Clinical characteristics and surgical treatment of schwannomas of the esophagus and stomach:A case series and systematic review
Jesús Morales-Maza,Francisco Ulises Pastor-Sifuentes,Germán E Sánchez-Morales,Emilio Sanchez-Garcia Ramos,Oscar Santes,Uriel Clemente-Gutiérrez,Adriana Simoneta Pimienta-Ibarra,Heriberto Medina-Franco
Abstract
Key words: Schwannoma;Esophagus;Stomach;Surgery;Systematic review
INTRODUCTION
Gastrointestinal schwannomas are slow-growing benign mesenchymal neoplasms that originate from Schwann cells.The most frequent locations are the stomach and colon,with the esophagus being the least frequent site.
Despite being tumors widely known by clinicians,gastrointestinal schwannomas are rare.It is accepted that the treatment of choice is laparoscopic or open resection,where in wedge,subtotal or total gastrectomy can be performed.
We present an institutional case series,and a systematic review of esophagic and gastric schwannomas.The aim of this study is to review the available literature about gastrointestinal schwannomas;especially lesions from de stomach and esophagus,including diagnosis,treatment,and follow up,as well as,reporting our institutional experience.
Literature review
Gastric schwannomas:Gastrointestinal schwannomas are slow-growing benign mesenchymal neoplasms that originate from Schwann cells of the nerve sheath of Auerbach´s plexus or less frequently from Meissner´s plexus[1].They were first described by Daimaruet al[2]since 1988 to date,only 300 cases approximately have been reported in the literature[3].It has been suggested that gastric schwannomas play a different genetic mechanism compared to soft tissue schwannomas by not expressing monosomy on chromosome 22 and very rarely mutations in NF2[4].Mesenchymal tumors include leiomyomas,gastrointestinal stromal tumors (GIST),and schwannomas,with the latter being very rare since it represents 0.2% of all gastric tumors,6.3% of gastric mesenchymal tumors,and 4% of all benign gastric tumors[5-7].Gastric schwannomas tend to appear as single lesions in the stomach with the following subdivisions:the body (59.3%),antrum (26.7%) fundus (12%) and cardia(2%),followed by colon as submucosal tumors[1,3].They have an average reported diameter of 4.69 cm ranging from 0.8 to 15.5 cm.Female predominance has been observed with a male to female ratio of 1:2.64 and can occur at any age,although predominantly between the fifth and eighth decades of life,with 86.43% diagnosed in people over 40 years of age,with an average age of 56.82 years[1-4,6].
The main differential diagnosis of gastric schwannomas are GISTs which careful differentiation of these two entities should be done,since clinical,histological and demographic presentation are very similar,but the treatment and prognosis of each one is very different[1,4].It is estimated that for every 45 cases of gastric GISTs there is gastric schwannoma[4].Gastric schwannomas have an excellent prognosis after surgical resection,while GIST can recur,have malignant potential ranging from 10%to 30% and in certain cases can be treated with imatinib achieving great response[1].
Gastric schwannomas can rarely progress into malignant tumors of the peripheral nerve sheath (MTPNS),known as malignant schwannomas,mainly when they have a mitotic index greater than 10/50 HPF[1,4].Only 10 cases (4.5%) of all gastric schwannomas reported in the literature have been described as MTPNS wich are characterized by a greater number of mitotic index,presence of necrosis and nuclear atypia[1,3].However,this idea of malignant transformation has been questioned in recent research,since most of the malignant transformation were reported prior to modern immunohistochemistry,which they probably corresponded to GISTs instead of schwannomas[4].
Patients with gastric schwannomas are usually asymptomatic with incidental findings in 43.3% during endoscopies for unrelated conditions[1,3,6].Symptomatic patients typically present with abdominal pain or discomfort followed by upper gastrointestinal bleeding and less frequently with a palpable abdominal mass (3.05%),poor appetite (3.05%),dyspepsia (1.82%),weight loss (1.21%),nausea or vomiting(0.6%)[1,3,6].There’s only one case of gastroduodenal intussusception due to gastric schwannoma reported in the literature[8].
Preoperative diagnosis is a challenge for the surgeon because of the difficulty to differentiate gastric schwannomas from GISTs.In upper gastrointestinal endoscopy,gastric schwannomas are frequently seen as firm,protruding submucosal masses and in patients with active bleeding the ulcerated mucosa is observed[1,6].Endoscopic biopsies have limited usefulness since false negatives can occur when the mucosa of the lesion is intact[1].Fine needle aspiration biopsy (FNA) guided by endoscopic ultrasound (EUS) is a reliable diagnostic method although with a reported diagnostic accuracy of 50 to 85.2% for mesenchymal gastric tumors,which have a hypoechoic appearance in the EUS[6,9].
