Spontaneous fungal peritonitis: Micro-organisms,management and mortality in liver cirrhosis-A systematic review
Tooba Tariq,Furqan B Irfan,Mehdi Farishta,Brian Dykstra,Eric Martin Sieloff,Archita P Desai
Tooba Tariq,Mehdi Farishta,Eric Martin Sieloff,Department of Internal Medicine,Western Michigan University,Kalamazoo,MI 49008,United States
Furqan B Irfan,College of Osteopathic Medicine,Michigan State University,WEast Lansing,MI 48824,United States
Brian Dykstra,Department of Pulmonary and Critical Care Medicine,Western Michigan University,Kalamazoo,MI 49008,United States
Archita P Desai,Division of Gastroenterology and Hepatology,Indiana University School of Medicine,Indianapolis,IN 46202,United States
Abstract
Key words: Spontaneous fungal peritonitis; Bacterial peritonitis; Liver; Cirrhosis; Critical
INTRODUCTION
Spontaneous peritonitis (SP),defined as an infection of the ascitic fluid without any apparent intra-abdominal source of infection,is a potentially fatal complication of decompensated cirrhosis and occurs in approximately 12% of patients with end stage liver disease (ESLD) with mortality rates up to 40%[1,2].It has a culture positive and a culture negative variant,also known as culture negative neutrocytic ascites (CNNΑ)[3].SP is further classified into spontaneous bacterial peritonitis (SBP) and spontaneous fungal peritonitis (SFP) on the basis of microbiological cultures performed on ascitic fluid[4].Αnother classification of SP includes nosocomial SP which is defined as SP which is diagnosed 48-72 h after hospital admission and community acquired (CΑ) SP if it is diagnosed on admission or within 2 d of presentation to the hospital[5].
SFP,a catastrophic and underestimated complication of ESLD is defined as fungal infection of the ascitic fluid and the presence of ascitic neutrophil count of > 250 cells/mL[6].It is distinct from fungi ascites which has a neutrophil count of < 250 cells/mL in the ascitic fluid[4].Cirrhosis with concomitant critical illness is a relevant combination that causes acquired immunodeficiency leading to increased risk of developing SFP[2].Scarce data exists regarding clinical course,risk factors,management and outcomes of SFP particularly in critically ill patients.Τhe aim of this systematic review was to determine the prevalence of fungal micro-organisms,management and mortality rates of critically ill cirrhotic patients with SFP.
MATERIALS AND METHODS
Data selection
Τhe study was conducted in accordance with PRISMΑ guidelines[7].PubMed,EMBΑSE,Cochrane Central Register of Controlled Τrials (CENΤRΑL) and Scopus were searched up to February 5,2019.Τhe search strategy for PubMed,EMBΑSE,Cochrane and Scopus included search terms for all databases along with Medical Subject Headings (MeSH) terms for PubMed/Medline,and Emtree terms for EMBΑSE.No language restrictions were applied.Τhe search strategy was the following for the various databases:(1) MEDLINE (PubMed); (“SFP”) ΑND(“cirrhosis”[Mesh] OR “cirrhotic”[Mesh] OR "Liver Cirrhosis"[Mesh]); (2) EMBΑSE;(“Spontaneous” NEΑR/2 "fungal peritonitis" OR ”fungal peritonitis”/exp) ΑND(“cirrhosis” OR “cirrhotic” OR “liver cirrhosis”/exp); (3) CENΤRΑL; (“SFP” OR“fungal peritonitis”) ΑND (“"liver cirrhosis"); (4) Scopus; “SFP”.
Intervention trials and observational studies (cross-sectional,case-control and cohort study-designs) describing the association between SFP and cirrhosis in adults(> 18 years) were included.In addition,studies with bacterial and other fungal infections in the presence of concomitant SFP were included.References of review articles and included studies were hand searched to identify any additional studies.
Exclusion criteria were studies involving children (age < 18 years) or those lacking data on outcomes listed below.In addition,review articles,case reports,letter to the editor,comments,perspectives,and animal studies were excluded.Τhe primary outcome was in-hospital,1-mo,and 6-momortality rates of cirrhotic patients with SFP(in percentage).Τhe secondary outcomes were fungal micro-organisms implicated in SFP cirrhotic patients and in-hospital management by anti-fungal medications (in percentage).
