Superior Vena Cava Occlusion as a Complication of Transvenous Cardiac Device Implantation:A Case Report and Brief Review
Steven J.Ross,MD ,Sahil Prasada,MD ,Hassan Ashraf,MD ,David Wymer,MD and C.Richard Conti,MD
1 University of Florida,Medical School,Gainesville,FL 32610,USA
Abstract
Superior vena cava (SVC) syndrome is a rare complication of transvenous cardiac device implantation,which may lead to delay of diagnosis when symptoms appear.A 68 year-old male with a dual chamber implantable defibrillator implanted 10 years prior presented to an emergency department with symptoms of facial swelling,frequent headaches,and early morning purple facial discoloration.At UF Health,he underwent computed tomographic (CT) scanning of the chest which was consistent with SVC syndrome,presumably a complication related to the prior implantation of his cardiac device.Despite the imaging findings,venography remains the diagnostic modality of choice.Heparinization,catheter-based venography,and catheter thrombectomy with serial balloon angioplasty were performed for recanalization of the SVC,and the patient was ultimately discharged asymptomatic on apixaban for anticoagulation.However,symptoms recurred within two weeks.Ultimately,the patient underwent surgical right internal jugular vein to right atrial bypass with resolution of symptoms.A post-operative CT venogram was performed and the anastomosis was successful.Apparently an angiogram was not done at one year.
Keywords: SVC occlusion;thrombectomy;bypass;Tranvenious atrial pacemaker
Introduction
Superior vena cava (SVC) syndrome is an uncommon complication of transvenous cardiac device implantation that was first described in the 1970s [1,2].As its occurrence is rare,with some estimating the incidence to be < 0.1% of patients undergoing device implantation [3],prompt diagnosis and initiation of appropriate treatment can be challenging.Herein we present a case of SVC syndrome as a complication of transvenous implantable cardioverter-defibrillator (ICD) implantation that highlights some of these diagnostic and management-related challenges.We also provide a brief overview of device-related SVC syndrome and its management.
Case Presentation
A 68 year-old male with coronary artery disease,ischemic cardiomyopathy with an ejection fraction of 30%,and prior cardiac arrest due to ventricular fibrillation 10 years after implantation of a single chamber ICD.The VF was due to rate slowing.A single chamber atrial lead was implanted to prevent slowing of the heart.He now presents to an emergency department with multiple complaints including facial swelling and purple facial discoloration,which had started to occur when lifting weights over his head.
Several months prior to presentation,the patient had begun to notice frequent headaches and occasional purple discoloration on his chest.He believed these symptoms to be due to a vigorous exercise routine and therefore did not seek care immediately.About two weeks prior to his emergency room presentation,his wife had noted facial swelling upon waking in the morning,which tended to resolve as the day progressed.The patient also noted symptoms of worsening exertional dyspnea,hoarseness,and non-productive cough for the few weeks prior to presentation.
The patient was seen initially at an outside facility,where a computed tomographic (CT) scan of his head was unremarkable and he was ultimately discharged without a specific diagnosis.He then presented to UF Health a few days later due to continued symptoms.Upon initial evaluation,the patient was afebrile with a heart rate of 71 and blood pressure of 148/72.The patient was noted to have facial swelling,erythema of his chest wall,and prominent venous distention of the neck and chest on physical exam.The usual blood studies were unremarkable.CT imaging of the chest with contrast showed an occluded SVC,as well as other findings suggestive of SVC syndrome,such as abnormal enhancement of the quadrate lobe of the liver (“ hot quadrate sign”) and left posterior hemithorax collaterals ( Figure 1 ).The patient was started on a full-intensity heparin infusion.Multiple consulting services including vascular surgery,thoracic surgery,interventional cardiology,and electrophysiology were involved in a discussion,and the plan was made to attempt catheter-based SVC venography and balloon angioplasty without stent placement in order to avoid interfering with the preexisting device leads.SVC venography demonstrated complete occlusion of the SVC extending from the junction of the right and left brachiocephalic veins to the SVC entrance into the right atrium ( Figure 2 ).The SVC was recanalized using catheter thrombectomy and serial balloon angioplasty ( Figure 3).The patient' s symptoms improved initially and he was discharged on the direct oral anticoagulant (DOAC) apixaban.

Figure 1 (A) Shows the SVC as dilated and nonopacified and the pacing wires centrally within (blue arrow).Posteriorly we see venous collaterals from the upper extremity to the abdomen due to SVC obstruction (red arrow).(B) Shows contrast opacification of the quadrate lobe of the liver,so-called “ hot quadrate sign” suggestive of SVC syndrome (red arrow).