In computed tomography (CT),gastric schwannomas are distinguished by having homogeneous density,leiomyomas often show calcifications and leiomyosarcomas are usually more heterogeneous[10].However,the radiological findings in both CT and magnetic resonance imaging (MRI) of gastric schwannomas are not specific and can be confused with GISTs even with positron emission tomography with 18-fluorodeoxyglucose (PET-FDG),since they present as hypermetabolic[6,11].The diagnosis is based on histology and confirmed with the immunohistochemical report which is the gold standard.Histopathology of these tumors shows a fascicular arrangement with spindle-shaped nuclei.Immunohistochemistry is positive for S-100 protein(Figure 1),vimentin and glial fibrillary acidic protein (Figure 2),CD34 positive or negative,and negative for smooth muscle actin,desmin,DOG-1 and c-Kit (CD117);the latter positive in GIST[12,13].It is important to distinguish gastric schwannomas from malignant tumors with positivity for S-100 such as clear cell gastrointestinal sarcoma and metastatic melanoma[4].
The treatment of choice for gastric schwannomas is surgery where laparoscopy plays an important role.Wedge resection,subtotal or total gastrectomy can be done since they have low malignant potential[1,3,4].Lymphadenectomy is not usually performed unless enlarged lymph nodes are seen,since gastric schwannoma rarely metastasizes to lymph nodes.Only minimally invasive endoscopic approaches should be performed with or without laparoscopic approach,when the diagnosis of gastric schwannoma is definitively confirmed[3].Given its benignity,the recurrence of gastric schwannoma is only associated with positive surgical margins.Frequent CT followup is not recommended[1,14].
Schwannomas of the esophagus:These benign esophageal tumors are very rare since they comprise less than 2% of all esophageal tumors[15-17].The most common submucosal esophageal tumor is leiomyoma,diagnosed in 50% of every benign case,followed by GISTs,which have malignant potential[18-20].Other less frequent benign submucosal esophageal tumors are lipomas,granular cell tumors and schwannomas[21].Gastrointestinal schwannomas comprise between 0.4 and 1% of all submucosal tumors of the gastrointestinal tract,and most of them are found in the stomach,making them extremely rare in the esophagus[15,21,22].
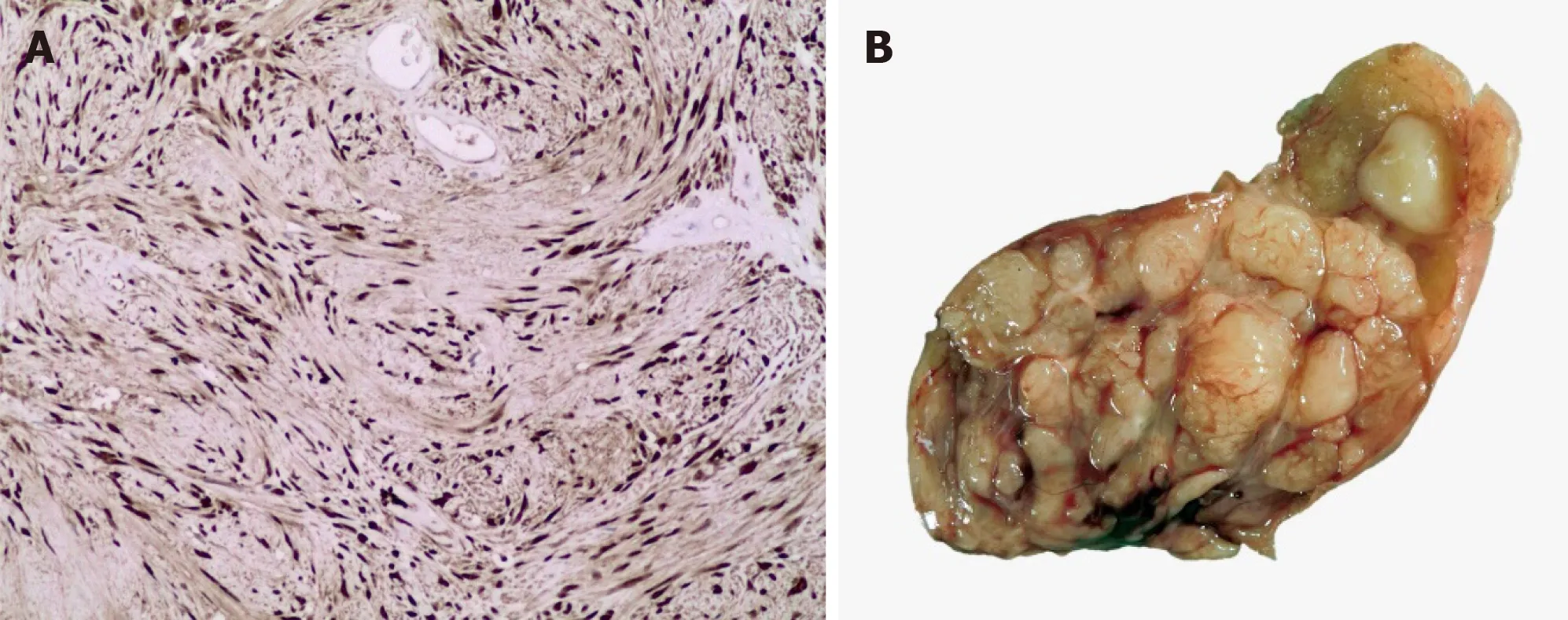
Figure1 lmmunohistochemistry and macroscopic images.