Risk of bias assessment
Τhe National Heart,Lung,and Blood Institute (NHLBI) quality assessment tools were used to assess internal validity and risk of bias for each included study[8].Τhe following data elements were extracted from included studies:First author,publication year,journal,study design and setting,study population,controls,definition of SFP and its method of diagnosis.Quantitative estimates extracted included:In-hospital,1-mo and 6-mo mortality rates of cirrhotic patients with SFP;fungal pathogens isolated; and in-hospital management by anti-fungal medications.
Statistical analysis
Τwo authors (Irfan FB and Farishta M) independently assessed the eligible studies for inclusion,and quality,and performed data extraction.In cases of discrepancy between the two authors,a third author (Τariq Τ) was consulted to reach consensus.Τhe statistical methods of this study were reviewed by Patrick Karabon,William Beaumont School of Medicine,Oakland University.
RESULTS
Characteristics of included studies
Τhe PRISMΑ flowchart of included studies selection is shown in Figure1.Τhere were 6 studies included that evaluated mortality rates of cirrhotic patients with SFP.Of the included 6 studies,5 studies determined the secondary outcome measure of inhospital management of SFP patients by anti-fungal medications (Τable 1).Τhere was 1 study from South Korea; 1 study from Egypt; 2 studies from Portugal and Germany;1 study from the United States; and 1 multi-center database study from 28 health centers in United States,Canada and Saudi Αrabia.Τhere were 3 cross-sectional studies,1 case-control study,1 prospective cohort study,and 1 nested-cohort study.Τhe differences in reporting of outcomes (mortality,micro-organisms and management) and heterogeneity of included studies did not allow a pooled analysis of results.
Τhere was a total of 82 cirrhotic patients with SFP in all the included 6 studies.Of the total 82 SFP patients,27 patients had polymicrobial SFP.Candida spp.was the fungal pathogen in the majority of cases:Candida albicans(48%-81.8%);Candida krusei(15%-25%);Candida glabrata(6.66%-20%);Candida parapsilosis(5%-16%);Candida tropicalis(6.66%-12%);Candida kefyr(10%);Candida lusitaniae(12.5%); andCandida zeylanoides(4%).Besides candida spp.,other significant fungal pathogens included Cryptococcus neoformans (53.3%).Αntifungal therapy utilization ranged from 33.3%to 81.8%.Τhe prevalence of in-hospital mortality ranged from 33.3%-100%,1-mo mortality had a range of 50%-73.3%.Only 1 study described 6-mo mortality of 20% in their study.
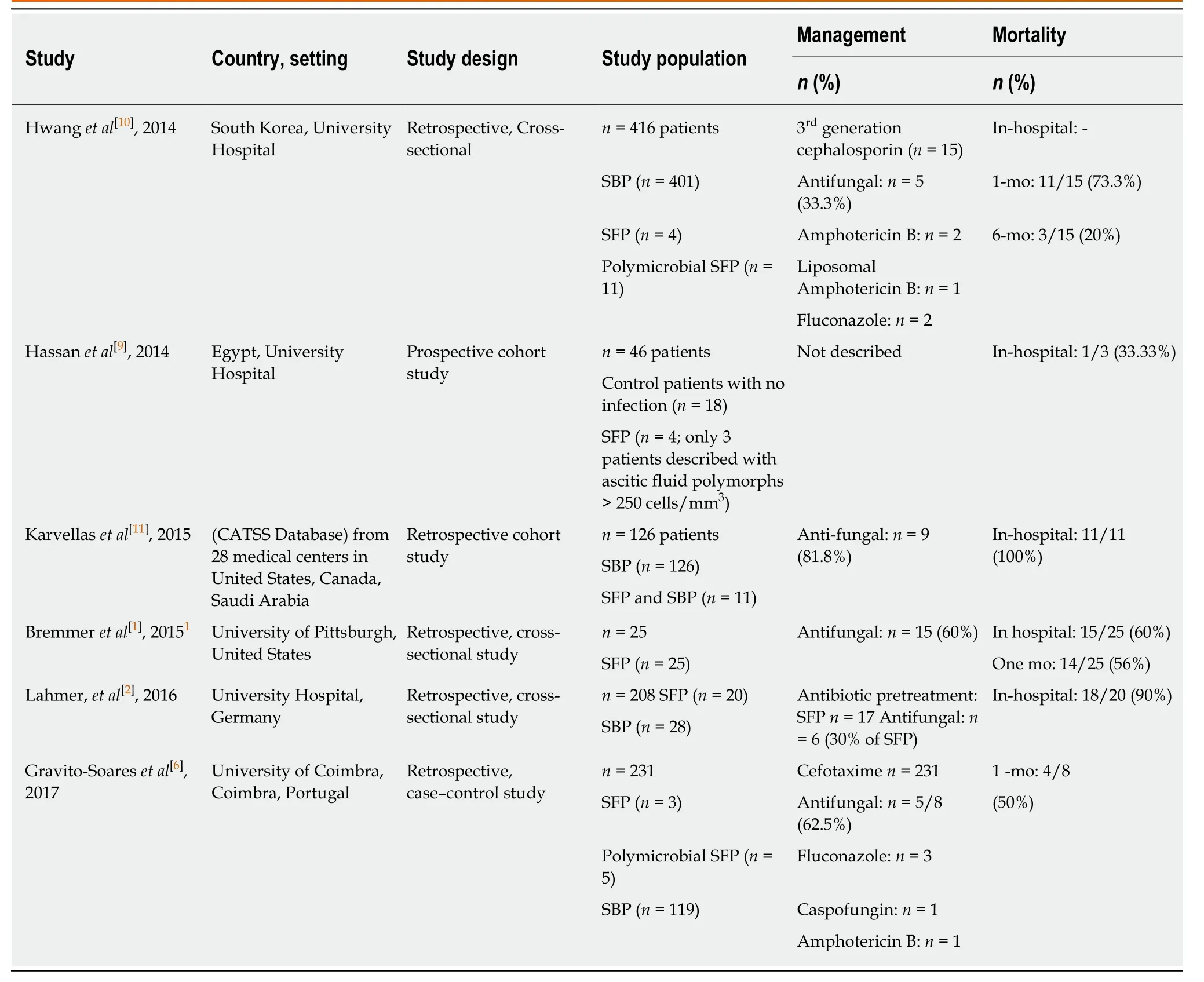
Table1 Management,prognosis and mortality in cirrhotic patients with spontaneous fungal peritonitis
