are no clinically available drugs that directly target MYCN.However,many promising approaches to targetMYCNindirectly and its transcriptional output have been developed.These mainly act by blockingMYCNstability,using transcriptional inhibitors or targeting synthetic lethal interactions.
TheMYC-family of oncoproteins are stabilized by altered phosphorylation at the conserved T58 and S62 residues[6].Signaling via the PI3K/Akt pathway in neuroblastoma regulates the phosphorylation of MYCN through GSK3b and mTOR,which makes this pathway a suitable candidate for pharmacological inhibition in order to indirectly target MYCN stability.Preferential sensitivity to inhibitors of PI3K/mTOR,including NVP-BEZ235,were prominently identified in a chemical-genetic screen of isogenic neuroblastoma cells with genetically modified MYCN stabilization versus wild-type MYCN expression[7].NVP-BEZ235 went on to demonstrate growth inhibition of neuroblastoma cells via suppression of MYCN bothin vitroandin vivo.Whilst NVP-BEZ235 is not a clinical candidate compound,the PI3K/mTOR inhibitor SF1126,was taken into pediatric trials for relapsed or refractory neuroblastoma (NCT02337309) (see Table 1 for full summary of targeted inhibitors in clinical studies for neuroblastoma).Recruitment to this study did not meet expectations,but it was the first pediatric study to feature the biomarkers PI3K/AKT/mTOR which can be measured from disseminated tumor cells or platelet-rich plasma[8].The more potent TORC1/TORC2 inhibitor,AZD2014,has also been added to the European Proof-of-Concept therapeutic Stratification Trial of Molecular Anomalies in Relapsed or Refractory Tumors (ESMART,NCT02813135).This trial aims to provide targeted therapy options for pediatric patients with molecular anomalies in their tumors which are not actionable via any other open study for children in Europe.
The control of MYCN expression has been further clarified in recent years.During the cell cycle MYCN stability is directly controlled by Aurora-A which competes with the E3 ligase FBXW7 to prevent the proteosomal degradation of MYCN[9-12].Interestingly,Aurora-A is expressed at an elevated level inMYCN-amplified neuroblastoma[12].We and others have reported that allosteric Aurora-A inhibitors (such as Alisertib and CD532) can dissociate the interaction between Aurora-A and MYCN,resulting in degradation of MYCN and reduced transcriptional output of MYCN[10,11].Following this,two Aurora inhibitors have been clinically evaluated in pediatrics; AT9283 (EudraCT2008-005542-23),an Aurora-A/B inhibitor and Alisertib (NCT02444884,NCT01154816,NCT01601535,NCT01601535),a specific Aurora-Ainhibitor.However both compounds were not well tolerated in pediatric Phase I and II trials[13-17].MYCN status did not improve response and it is unknown whether MYCN is selectively targeted in these tumors.The way remains open for suggestions of alternative or combination studies.For example,it is predicted that the combination targeting of Aurora-A and ATR is beneficial in MYCN-driven tumors,as Aurora-A inhibitors activates ATR[9].

Table 1.Summary of open and completed trials for MYCN or ALK-activated neuroblastomas
Recently,a set of self-regulated master transcription factors known as the “core transcriptional regulatory circuits” have been described to maintainMYCN-amplified neuroblastoma in a state of pro-growth and pro-survival[18].The identification of the key genes involved in maintaining these tumors will allow researchers to focus on finding specific vulnerabilities in the pathways that they control.In addition,indirect approaches to block transcriptional output of MYCN have gained traction with the development of improved genetic and chemical tools targeting various components of the transcriptional machinery that chaperone MYC to target promotors and enhancers.
Inhibition of the bromodomain and extraterminal domain (BET) family has also been shown to downregulateMYCNtranscription inMYCN-amplified neuroblastoma[19].Bromodomain-4 (BRD4),a member of this family,interacts with the positive transcription elongation factor b,and together they are recruited to promoters to phosphorylate RNA polymerase II,particularly at the promoters of genes associated with super-enhancer regions,including MYC[20,21].In an effort to support the progression of BRD4 inhibitors to the pediatric clinic for neuroblastoma,OTX015,an orally-administered compound,was studied in a panel of preclinical neuroblastoma models[22].This molecule was found to have specific activity against MYCN target genes,which correlated with high level MYCN expression andMYCNamplification in a panel of neuroblastoma cell lines.The conclusions from a recent phase I/II study with the BET inhibitor,GSK525762,which allowed for the inclusion of neuroblastoma patients over the age of 16,are awaited (NCT01587703).