Schwannomas are the most common neurogenic tumor,which are derived from Schwann cells hence its name[15].Schwannomas typically originate in the posterior mediastinum,followed by the chest wall and lung parenchyma,and extremely rare from the esophagus[15,20].Esophageal schwannomas are usually found in the upper thoracic segment[17,23].An average size of 5.6cm has been reported,with a range of 0.5 to 10 cm[24].They are predominant in the female gender with a female to male ratio of 19:8 and a mean age at diagnosis of 50 years[25,26].
Most patients are asymptomatic and are diagnosed incidentally[17].The most common symptom is moderate to severe dysphagia followed by dyspnea[15,17,20].Symptoms usually correlate with tumor size due to the effect of mass on neighboring structures which can also result in chest pain,pneumonia or hemoptysis[17].There are two reported cases of benign schwannoma in the upper esophagus with compression to the trachea[23,25].
The preoperative diagnosis of esophageal schwannoma is a challenge for the surgeon since there are no special characteristics on imaging studies and even endoscopic biopsies can be useless because schwannomas are found in the submucosal tissue[15,21].A successful preoperative diagnosis can lead to a less invasive surgical treatment[26].CT and MRI have limited diagnostic utility;however,its use in conjunction with PET-FDG has been reported to be useful in the diagnosis of esophageal tumors[27].
On CT,esophageal schwannoma tends to show a homogeneous density while leiomyomas often show calcifications;on the other hand,leiomyosarcomas tend to be more heterogeneous[10].Currently,fine FNA biopsy guided by EUS is used to diagnose submucosal tumors because it has a diagnostic accuracy of 85.2%,allowing more adequate samples to be obtained than upper gastrointestinal endoscopy biopsy[10].Some unlikely risks of EUS-guided FNAB are bleeding,infection,trachea perforation;however,it is considered a safe,reliable and accurate method[9,17,21].Through PET,schwannomas prove to be hypermetabolic;however,this has no clinical correlation with malignancy since these tumors are derived from nerve cells that express the type 3 glucose transporter which increases FDG uptake[28].When the preoperative diagnosis is not reliable,a transoperative pathological diagnosis may be useful[17].Schwannomas are usually benign and can show one or two histological patterns:Antoni A and B.The Antoni A pattern shows compact areas with palisaded spindle cells,while the Antoni B pattern consists of poorly organized tissue with variable cystic changes and hemorrhage.MTPNS are the counterpart of benign schwannomas.These tumors are very rare and their histopathological report is characterized by greater mitotic cells,necrosis and atypia[15].Positive immunohistochemistry for S-100 protein and negative for smooth muscle markers such as actin and desmin support the diagnosis of MTPNS[11].Immunohistochemistry is essential to differentiate a GIST from a schwannoma[20,25].
The treatment of esophageal schwannoma is tumoral enucleation or esophagectomy[17,25].Local resection versus esophagectomy is preferred since the former has lower morbidity and is curative for benign schwannomas while the latter has a higher rate of postoperative complications such as recurrent laryngeal nerve palsy,pulmonary involvement or chylothorax[29-31].Tumor enucleation is usually viable because esophageal schwannoma is usually limited to the submucosa;however,this technique is not recommended for very large tumors due to an increased risk of esophageal stenosis[31,32].