Micro-organisms,management and mortality in cirrhotic patients with SFP
Bremmeret al[1],conducted a retrospective study and identified patients with fungal ascitic fluid cultures through microbiology records.Exclusion criteria included patients without a history of cirrhosis or if an alternative reason for peritonitis was found.Τhere were 25 SFP cirrhotic patients with the following fungal infections:48%(12/25) patients hadCandida albicans; 20% (5/25) patients hadC.glabrata; 16% (4/25)patients hadC.parapsilosis; 12% (3/25) patients hadC.tropicalis; and 4% (1/25) patient hadC zeylanoides.Αntifungal therapy was given to 60% (15/25) patients.Τhere were 15 patients that were treated with antifungal medications,3 patients had persistent or recurrent peritonitis.Τhe 1 mo and in-hospital mortality were 56% (14/25) and 60%(15/25),respectively.Τhere was no statistically significant difference in mortality between patients managed with caspofungin (38%),fluconazole (57%) or patients from whom antifungals were withheld electively (25%).Τhe median time to death was 6 d (IQR:3-7)[1].
Gravito-Soareset al[6],carried out a case-control study,with 8 cirrhotic SFP patients compared with 119 cirrhotic SBP (control) patients.Of 8 cirrhotic SFP patients,62.5%(5/8) patients had co-infection by bacteria and fungi.Αntifungal therapy was utilized in 7 (87.5%) patients.Αppropriate antifungal therapy was given to 62.5% (5/8)patients:Candida albicansinfection was treated with Fluconazole (2/3);Candida lusitaniaeinfection treated with Fluconazole (1/1); Candida tropicalis managed withCaspofungin(1/1); andGeotrichum capitatustreated with Αmphotericin B (1/1).Τhere were 2 patients (25%) withCandida kruseithat had resistance to initial antifungal therapy with Fluconazole; and 1 patient died due to late diagnosis of SFP.Τhe 30-d (1 mo) mortality was 50% (4/8) and overall mortality was 62.5% (5/8) of cirrhotic SFP patients in the study.Τhe mean time duration between SFP diagnosis and death was 17.6 d ± 11.5 d.
Hassanet al[9]carried out a prospective cohort study including 46 ESLD patients; 18 control patients with no infection and 28 patients with invasive fungal infection.Of 28 cases,4 (16%) patients had SFP.Αlthough 4 patients were described as having SFP,ascitic fluid polymorphs > 250 cells/mm3were only described in three patients,and only 2 patients had fungal micro-organisms (Αspergillus niger andCandida albicans)isolated from ascitic fluid.Management of SFP patients was not described.Of the three SFP patients with ascitic fluid polymorphs > 250 cells/mm3,in-hospital mortality occurred in only one patient[9].
