Relations of change in fruit and vegetable intake with overall energy reduction and physical activity with weight change:Assessing theory-based psychosocial mediators James J.Annesia,b
a
b Young Men’s Christian Association of Metro Atlanta,Atlanta,GA 30303,USA
Abstract Background: Increased physical activity and fruit and vegetable (FV) intake are typically suggested to counter obesity. Sustained behavior change in those areas has, however, been poor, possibly because of a lack of understanding of the effects of psychosocial factors. Using data from previous research, this study aimed to better define the role of physical activity and FV intake in short- and long-term weight loss via changes in malleable psychosocial mediators and moderators.Methods:Women who were obese(n=183;age=50.0±7.9 years;body mass index=35.2±3.2 kg/m2,mean±SD)and who previously participated in 3 different community-based behavioral weight-loss treatments were assessed over 2 years.Changes in FV intake,physical activity,self-regulation of physical activity and eating(aggregated),negative mood,and weight were measured over 6 and 24 months.Results:Changes in each variable over both 6 and 24 months were significant(all p values <0.001).The FV intake to the weight-related caloric intake relationship(β=-0.30,p <0.001)was significantly mediated by self-regulation change over 6 months.The physical activity to weightchange relationship(β=-0.46,p <0.001)was significantly mediated by both self-regulation and mood change over 24 months.Physical activity,itself,accounted for only 16%of weight-related caloric expenditure differences.Changes in physical activity and FV intake were each independent predictors of weight change over 24 months(overall R2=0.50,p <0.001).Conclusion:Findings clarified theory-based targets for weight-management treatments and suggested that future weight-loss treatments strongly focus on developing self-regulatory skills to address barriers to behavioral changes.2095-2546/© 2019 Published by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license.(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Keywords: Fruit and vegetable;Obesity;Physical activity;Psychosocial;Weight loss
1. Introduction
The obesity epidemic is increasing internationally and has become a major public health issue.1In the United States,women of ages 40-59 years have an obesity rate of approximately 40%.2Behavioral (nonsurgical and nonpharmacological) treatments have typically been ineffective beyond the short term.3,4Within weight-loss treatments,physical activity(PA)is typically assigned for energy-expenditure purposes.Although PA is strongly associated with sustained weight loss,5,6concomitant energy outputs are minimal in deconditioned individuals.7Although fruit and vegetable(FV)consumption has been considered a predictor of overall diet quality and energy intake,8most treatments address numerous nutritional factors that might confuse,and actually be detrimental to,appropriate eating behaviors.9
Effects of self-regulation and mood, although not addressing the full scope of Bandura’s social cognitive theory,10are vital aspects of the broad and well-accepted paradigm of human actions that might be associated with successful weight-loss behaviors such as PA and improved eating.11Selfregulation refers to“processes responsible for guiding individuals’ behavior toward goals or other standards”.12Bandura indicated that self-regulation plays a key role in individuals’ability to successfully control their environments, especially when confronted with barriers.13,14For example, it was suggested that the aforementioned association between FV consumption and overall energy intake8might be mediated by one’s ability to use self-regulation strategies.11Within the present research, mood refers to an aggregation of feelings such as anxiety, depression, fatigue, and vigor. Social cognitive theory suggests moods and feelings that are pleasant or aversive can serve as “incentives” and “disincentives”, and accordingly,influence behaviors.15Although there are theories that uniquely target the effects of self-regulation (e.g., temporal self-regulation theory16) and mood (e.g., mood-behavior model17),the advantage of social cognitive theory is in its ability to provide both “predictive and operative tools”13useful with multimodal interventions such as those incorporated within this research.Thus,methods as diverse as goal setting,recruiting social supports, self-regulating internal talk, selfregulating behavioral cues and prompts, and mood regulation can be homogeneously assimilated within a single theory.