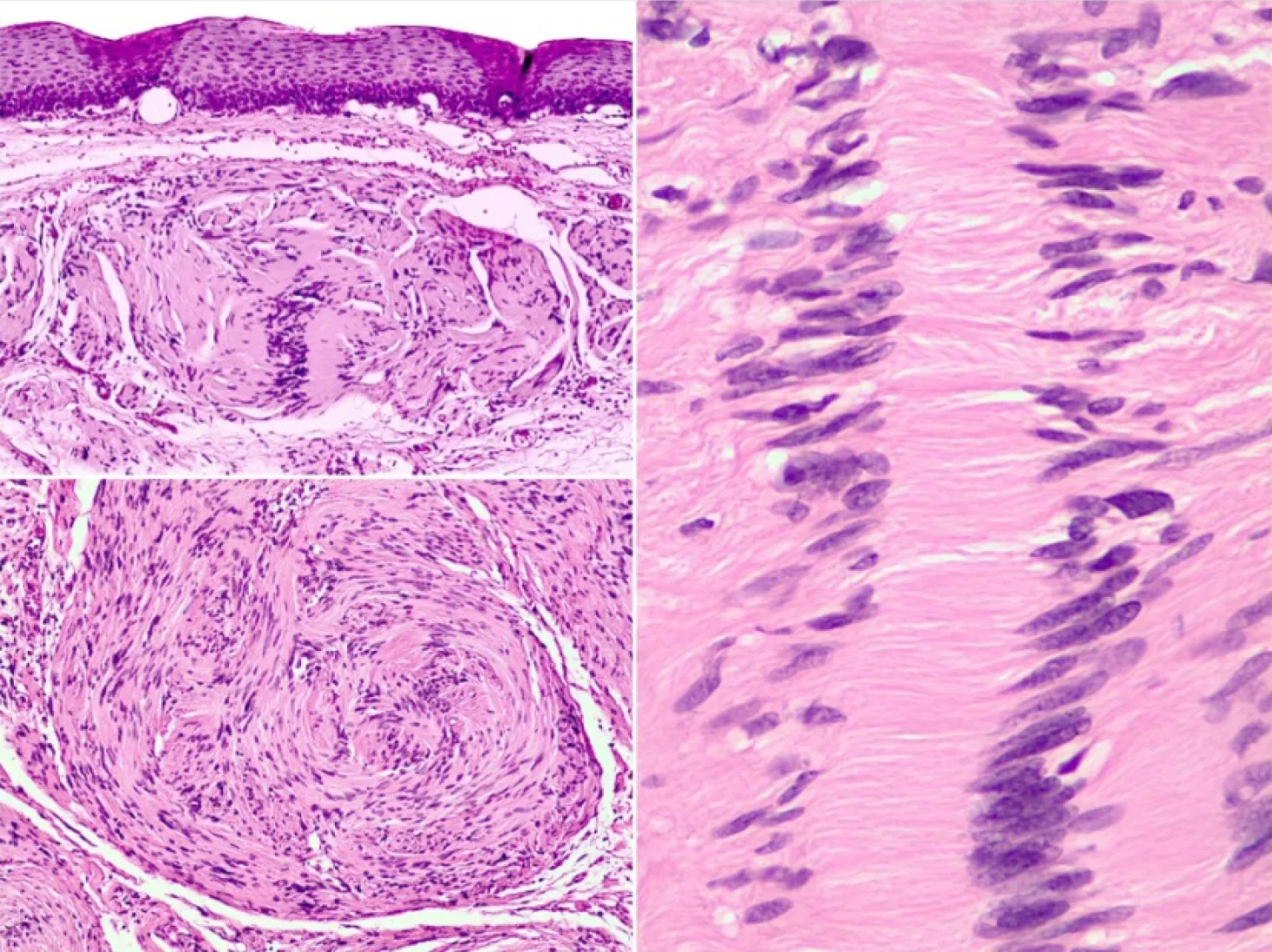
Figure2 Nulcear palisading around fibrillary process (verocay bodies) is often seen in cellular areas.
Surgery is indicated for symptomatic lesions,lesions with a diameter greater than 4 to 5 cm,suspicion of malignancy and lesions that have increased in size during follow up[15].The surgical approach should be considered based on the tumor size,the location of the lesion and the patient's condition[17].