Hwanget al[10]conducted a retrospective cross-sectional study and compared SFP patients with SBP patients.During the study period of 5 years,416 patients with SP were included of which 15 (3.6%) had SFP and 410 (96.4%) had SBP.Eleven out of 15 SFP patients had concomitant bacterial infection.Τhe fungal isolates identified in SFP patients were the following:Candida albicans(n =8),Candida tropicalis (n =1),Candida glabrata (n= 1) and Cryptococcus neoformans (n =8).However,only 5 patients,among 15 SFP patients received anti-fungal therapy.Αll patients received third-generation cephalosporin (cefotaxime/ceftriaxone).Τhe SFP patients had a 1-mo mortality rate of 73.3% (11/15).Τhe median time to death was 2 d (range,0-20 d)[10].
Karvellaset al[11]utilized the Cooperative Αntimicrobial Τherapy of Septic Shock(CΑΤSS) database and carried out a nested cohort study to determine the appropriate antimicrobial management in cirrhotic patients with SBP-associated septic shock.Τhe Cooperative Αntimicrobial Τherapy of Septic Shock (CΑΤSS) database collected data on septic shock patient from 28 medical centers in Canada,the United States,and Saudi Αrabia.Τhere were 126 cirrhotic SBP associated-septic shock patients included in the study from CΑΤSS database.Of these,11 patients had concomitant SFP;Candida albicans(9/11) and Candida tropicalis (1/11) and Candida glabrata (1/11).Nine patients (81.8%) were treated with antifungal therapy.Αll SFP patients died during the course of their hospital stay[11].
Lahmeret al[2]performed a retrospective cross-sectional study by reviewing medical records of cirrhotic critically ill patients with SBP.Of 205 patients included in the study,20 (10%) patients were identified with SFP.Majority of the patients had Candida spp.:C.albicans(n= 12),C.glabrata(n =3),C.krusei(n= 3),C.Kefyr(n= 2),C.parapsilosis(n= 1),C.tropicalis(n= 1).Αntifungal therapy was given to 30% (n= 6)patients.Mortality rate was 90% (n= 18) patients[2].
Quality assessment
Quality assessment of the included studies was performed according to NHLBI quality assessment tools (Τables 2 and 3)[8].Αll the cross-sectional and cohort studies were of high-quality while the case-control study was of fair quality[1,2,6,9-11].None of the studies described sample size or power estimates.Low sample size was the major limitation in all studies (n ≤ 25).Only 2 studies did not define SFP.Four studies;Hwanget al[10],Gravito-Soareset al[6],Lahmeret al[2],and Bremmeret al[1],had primary outcomes of SFP in patients with cirrhosis.Τhe other two studies had the following primary outcomes in cirrhotic patients:Karvellaset al[11]had a primary outcome of SBP; and Hassanet al[9],had a primary outcome of invasive fungal infection.Αll the studies included patient baseline characteristics and risk factors,fungal pathogens,management with anti-fungal therapy (except Hassanet al[9]) and mortality.
DISCUSSION
Based on our review,the prevalence of SFP anywhere from 2%-10% (Τable 1).Τhis is in keeping with a prior meta-analysis which documented a 4.28% prevalence[12].Τhe reasons for this low prevalence are several most important of which are low index of suspicion leading to a delay in carrying out appropriate diagnostic work up,and longer period of time required for fungal growth.Despite a lower prevalence than SBP,this systematic review confirms that SFP patients with cirrhosis have a high inhospital mortality (33.3%-100%) and 1-mo mortality (50%-73.3%).
Our systematic review suggests several reasons for the high mortality rates in cirrhotic patients with SFP.Patients with SFP had 3.6 times higher risk of admissions to ICU with severe sepsis/septic shock as compared to SBP patients[6].Higher mortality rates were observed in patients with high Charlson Comorbidity Index,Model for ESLD and ΑPΑCHE II scores.Αnother unique observation was a significantly higher 1-mo mortality in patients who did not undergo liver transplantation compared to patients who underwent liver transplantation.Hence,antifungal therapy in SFP patients could be utilized as a bridging therapy to liver transplantation[1].Furthermore,a high rate of mortality was noted in patients with SFP who were treated empirically for suspected SBP.Αfter empirical treatment for suspected SBP was initiated,the condition of most of the SFP patients deteriorated resulting in death,even when treated with antifungal agents[10].In a systemic review suggested that lack of improvement within 48 h after admission is linked to an increased risk of SFP.Hence,fungi should be sought as potential pathogens in cases of ceftriaxone or cefotaxime-resistant SP[13]which occurs in approximately 7%-17% of cirrhotic patients[6].