Even minimal amounts of PA (i.e., about 3 moderate sessions/week)have been shown to benefit mood,self-regulation,and their interactions.18Thus, weight reductions associated with PA and targeted dietary changes might occur through(i.e., be mediated by) associated psychosocial improvements during both phases of weight loss (typically about 6 months after initiating treatment3,6,19), and through weight-loss maintenance/regain (typically assessed 12-24 months after treatment initiation and beyond3,6,19).Theory is less clear whether mood change would be best tested as an additional mediator(along with self-regulation) of the long-term relationship of PA and weight change or as a moderator potentially affecting relationship between PA and self-regulation change.13For example, changes in mood are proposed to affect (moderate)the development and use of self-regulatory processes.20Although the importance of a richer understanding of the proposed relationships has been suggested on both theoretical13and applied12levels,there was a lack of interest in decomposing treatment effects to understand psychosocial correlates’role in associated behavioral effects.20,21
It has been proposed that because mechanisms at work during weight loss and through the period of expected regain might be different, separate analyses are warranted.3Because there might be sex-specific implications related to psychosocial factors within behavioral weight-management interventions, research has supported accounting for effects associated with women and men separately.8,11The aim of this research was to provide an improved understanding of the proposed relationships to more precisely target treatment processes and improve effects within large-scale, community-based interventions that have, so far, remained overwhelming ineffective.3,4,22
Thus,the present research with women who previously participated in 3 community obesity interventions was conducted to inform both weight-loss theory and treatment. The following hypotheses addressing both the weight loss and weightloss maintenance phases were given:
(1) Over both 6 and 24 months from baseline, there will be significant treatment-associated improvements in FV intake, PA, self-regulation for weight-loss behaviors,mood,and weight.
(2) During the weight-loss phase (baseline-Month 6), the caloric-intake change associated with each participant’s initial weight change will be significantly predicted by change in FV intake. Change in self-regulation will significantly mediate this relationship.
(3) Through the weight-loss maintenance phase (baseline-Month 24), weight change will be significantly predicted by change in PA. Change in self-regulation and mood will significantly mediate that relationship.When instead entered as a moderator, mood change will moderate the change in PA and self-regulation relationship.
(4) Only a small percentage of observed weight change(≤20%) will be attributable to PA-associated caloric expenditures.
2. Methods
2.1. Participants
Data were extracted from previous research on communitybased behavioral treatments focused on personal characteristics and weight change.23,24This research was conducted in the southeastern United States, where women volunteered to participate in methods designed to support healthy changes in eating and PA behaviors. Inclusion criteria were: age≥21 years, body mass index (BMI) 30-40 kg/m2, no present psychotropic medication use, and no present or soon-planned pregnancy. The overall age of the sample (n=183) was 50.0± 7.9 years, BMI of 35.2 ± 3.2 kg/m2, middle-class median income range of USD50,000-USD100,000/year, and an educational level of 31% high school, 36% college degree, and 33% beyond college. Kennesaw State University Institutional Review Board (IRB) approval was received, and a signed informed consent form that was approved by the IRB was obtained from all participants.Principles of the Helsinki Declaration were followed throughout.
2.2. Measures
The number of typical daily servings of FV, recalled over the previous month,was summed using a brief self-report survey. Serving sizes (e.g., 118 mL fruit juice, 118 mL carrots)were indicated by U.S. governmental sources.25,26The survey demonstrated significant correspondences(β=0.45-0.83,p <0.001) with comprehensive food frequency recall instruments27,28and weight change.29Test-retest reliabilities over 2 weeks were 0.77-0.83.26
The number of PA sessions (≥15 min) over the last week was recalled using the Leisure-Time Physical Activity Questionnaire.30Activity types corresponded to metabolic equivalents (METs)—a measure of energy expenditure(MET)31=(mL O2/kg/min)—ranging from 3 METs(e.g.,easy walking) to 9 METs (e.g., running), and were summed.30,32The Leisure-Time Physical Activity Questionnaire significantly corresponded to accelerometer, weight change, and VO2maxresults (β=0.38-0.57, p <0.001).33,34Test-retest reliability over 2 weeks was 0.74.30
To assess overall use of self-regulation skills applied to weight-management behaviors, responses to 10 items each(scored 1=never to 5=often) focused on PA self-regulation(e.g., “I set physical activity goals”) and eating self-regulation(e.g., “I keep a record of my eating”) were summed.The scale was based on an earlier validated instrument35that was previously adapted to address the self-regulatory skills used in cognitive-behavioral treatments.36In preliminary research, there was considerable cross-loading of the PA and eating item responses that justified use of the present version of an aggregated measure of self-regulatory skills use for weight-loss behaviors, overall.Internal consistencies were Cronbach α=0.79-0.80.36Test-retest reliabilities over 2 weeks ranged from 0.74 to 0.78.36Within the present research,the Cronbach α value was 0.77.
To assess overall negative mood, responses (scored 0=not at all to 4=extremely) to the 30 items of the Profile of Mood States Short Version37related to factors of tension (e.g.,“uneasy”), depression (e.g., “sad”), fatigue (e.g., “worn out”),anger (e.g., “angry”), and confusion (e.g., “forgetful”) were first summed,and then the vigor(e.g.,“energetic”)factor score was subtracted.This yielded a possible overall negative mood score range of-20 to 100.Internal consistencies across factors were Cronbach α values=0.84-0.95.37Test-retest reliability over 2 weeks was 0.69.37Cronbach α values ranged from 0.79 to 0.87 for the present data.