Cyclin dependent kinase 7 (CDK7) and cyclin dependent kinase 9 (CDK9) play a key role in the transcriptional cycle of RNA polymerase II.Inhibition of CDK7 or CDK9 selectively kills tumor cells,by targeting the super-enhancer clusters of the genome that are associated with MYCN regulation[23].In the laboratory,many mono-or pan-CDK inhibitors have been reported to display robust anti-tumor effects either by down-regulating MYCN protein or shutting down its transcriptional activity in neuroblastoma (THZ1,CYC065 and dinaciclib) or other cancers (SY-1365,BAY1143572)[24].Although many of them are undergoing clinical evaluation in adults,pediatric trials in neuroblastoma have not yet commenced.
Genetic screens have been used to identify genes that are synthetic lethal toMYCNamplification/overexpression,leading to preclinical evaluation of many new agents in neuroblastoma.One of such agent is CCT244747 following the characterization of synthetic lethal interaction between CHK1 and MYCN[25].Another example is AT7519 following the finding that inactivation of CDK2 is synthetically lethal toMYCNin neuroblastoma cells[26].These new approaches may identify many new targets and agents that are effective in treating neuroblastoma,especially when used in combination with established therapeutics[27].
MYCNamplification and overexpression has also been found in a further small subset of pediatric and adult cancers such as medulloblastoma,retinoblastoma,glioma,lung,pancreas,prostate and hematological cancers.Some effort has been made in the recent years to inhibit MYCN in these tumors,however,most of them were adapted from approaches that have been identified in research conducted originally in neuroblastoma[28].
DIRECT AND COMBINATORIAL THERAPEUTICS FOR ALK-MUTANT NEUROBLASTOMA
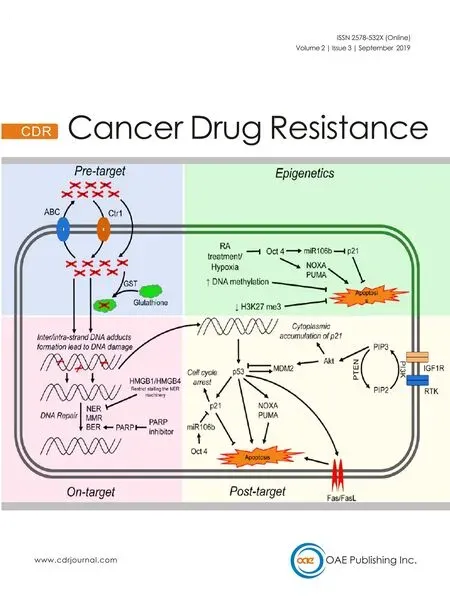
Mutations of the tyrosine kinase ALK were firstly identified in neuroblastoma as the main cause of rare,familial cases of the disease[29,30].In hereditary neuroblastoma,a mutation at the R1275 locus ofALKcan be treated using the first-generation ALK inhibitor,Crizotinib[31].In non-hereditary cases of neuroblastoma somaticALKmutations or amplifications have been shown to be associated with a poor prognosis,for which Crizotinib treatment is often not efficacious[2,30,32,33].ALKmutations are found in around 9% of all neuroblastomas at diagnosis,with the incidence increasing to 14% in the high-risk subtype[2].In contrast to the situation withMYCNamplification,ALK is the first kinase identified as a driver in neuroblastoma with real potential as a tractable therapeutic target,due to the number of inhibitors already available.IfMYCNamplification and anALKmutation are found concomitantly,this is associated with an ultra-highrisk molecular phenotype[3].Constitutive activity of ALK,which activates signaling via PI3K/Akt,MAPK,ERK5 and JAK/STAT,leads to the transcriptional up-regulation ofMYCNand MYCN protein stabilization,thus compounding the aggressive nature of this cohort of tumors[34-36][Figure 1].
The availability of later-generation ALK-targeted therapeutics has led to a unique situation for pediatric neuroblastoma patients.There are now open trials for pediatric patients with either Ceritinib or Lorlatinib.