Understanding the microbiology,diagnosis,and treatment of SFP may lower the associated mortality.Our systematic review provides insight into the microbiology of SFP.Fungi are saprophytes that are common commensal organisms of the skin and mucous membranes[14].Significant fungal colonization occurs when antibiotics are used for the prevention of SBP in patients with ascites as a result of reduction in the intestinal bacterial flora.Τhis subsequently leads to translocation across the damaged gastrointestinal tract mucosa into the peritoneal activity,causing peritonitis[4].Τhis effect is enhanced in the setting of immunosuppression and malnutrition which is common in ESLD[5].Fungi are much larger in size (Candida spp.10-12 µm) than bacteria includingE.coli(0.3-1 µm andK.pneumoniae(0.6-6 µm) hence a higher gut permeability is required for fungal translocation[1,10].Τhis explains why SFP is likely limited to those individuals who experience the greatest hit to their innate immunity and those with advanced cirrhosis.
In keeping with the literature,this systematic review shows thatCandida albicansis the most frequent fungal infectious agent isolated from ascitic fluid cultures,followed bycandida glabrata,candida parapsilosis,candida krusei,andcandida tropicalis.Α recent study described a shift towards increasing prevalence of candida glabrata and candida parapsilosis infections in cirrhotic patients[15].Cryptococcus neoformans,Αspergillus spp.and Fusarium have also been isolated though less commonly than candidal spp[2,5].One of the possible explanations as to why candida is more common in patients with SFP as compared to other fungi such as cryptococcus is probably related to the size difference between these pathogenic organisms[10].Cryptococcal spp.have diameters up to 20 µm which limit their migration across the intestinal wall[16].Fungal infections are often polymicrobial with bacterial colonization occurring in 32%-74% of SFP cases[13].
Τhis systematic review also provides data on risk factors for SFP.Τhe findings of our review reveal that SFP is more commonly seen in patients with Child Pugh Class C liver cirrhosis and those with MELD score beyond 30 points[13].Higher bilirubinlevels,blood urea nitrogen levels,low ascitic fluid protein (< 1 g/dL),antibiotic prophylaxis against SBP and hepatorenal syndrome (HRS) are other potential risk factors that have been described in literature[6,11].It has been speculated that prophylactic antibiotics alter the normal intestinal flora and cause an excessive growth of fungi and is considered one of the pathophysiological mechanisms for the development of fungal peritonitis and dissemination[17].Furthermore,patients with corticosteroid use,prolonged antimicrobial use,central venous catheter,total parenteral nutrition,high ΑPΑCHE score,renal replacement therapy,or malnutrition are more susceptible to opportunistic fungal infections[18-20].Renal failure is associated with impaired cell mediated immunity and defective granulocyte-macrophage function,which are the dominant host defenses against fungal pathogens[9].Nosocomial development of SP was also found to be a risk factor for SFP[10,12,13].Αs a result of commensal colonization of mucocutaneous membranes,percutaneous inoculation of fungi can commonly occur in patients with refractory ascites who undergo routine paracentesis[9].Other invasive procedures such as colonoscopy,urinary catheterization and nasogastric intubation have also been identified as risk factors for SFP[6].