Participants’ weight was measured in kg using a recently calibrated digital scale. The mean of 2 consecutive measurements was recorded after removal of heavy outer-clothing.
2.3. Procedures
Staff from community-based wellness centers administered the weight-loss treatments, each with its bases in tenets of social cognitive theory.10Although each treatment focused on building self-regulatory skills and managing mood and emotional eating,3 distinct formats were used:(a)manual-based,38with phone follow-ups over 6 months, (b) biweekly group meetings (14 months),24and(c) biweekly group meetings (14 months) followed by 6 brief monthly phone follow-ups.24Based on Abraham and Michie’s39taxonomy of behavior change techniques, the treatments each emphasized goal setting and regular reviews of goal progress, barrier identification, relapse prevention, controlling self-talk, stress management, time management, and recruiting social supports.Each treatment format indicated to participants the benefits and importance of increasing PA in forms that were individually acceptable to them and in amounts that could be well tolerated.
Measurements were taken in private areas at baseline,Month 6,and Month 24.Structured fidelity checks were completed on approximately 15%of sessions.Several minor issues with protocol compliance were easily remedied.
2.4. Data analyses
An intention-to-treat design was employed,and the 12%of missing data were imputed through the expectation-maximization algorithm under the assumption of missing at random.For the primary regression analyses, a sample size of 160 was required to detect a small-to-moderate effect of f2= 0.08 at the power level of 0.90 (α <0.05).40Statistical significance was set at α <0.05 throughout,with the Bonferroni correction applied for multiple tests.
Data from the 3 treatment formats were merged for analyses. Repeated measures analysis of variance (ANOVA) were first calculated to assess changes in FV intake,PA,self-regulation, negative mood, and weight. Follow up t tests assessed changes from baseline to Month 6 and baseline to Month 24,with effect sizes (0.20=small, 0.80=large) calculated as Cohen’s d(meantime2-meantime1/SDtime1).
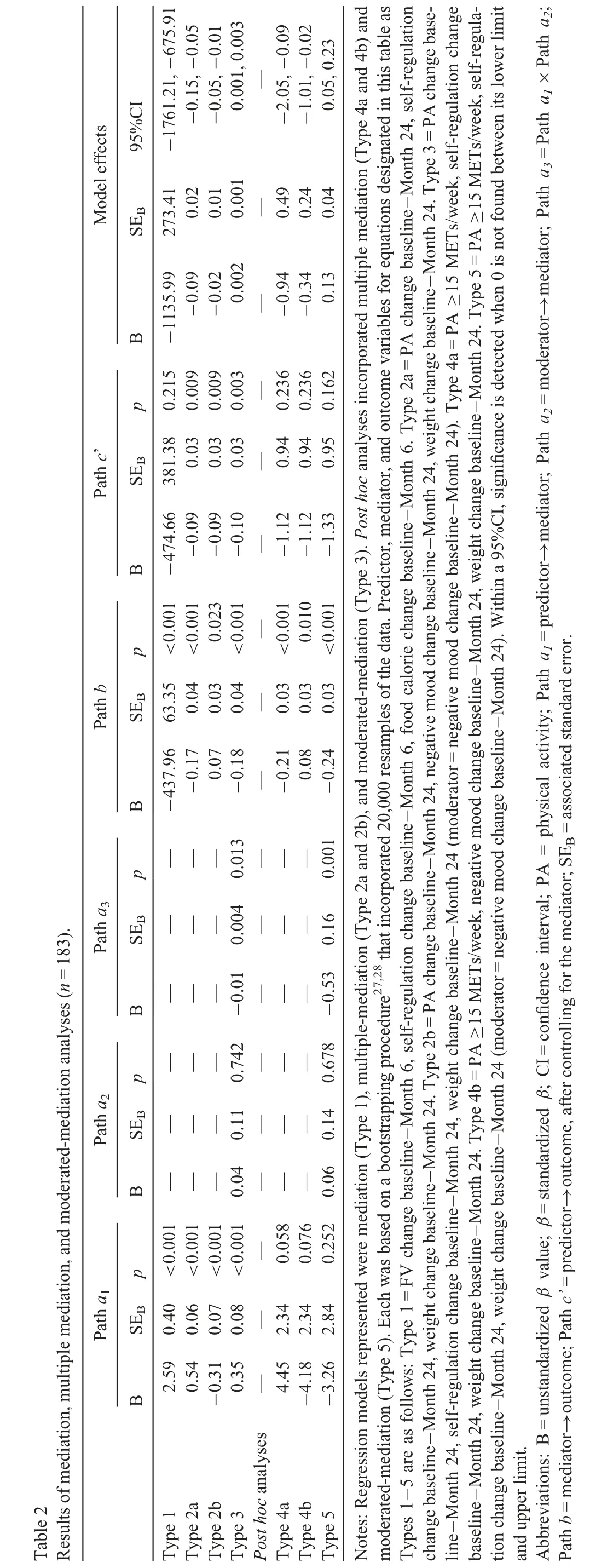
In the regression model results, the unstandardized beta value(B),its associated standard error(SEB),and standardized beta value (β) is reported. A bias-corrected and accelerated bootstrapping method incorporating 20,000 resamples was used in the mediation,41multiple-mediation,41and moderatedmediation42analyses. Specifically assessed variables in the regression equations were: (a) the mediation of the prediction of caloric intake by FV intake through self-regulation change over 6 months, (b) the mediation of the prediction of weight change by change in PA through self-regulation and mood change over 24 months, and (c) mood change instead entered as a moderator in the preceding equation (where self-regulation change was the mediator). Because no significant effects on the assessed relationships were found based on group participation within preliminary analyses, no covariates were entered into those regression analyses. Fig. 1 is given as a guide to the(A)mediation and(B)moderated-mediation models incorporated. Significant mediation is detected when 0 is not found between the lower-and upper-limit of a 95%confidence interval.