Ceritinib,which received USA Food and Drug Administration approval in 2014 for treatment of patients withALK-rearranged metastatic non-small cell lung cancer (NSCLC),has shown efficacy above that of Crizotinib in neuroblastoma models[37].However,its success in neuroblastoma patients is yet not fully evaluated,apart from a favorable case report for a tumor harboring anALKI1171T mutation[38].I1171T is a gain-of functionALKmutation,located in the neuroblastoma mutation hotspot of ALK,at the αC-helix in the amino-terminal lobe of the kinase.The most common neuroblastoma-associated mutations at this hotspot are F1174,R1275 and F1274,each with different degrees of transforming ability and differential sensitivities to available inhibitors[2,39].A screen of known neuroblastoma-associatedALKmutations utilizing recombinant ALK variants,revealed that response to crizotinib correlated with a relatively reduced affinity of the mutant kinase for ATP.For example,ALKF1174L results in higher ATP-binding affinity,predicting resistance to crizotinib[2].Much attention has been upon the potential of the thirdgeneration ALK inhibitor,Lorlatinib,for which exceptional preclinical evidence of its efficacy against the Crizotinib-resistant ALK F1174L has been published[40,41].Lorlatinib was initially developed for NSCLC patients requiring targeted therapy against ALK for brain tumor metastases,as it has good Central nervous system (CNS) availability[42].This could become a necessity for children with neuroblastoma,as relapses within the CNS may become more frequent following the introduction of immunotherapy into standard therapy.Based on this evidence,Lorlatinib is now available in an international study for children with relapsedALKmutant neuroblastoma.Other ALK inhibitors demonstrating good preclinical rationale for neuroblastoma include Alectinib and Entrectinib[43,44].Alectinib shows activity against RET,a downstream target of ALK in neuroblastoma,which may increase its effectiveness in this form of the disease[45].Entrectinib inhibits both ALK and the TRK receptors; TRKb is associated with poor prognosis in neuroblastoma.Both these compounds are therefore a priority for further pediatric studies.
Although the standard route for the evaluation of novel compounds is through early phase clinical studies in relapsing or treatment-refractory disease,there is strong preclinical rationale for the combination of ALK inhibition with up-front chemotherapy inALK-positive neuroblastoma patients.Krytskaet al.[46]demonstrated that neuroblastomaALKcell lines withde novoresistance to Crizotinib,achieved complete responses to Crizotinib combined with chemotherapy in xenograft models.This synergy was dependent upon a functional p53 pathway,further making the case for targeted therapy upfront in treatment schedules,as p53 pathway in-activation is a characteristic of chemotherapy-resistant disease[47].The phase II pediatric study,PEDS-PLAN,is currently evaluating feasibility of molecularly guided therapy in combination with induction chemotherapy (NCT02559778).Additionally,Crizotinib is being tested against Iobenguane I-131 with standard therapy for children newly diagnosed with high-risk neuroblastoma or ganglioneuroblastoma (NCT03126916).
InALK-rearranged NSCLC,there is a strong precedent for the transition of patients between different ALK inhibitors,as a common mechanism of resistance in this patient group is the acquisition of a secondary treatment-inducedALKmutation[48].It has even been reported that re-challenge with a previously used ALK inhibitor can be effective,if compoundALKmutations occur with different inhibitor sensitivities[49].In neuroblastoma,the picture of acquired resistance to ALK inhibitors may be very different.Upregulation of signaling through the alternative tyrosine kinase AXL,associated with an increase in endothelial-tomesenchymal transition,has been proposed in response to induced resistance to the non-clinical ALK inhibitor TAE684,in vitro[50].A more recent study of induced Lorlatinib resistancein vitropin-pointed an acquired mutation ofNF1with RAS/MAPK activation[51].
In fact,the dominance of the RAS/MAPK pathway in refractory and relapsing neuroblastoma is becoming clear.Relapsed high-risk neuroblastoma has a higher mutational burden than neuroblastomas at diagnosis,and the largest study of this type has shown that over half of the mutations identified at relapse are targetable by compounds already in clinical development[52].This study also concurred with evidence of the preponderance of RAS/MAPK pathway mutations at relapse published previously[53-55].For example,Eleveldet al.[54]carried out a whole genome sequencing paired study of 23 diagnostic and relapsing neuroblastomas,finding that 18 out of 23 relapse samples had acquired mutations predicted to hyperactivate the RAS/MAPK pathway.Included in this relapse group were 10 mutations ofALK,strongly suggesting that the incidence ofALKmutations at relapse is higher than at diagnosis.Re-sequencing of tumors in relapsing patients is therefore essential,due to the availability of ALK inhibitors,amongst others.However,the application of MEK inhibitors to treatALK-activated neuroblastomas is not straightforward.As demonstrated in a recent preclinical study,MEK/ERK inhibition in this context results in the increased activation of AKT-ERK5 and therefore does not slow neuroblastoma growth[56].The complexity of the signaling,and escape-signaling pathways involved in neuroblastomas treated with targeted inhibitors underlines the need for a personalized medicine approach to treat these patients.
In anticipation of resistance to ALK inhibition and in order to improve the best response for patients withALKmutant neuroblastoma,combination clinical studies are already underway.The NEPENTHE (Next Generation Personalized Neuroblastoma Therapy,NCT02780128) study is designed to match genomic aberrations found at neuroblastoma relapse with the optimal combination of small molecule targeted treatment.ALK-positive patients enrolled onto this study will receive a combination of Ceritinib with the CDK 4/6 inhibitor,Ribociclib.This combination demonstrated strong evidence of synergy in preclinical work,using bothin vitroexperiments to study the effect of the combination on the relevant cyclin D/CDK4/CDK6/RB and ALK signaling pathways,andin vivotrials with conventional and patient-derived xenograft models[57].The precise mechanism of interaction between these two compounds is not fully characterized,except that when dosed together inALKmutant cell lines,there was enhanced depletion of both phosphorylated ALK and phosphorylated Rb,compared to either agent alone.