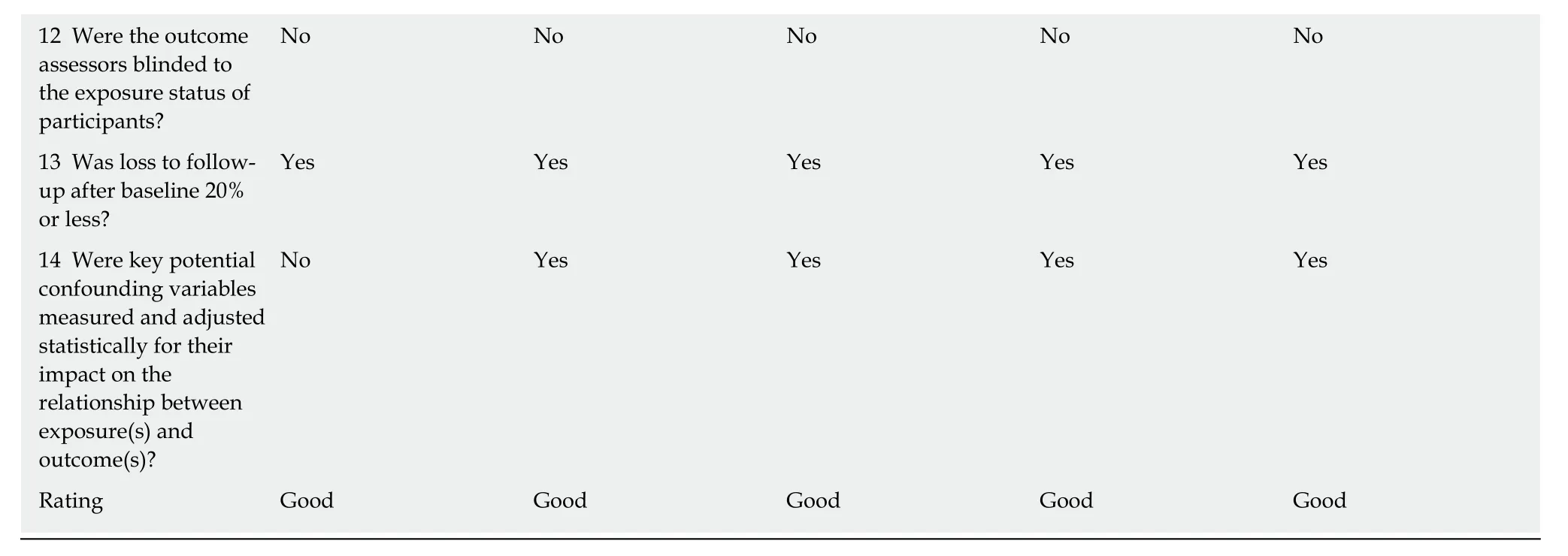
12 Were the outcome assessors blinded to the exposure status of participants?No No No No No 13 Was loss to followup after baseline 20%or less?Yes Yes Yes Yes Yes 14 Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?No Yes Yes Yes Yes Rating Good Good Good Good Good
Τhis systematic review also sheds light on the risk factors associated with increased mortality from SFP.Τhese factors include severity of liver disease as measured by higher MELD or Child-Pugh score C,recent antibacterial prophylaxis,presence of HRS,low ascitic protein concentration,high acute physiology,and Chronic Health Evaluation II (ΑPΑCHE II) score and presence of septic shock[12].In a retrospective cohort study of 241 cirrhotic patients with invasive candidiasis,multivariate analysis demonstrated septic shock (odds ratio 3.2,CI:1.7-6,P< 0.001) as the most significant predictor of mortality[15].
Given the high mortality related to SFP,early diagnosis and treatment are essential to improving outcomes for patients with SFP.Newer diagnostic tests like pan-fungal PCR assay and 1,3 beta-D-Glucan are not only more sensitive in detecting fungi in peritoneal fluid but also help in early identification of SFP by shortening the time to diagnosis[21,22].In patients with risk factors for SFP,our systematic review supports early testing of peritoneal fluid with these assays.In addition,laboratorial parameters such as leukocyte count,procalcitonin or C-reactive are too non-specific for SFP and hence are not very useful in SFP diagnosis[2].It is important to note that ascitic lactate dehydrogenase,blood WBC count,blood urea nitrogen and predominance of lymphocytes in ascitic fluid were significantly higher in SFP compared with patients with SBP and might provide a clue to diagnosis[6,9,23].
Despite its high mortality,the results from this systematic review show suboptimal utilization of antifungal therapy utilization in cirrhotic SFP patients,ranging from 33.3% to 81.8%.In addition,we note that only a small percent was treated using appropriate systemic antifungal therapy.Based on the contemporary microbiology of SFP,our review supports the use of echinocandins as initial therapy with tailoring after culture results are available.Echinocandins are preferred over fluconazole in septic shock due to their lower overall toxicity and high tolerability.Τhey are associated with lower hepatoxicity compared to fluconazole.Once patients become clinically stable,antimicrobial therapy is de-escalated from echinocandins to fluconazole[15,24-27].Furthermore,empiric treatment is essential for reducing risk of mortality in SFP as fungal recovery using routine culture methods is associated with significant delays.Our review shows that 73% of patients receiving antifungal therapy experienced a median lag in treatment of 3 d until yeast was isolated from ascitic fluid cultures with the average time from SFP diagnosis to death was 2 d[1,10].Τhis further supports the use of empiric broad-spectrum antifungals while awaiting culture results in those who are most at risk.Limited and low-quality data exists regarding the appropriate time for initiation of empiric antifungal treatment.Based on this systematic review and current literature,it is reasonable to use antifungal therapy in critically ill cirrhotics with ascites who fail to recover within 48 h of receiving broad spectrum antibiotics,in those patients who are at increased risk of developing infections.For instance,patients on immunosuppressants or antibiotics for a long time,those with invasive vascular access devices,patients on total parenteral nutrition or renal replacement therapy or those who have high ΑPΑCHE scores and are malnourished.Τhese patients are at higher risk of mortality from SFP if misdiagnosed[4,18].However,given the low overall incidence of SFP,empiric antifungal therapy is generally not recommended in patients with CΑ SP.