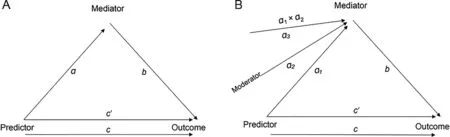
Fig.1. Diagrams of mediation(A)and moderated-mediation(B)models incorporated.
Accepted formulas for energy expenditure(METs×kg×time (h)),43weight loss (a reduction of 7700 kcal yields a reduction in weight of 1 kg),44and percentage of weight change from PA (change in weight from PA/change in weight overall) were applied. Analyses were conducted using SPSS Statistics Version 22.0(IBM Corp.,Armonk,NY,USA).
3. Results
3.1. Score changes
Repeated-measure ANOVAs indicated significant overall improvements, and all planned follow-up dependent t tests also demonstrated significant improvements in FV intake,PA,self-regulation,negative mood,and weight over both 6 and 24 months(Table 1).
3.2. Effects of FV intake
The caloric-intake change associated with the observed weight change over 6 months was significantly predicted by 6-month change in FV intake (B=-1610.65, SEB= 386.11,β=-0.30, p <0.001). However, the FV change-caloric change relationship was no longer significant after change in self-regulation was entered as the mediator (model R2=0.28,p <0.001;Table 2,Type 1).
3.3. Effects of PA
In a bivariate analysis, weight change over 24 months was significantly predicted by change in PA(B=-0.20,SEB=0.03,β=-0.46, p <0.001). In a separate equation, change in both self-regulation and mood uniquely mediated that relationship at the accepted level of significance(model R2=0.33,p <0.001;Table 2, Type 2a/2b). When entered instead as a moderator,change in mood significantly moderated the PA-self-regulation change relationship (model R2=0.31, p <0.001; Table 2,Type 3).Of the observed weight change,only 16%was attributable to caloric expenditures.
3.4. Post hoc analyses
In post hoc tests where the completion of a mean of≥15 METs/week of PA (~3 moderate sessions/week) (coded 0=no, 1=yes) was entered in place of PA change, the linear bivariate relationship (B=-2.40, SEB= 1.09, β=-0.16,p=0.029) and results of the multiple-mediation and moderated-mediation equations, were similar (Table 2, Type 4a/4b and Type 5).
Both changes in FV intake (B=-1.66, SEB=0.53,β=-0.22, p=0.002) and PA (B=-0.35, SEB=0.07,β=-0.36,p <0.001)significantly contributed to the prediction of weight change over 24 months(model R2=0.50,p <0.001).
4. Discussion
The results clarified the foci for community-based weightmanagement interventions. Based on the significant association between changes in FV intake and overall kcal intake(mediated by self-regulation change), FV consumption was supported as a proxy for the overall diet, and thus should be specifically emphasized.Based on an even more robust association,PA(even as minimal as 3 sessions/week)was upheld as a strong predictor of longer-term(i.e.,2 years)weight loss.Its direct impact on overall kcal expenditure was,however,minimal. Indirect effects of the PA-weight-loss relationship through the psychosocial variables of self-regulation and improved mood were substantiated. Thus, attention to moderate PA is also warranted for reasons well beyond its associated energy expenditures.Additional research is required to further clarify psychosocial mechanisms.