When there is suspicion of malignancy,such as tumor larger than 10 cm,biopsy with mitotic figures,esophageal muscle invasion or cellular atypia;the indication is esophagectomy with negative margins and lymph node dissection to prevent recurrences or lymph node metastases[33,34].For sporadic tumors in the upper thoracic segment,a right thoracotomy is preferred,and less often a cervical approach[15,23,33].There are case reports of successful resections of schwannomas by minimally invasive thoracic surgery (VATS) with less pain,fewer postoperative complications such as pneumonia and shorter recovery time compared to standard thoracotomy[15,18,35].However,VATS is not recommended for large submucosal tumors due to an increased risk of mucosal damage when performing extensive dissections[36].
In general,esophageal schwannomas have a good prognosis after surgical resection and a long term with CT and esophagoscopy is recommended[35].
MATERIALS AND METHODS
A comprehensive literature search was conducted using controlled vocabulary and key words in the following databases:PubMed,MEDLINE,Cochrane and Ovid.The following MeSH terms were used "schwannoma" and "gastrointestinal schwannoma".The detailed search strategy is shown in the study flow diagram (Figure 3).The references of identified studies were also searched to identify additional studies for inclusion.Only English language manuscripts were included.All Gastrointestinal schwannomas specifically located in the esophagus and stomach were included.Cases that did not report long-term follow-up were excluded.Only one researcher carried out the review of the cases reported in the literature.The following variables were extracted for each case report:age,sex,race of the patient,tumor site,tumor size,surgical procedure,long-term follow-up,and disease-free time.
RESULTS
Initially,90 case reports and series of cases were found in the literature,of which 39 publications were excluded due to lack of complete data according to the methodology previously described,and finally 51 articles were included.We extracted a total of 317 cases of esophageal and gastric schwannomas,with a total of 16 and 301 cases respectively[2-4,8,12,34,37-75].The clinical characteristics of these 317 cases[including the documented cases of our center (INCMNSZ)] are summarized in Table 1.
Institutional experience
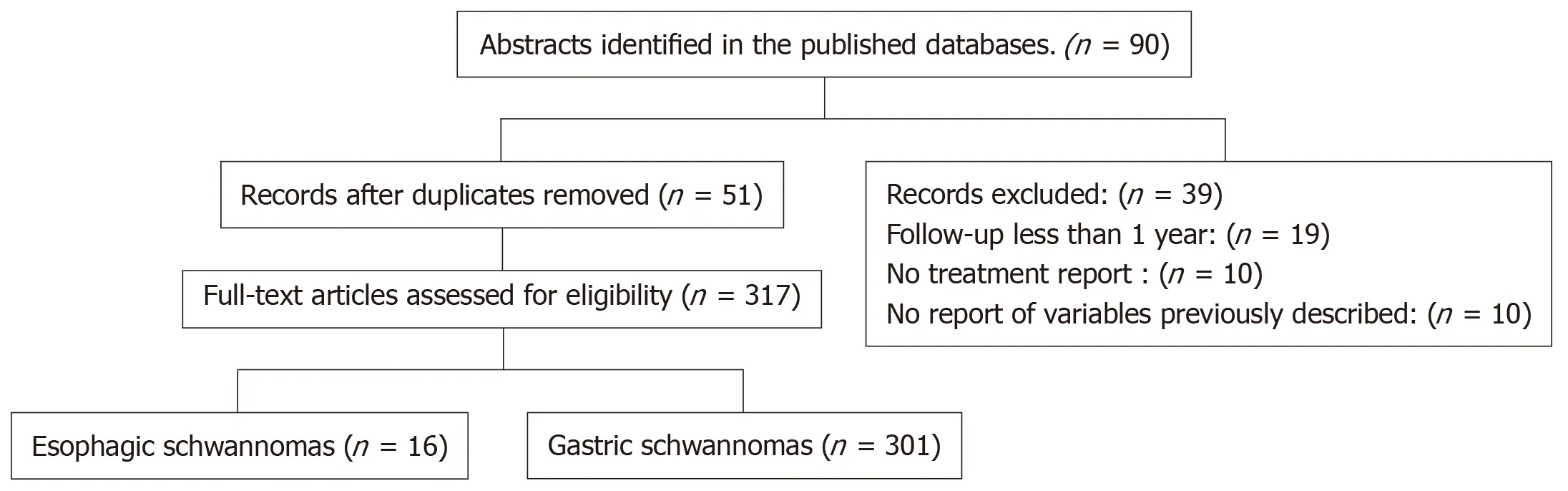
Figure3 Flowchart.