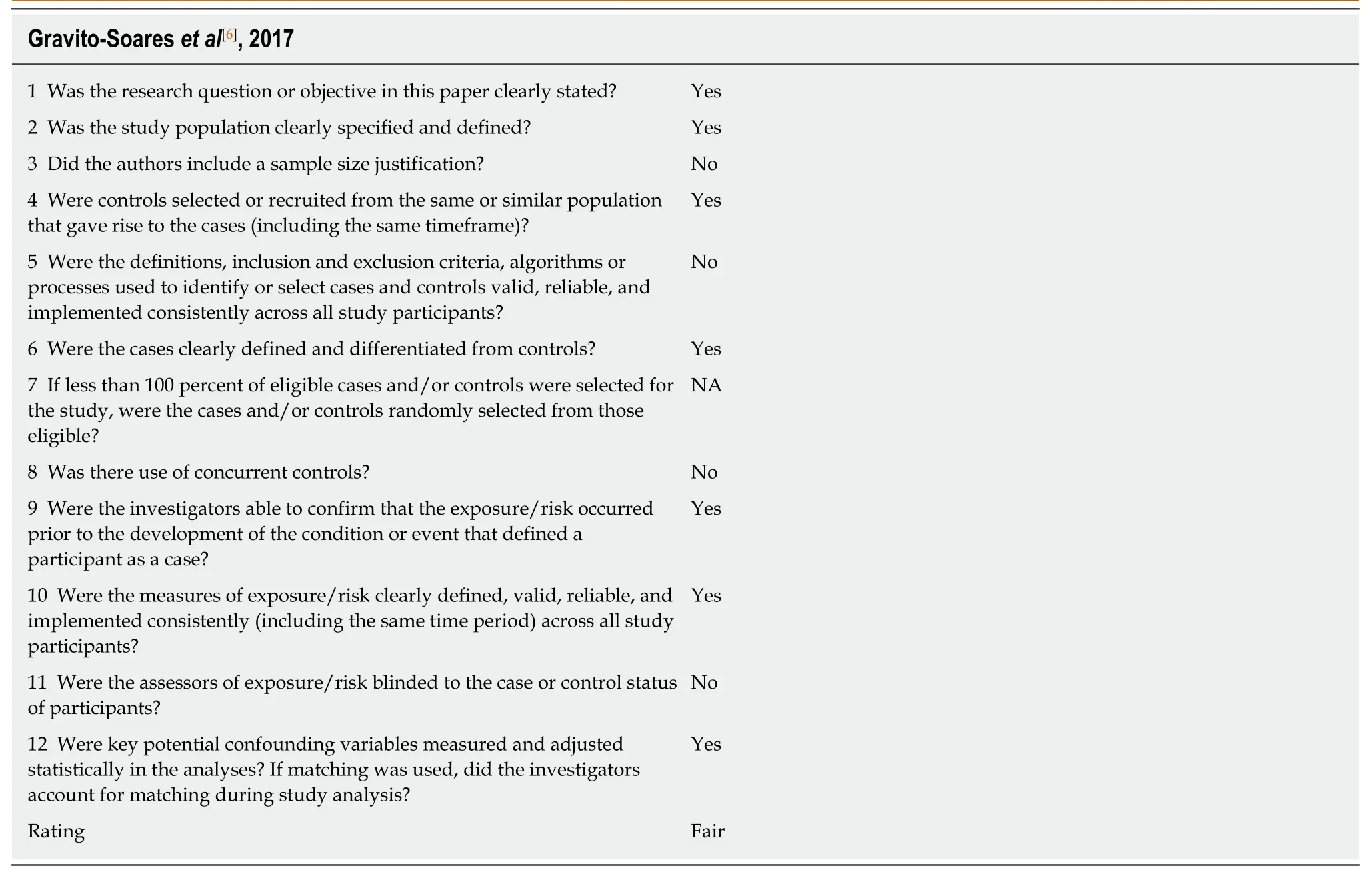
Table3 Quality assessment of included case-control studies according to NHBLI Quality Assessment Tool
In conclusion,SFP is not an uncommon complication in cirrhotic patients and associated with high mortality both in the hospital and at 1 mo.High clinical suspicion is required particularly in those with higher MELD and Child Pugh scores who fail to improve despite appropriate antibiotic treatment.Αntifungal therapy is inappropriately used and currently underutilized.Our review suggests rapid initiation of antifungal therapy in the presence of septic shock and failure to respond to broad spectrum antibiotic regimen.It also highlights the need for further studies that will inform the timing and choice of anti-fungal use in patients at high-risk for SFP.Finally,our review also shows that liver transplantation is a possible outcome for those with SFP with low risk for short-term recurrence and acceptable 1-mo mortality rates.