Most behavioral weight-loss treatments seek to inform individuals of a plethora of(often extraneous)nutritional details.9They have had especially poor effects.4PA and exercise is often incorporated in a haphazard, “more is better” manner without purposefully leveraging its proven psychological benefits.45This can overtax individuals into poor adherence,46andthus, might not be optimal for maximizing effects. Additionally, although suggested by theory and previous research,10,13,29treatments generally fail to sufficiently focus on overcoming behavioral barriers through self-regulatory skills use or leveraging PA-associated change in mood to reduce emotion-based overeating. Although further analyses of advantages of such intervention foci are required, the present results suggest their efficacy as treatment bases.
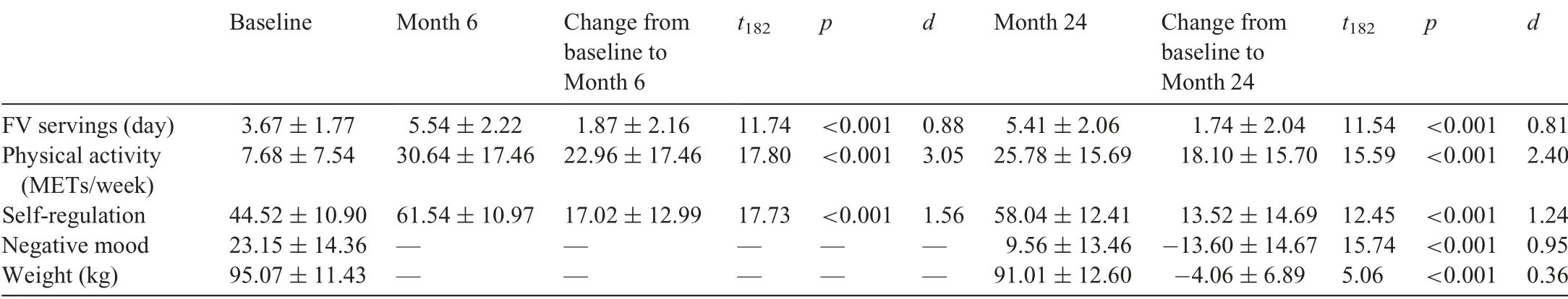
Table 1 Changes in study variables(n=183)(mean±SD).
Limitations within this research include a lack of control over influences based on instructors’personal styles and possible expectation effects associated with the modality and length of the different treatment formats. Other key aspects of social cognitive theory(e.g.,self-efficacy)and their interactions with the present psychosocial constructs require testing in extensions of this research. Although additional limitations include the use of a specific sample of women volunteers, possible social support effects(e.g.,from fellow participants)that could have biased survey responses, and a need for replications and extensions to increase confidence in findings,clear weight-loss treatment targets applicable for large-scale dissemination were suggested. Thus, the present research serves to bridge theory and application,as previously noted,47to advance the development of effective weight-management treatment architectures.
5. Conclusion
The present findings suggest an evidence-based retort to commonly used approaches by targeting and supporting (a)primarily FV intake (because of its association with the adequacy of the overall diet and energy intake), (b) manageable but consistent PA (because of its association with improved mood, self-regulation, and long-term weight loss), and (c)development of self-regulatory skills(to strengthen behavioral changes and overcome barriers). They contributed to the emerging yet inconclusive body of research on psychosocial correlates of weight-management behaviors over the short and long term.11,29
Acknowledgment
This study was funded in part by the Thrivent Foundation Let’s Get Healthy grant.
Competing interests
The author declares that he has no competing interests.
 Journal of Sport and Health Science2019年4期
Journal of Sport and Health Science2019年4期
- Journal of Sport and Health Science的其它文章
- Journal of Sport and Health Science Guide for Authors
- Standardization of exercise intensity and consideration of a dose-response is essential.Commentary on“Exercise-linked FNDC5/irisin rescues synaptic plasticity and memory defects in Alzheimer’s models”,by Lourenco et al.,published 2019 in Nature Medicine
- Could sport be part of pediatric obesity prevention and treatment?Expert conclusions from the 28th European Childhood Obesity Group Congress
- Editorial re:Could sport be part.....by Ring-Dimitriou et al.
- Exercise,cognitive function,and the brain:Advancing our understanding of complex relationships
- Author biographies