We included a total of 6 upper gastrointestinal schwannomas (esophagus and stomach) (Figure 4).Only one case was at the esophageal level and the remaining 5 at gastric level.The clinical and pathological characteristics of these patients are shown in Table 2.In all 6 cases,complete surgical resection was attempted,with only one case reporting positive surgical margins in the histopathologic report.
DISCUSSION
Schwannomas or neurinomas are benign mesenchymal neoplasms that originate from Schwann cells located at the sheath nerve of the Auerbach’s plexus or less frequently at the Meissner plexus.Its presentation as gastrointestinal tumors are uncommon;being the most frequent location at the level of the stomach,representing 4% of benign tumors at this level,and 2% of all esophageal tumors;a female predominance has been reported,and tend to appear in the 6th decade of life.Most of them are asymptomatic[3,6].
Among the most important differential diagnoses to be ruled out is GIST,which often has a malignant behavior (10%-30%) with different prognosis and treatment.The definitive diagnosis is made through immunohistochemistry which plays a fundamental role,since it allows distinguishing them from other tumors such as GIST and leiomyoma[8,9,10].
Our research tend to review the existing literature in a systematic way and report the clinical experience of INCMNSZ.A total of 317 cases were reported in the main databases while we present a total of 6 cases.Gastric localization showed a higher prevalence in both,the literature review and our institution:94.95% (n= 317) and 83%(n= 5) respectively.With a follow-up with disease-free survival