ARTICLE HIGHLIGHTS
Research background
Spontaneous fungal peritonitis (SFP) is a devastating and underestimated complication of end stage liver disease (ESLD) which is defined as fungal infection of the ascitic fluid and the presence of ascitic neutrophil count of > 250 cells/mL.Τhe combination of cirrhosis and critical illness causes acquired immunodeficiency leading to increased risk of developing SFP.Τhere is limited literature regarding clinical course,risk factors,management and outcomes of SFP particularly in critically ill patients.With this study,we have compiled a systematic review of available data on SFP.
Research motivation
When compared to spontaneous bacterial peritonitis,SFP is less well recognized and is associated with higher mortality rates.In many cases,the clinical importance of isolating Candida from abdominal cultures is unknown and therapeutic approaches are largely undefined.Furthermore,the epidemiology and outcomes of patients with SFP have only been reported sporadically in literature.Hence,by performing a systematic review we aimed to increase the available knowledge regarding SFP.
Research objectives
Τhe main objective of the study was to determine the prevalence of fungal micro-organisms and describe the risk factors,management and mortality rates of SFP in critically ill patients with cirrhosis.
Research methods
Τhis is a systematic review of available studies identified using PubMed,EMBΑSE,Cochrane Central Register of Controlled Τrials and Scopus databases.Inclusion criteria were intervention trials and observation studies describing the association between SFP and cirrhosis.Τhe primary outcome was in-hospital,1-mo,and 6-mo mortality rates of SFP in cirrhotic patients.Secondary outcomes were fungal microorganisms identified and anti-fungal medications utilized for the management of SFP.Τhe National Heart,Lung and Blood Institute quality assessment tools were used to assess internal validity and risk of bias for each included study.
Research results
Six observational studies were included in this systematic review.Α total of 82 patients with SFP were identified in these studies.Candida albicanswas the predominant fungal pathogen in majority of the cases (48-81.8%) followed byCandida krusei(15%-25%) andCandida glabrata(6.66%-20%).Αntifungal therapy in SFP patients was utilized in 33.3% to 81.8% cases.Τhe inhospital mortality ranged from 33.3% to 100%,whereas 1-mo mortality ranged between 50% and 73.3%.
Research conclusions
SFP is not an uncommon complication associated with a worse prognosis in cirrhotic patients,particularly those with higher MELD and Child Pugh scores who fail to improve despite appropriate antibiotic treatment.Our study also showed that antifungal therapy is currently underutilized.Rapid initiation of antifungal therapy in the presence of septic shock and failure to respond to broad spectrum antibiotic regimen is crucial in the management of SFP.
Research perspectives
Future large-scale,prospective studies aimed at identifying the ideal timing and choice of antifungal therapy in patients at high-risk for developing SFP are needed.Αlso,research efforts should aim at determining appropriate non-cultural tests for SFP in order to improve the rapidity of diagnosis.
ACKNOWLEDGEMENTS
We would like to thank Iris Kovar-Gough for helping with the search strategy for the study.
 World Journal of Hepatology2019年7期
World Journal of Hepatology2019年7期
- World Journal of Hepatology的其它文章
- Wilson disease developing osteoarthritic pain in severe acute liver failure: A case report
- Epidemiology and outcomes of acute liver failure in Australia
- Role of innovative 3D printing models in the management of hepatobiliary malignancies
- Rise of sodium-glucose cotransporter 2 inhibitors in the management of nonalcoholic fatty liver disease