THE RELATIONSHIP BETWEEN ALK AND MYCN EXPRESSION AND ITS INFLUENCE ON THE DESIGN OF THERAPEUTIC APPROACHES
The mechanism underpinning the relationship between ALK and MYCN is being gradually further characterized,and it is known that ALK stabilizes MYCN protein via the PI3K-Akt pathway[34,58].This strengthens the rationale for the current clinical study of Crizotinib combined with Temsirolimus for patients withALKmutant neuroblastoma.One of the primary objectives of this study is to determine the Phase 2 dose of Crizotinib and Temsirolimus in the setting of relapsed or refractory neuroblastoma with mutations of eitherALKor MET,as the tyrosine kinase MET is an additional target of Crizotinib.In addition to this the activity of Crizotinib will be recorded alongside pharmacodynamic analysis of biomarkers for PI3K/AKT/mTOR in platelet rich plasma samples and paired tumor samples collected through the course of treatment (ITCC053).
Both wild type ALK and ALK mutant species are able to stimulate the transcription ofMYCNin neuroblastoma and neuronal cell lines[59].Most recently the transcriptional mediator between ALK andMYCNhas been identified as “HMG-box transcription factor 1” (HBP1)[60].HBP1 was previously identified as a negative regulator of MYCN activity[61],and also as a component of theALK-77gene signature described by Lambertzet al.[45].Further to this,it is now determined that mutant ALK negatively regulates HBP1 through the PI3K-Akt-Foxo3a signaling axis,allowing specific discussion of further targeted combination therapies which should be investigated with a view to disrupting this pathway to the benefit of these ultra-high-risk neuroblastoma patients.To this end,preclinical evidence of synergy has already been presented for several combinations,including the PI3K inhibitor NVP-BEZ235 with the BETBromodomain inhibitor,JQ1,allowing for upregulation of HBP1 and suppression ofMYCNtranscription simultaneously.
Whilst it is generally acknowledged that combination therapy will be required to see durable clinical responses,the difficulties associated with moving preclinical combinations to the clinic have led researchers to investigate the potential of dual inhibitors for high-risk patient populations.In particular,the Pololike kinase 1 (PLK-1) inhibitor BI-2536,which already had low-nanomolar IC50activity against BRD4,has been re-designed to have additional activity against mutant ALK F1174L[62].Through a series of chemical modifications to the structure,an initial set of dual inhibitors has been created,which retain their activity against BRD4,reduce their specificity for PLK-1 and increase their activity and selectivity for the mutant ALK ATP-binding pocket.Rationalizing further these compounds within thein vivopreclinical setting,using a panel of validated neuroblastoma models,will provide a compelling case for these compounds to progress into clinical studies.
CONCLUSION
Finding a targeted therapy for MYC-activated tumors,including neuroblastoma,has provided an insurmountable challenge for cancer researchers for many years.However,as more is understood about the transcriptional control of MYC expression,within the context of our greater appreciation of the global control of gene expression,it is now highly likely that selective compounds will make their way from bench to bedside.The opportunity to manipulate ALK activity in neuroblastomas is complicated by the specificity of individual ALK mutants for available compounds.However,the progression towards innovative trial designs incorporating personalized genomic medicine and pharmacodynamic markers will undoubtedly improve the translational outcomes.
DECLARATIONS
Authors' contributions
Manuscript writing:Tucker ER,Poon E
Supervised the work:Chesler L
Availability of data and materials
Not applicable.
Financial support and sponsorship
The authors are supported by a programme grant from Cancer Research UK (C34648/A18339 and C34648/A14610).
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2019.
- Cancer Drug Resistance的其它文章
- Enhanced Kat3A/Catenin transcription:a common mechanism of therapeutic resistance
- Longitudinal monitoring for the emergence of epidermal growth factor C797S resistance mutations in non-small cell lung cancer using blood-based droplet digital PCR
- Regulation of ABCB1 activity by microRNA-200c and microRNA-203a in breast cancer cells:the quest for microRNAs' involvement in cancer drug resistance
- MicroRNA-126 and epidermal growth factor-like domain 7 predict recurrence in patients with colon cancer treated with neoadjuvant chemotherapy
- Genetic variations in triple-negative breast cancers undergoing neo-adjuvant chemotherapy
- Use of MRl,metabolomic,and genomic biomarkers to identify mechanisms of chemoresistance in glioma