greater than 36 months in most cases:62.01% (n= 80)vs66.66% (n= 4).In both groups,the median size was > 4.1 cm.However,there was a slight discrepancy regarding the age of presentation,which was manifested earlier in the patients of our center with a predominance of 51-60 years of age.
Surgical treatment is curative in most cases and usually a wedge resection,subtotal or total gastrectomy without lymphadenectomy is enough to achieve negative margins with a low recurrence rate.
In conclusion,schwannoma is a clinical entity that must be taken into account in the differential diagnosis of gastrointestinal mesenchymal tumors.It has a good prognosis,and most are benign.
The clinical characteristics reported in the literature are very similar to our series of cases,gastric localization is more prevalent than esophageal location.A disease-free survival of more than 36 mo can be achieved by surgery.
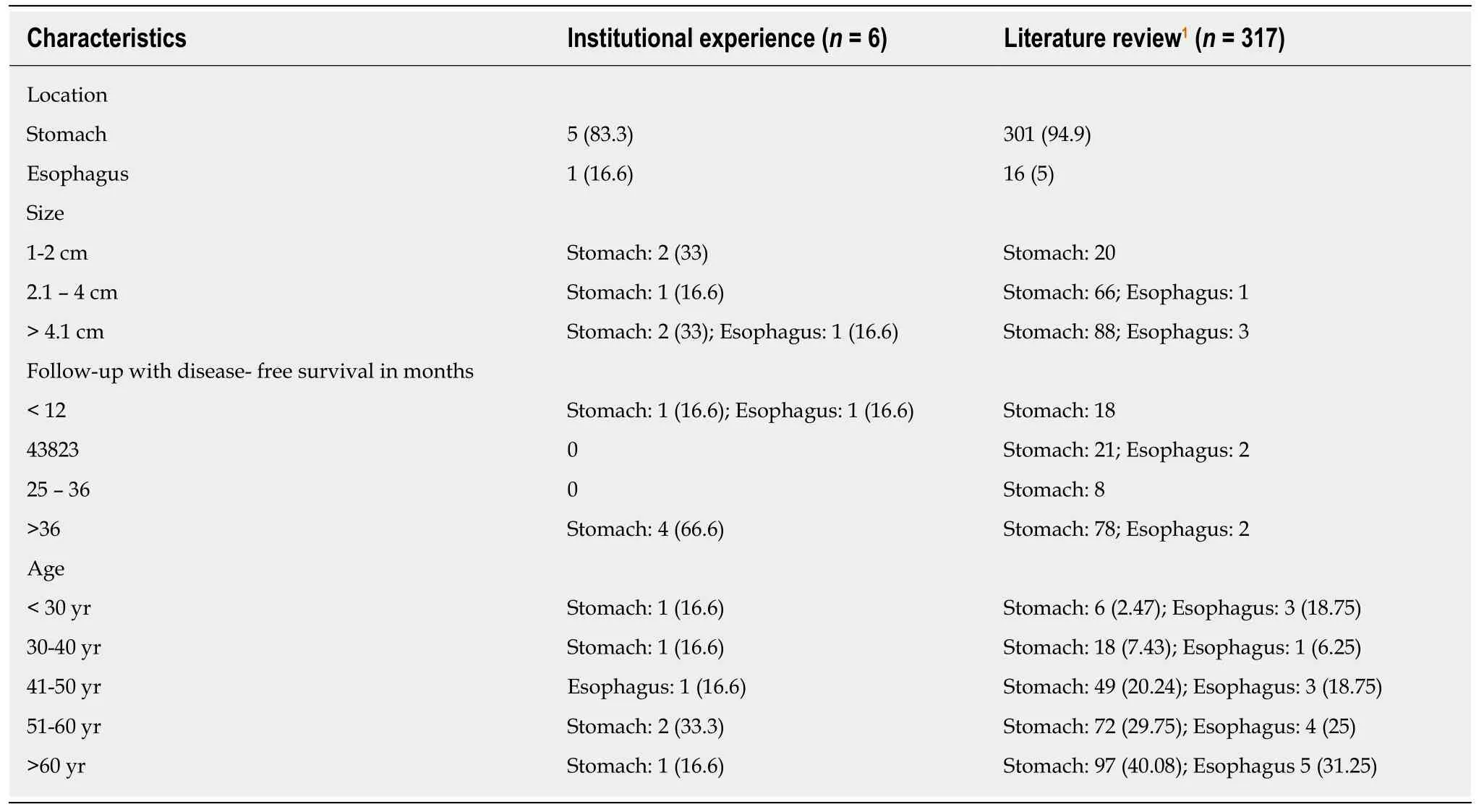
Table1 Clinical characteristics of esophageal and gastric schwannomas,n (%)
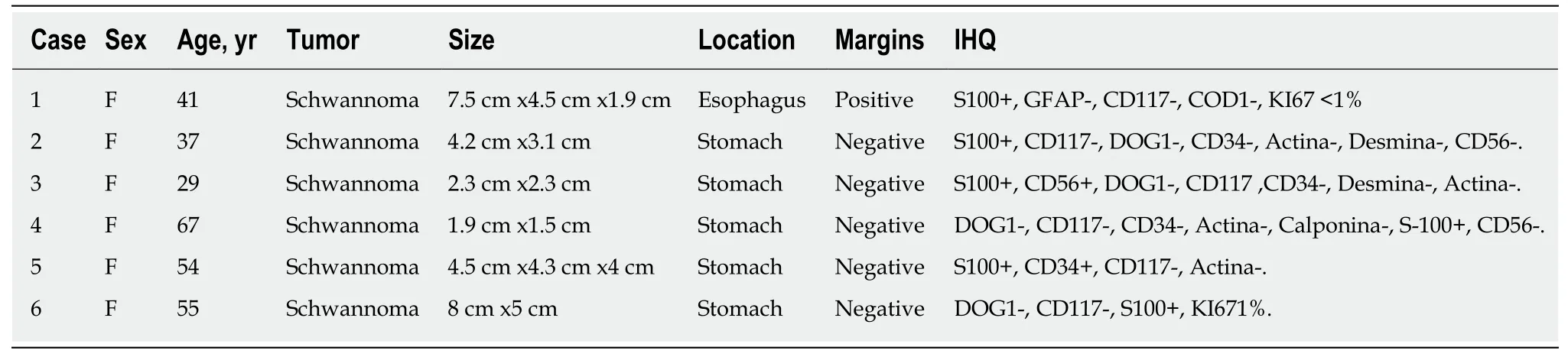
Table2 Clinical and pathological characteristics
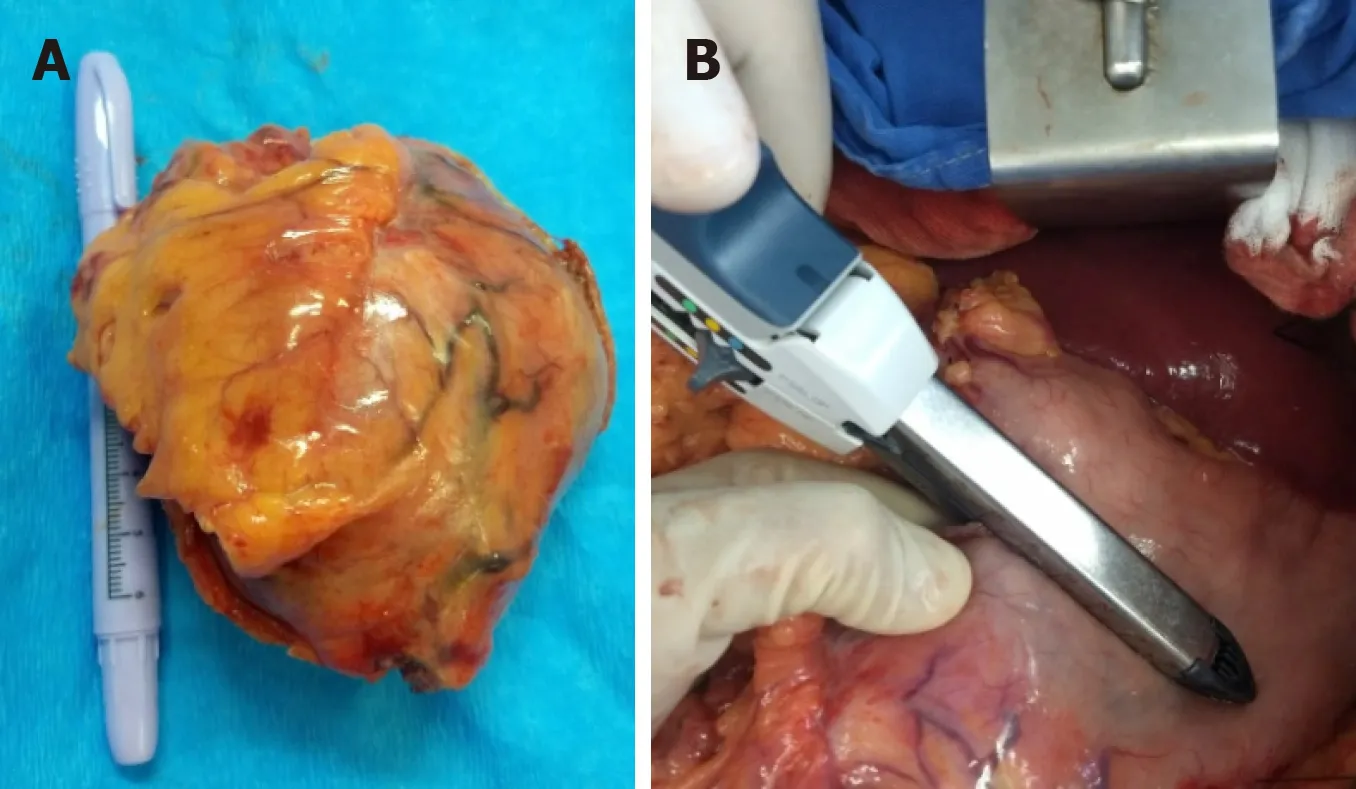
Figure4 Resection of a gastric schwannoma.
ARTICLE HIGHLIGHTS
Research background
Schwannomas are benign neoplasms originated from Schwann cells.Schwannomas are more commonly locate in the stomach.Schwannomas are usually asymptomatic lesions.
Research objectives
We have reviewed the available literature about gastrointestinal schwannomas,especially lesions from de stomach and esophagus (diagnosis,treatment,and follow up).
Research methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes guidelines,a systematic review was conducted.The PubMed,Ovid,MEDLINE,and Scopus databases were used for reviewing process.Only English language manuscripts were included.All gastrointestinal schwannomas specifically located in the esophagus and stomach were included,and cases that did not report long-term follow-up were excluded.
Research results
Gastric localization showed a higher prevalence in both,the literature review and our institution.With a follow-up with disease-free survival greater than 36 mo in most cases.In both groups,the median size was > 4.1 cm.Surgical treatment is curative in most cases.
Research conclusions
Schwannoma must be taken into account in the differential diagnosis of gastrointestinal mesenchymal tumors.Schwannoma has a good prognosis,and most are benign.A disease-free survival of more than 36 mo can be achieved by surgery.
 World Journal of Gastrointestinal Oncology2019年9期
World Journal of Gastrointestinal Oncology2019年9期
- World Journal of Gastrointestinal Oncology的其它文章
- Gallbladder cancer harboring ERBB2 mutation on the primary and metastatic site:A case report
- Detection and management of oligometastatic disease in oesophageal cancer and identification of prognostic factors:A systematic review
- Colorectal cancer fecal screening test completion after age 74,sources and outcomes in French program
- Correlation between invasive microbiota in margin-surrounding mucosa and anastomotic healing in patients with colorectal cancer
- MicroRNA-331 inhibits development of gastric cancer through targeting musashi1
- Tumor progression-dependent angiogenesis in gastric cancer and its potential application