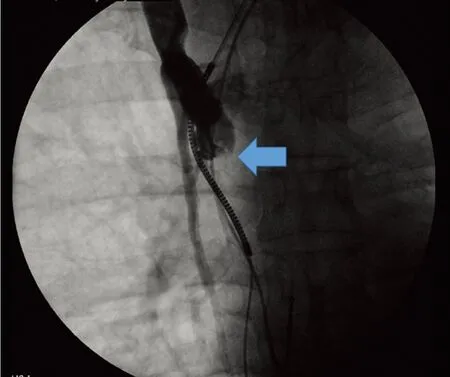
Figure 2 Catheter-based venogram demonstrating occlusion of the superior vena cava (blue arrow).
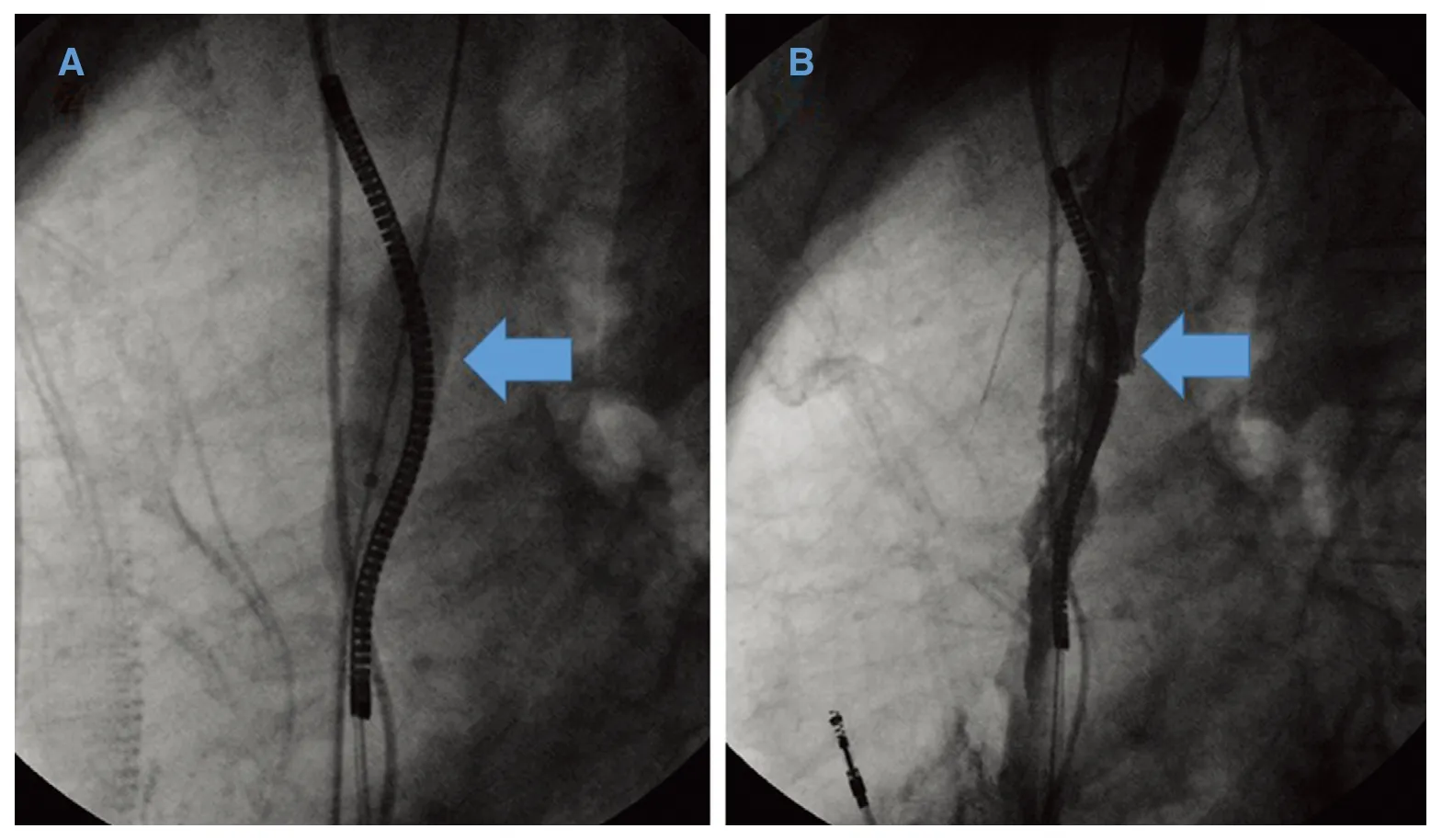
Figure 3 (A) Serial balloon (blue arrow) dilation was used to recanalize the superior vena cava.(B) Superior vena cava with irregular patency restored (blue arrow) after balloon dilation.
Unfortunately,two weeks after the catheterbased procedure the patient experienced recurrent symptoms.He ultimately underwent surgical right internal jugular vein to right atrial bypass,along with explantation of his transvenous device and implantation of an epicardial system.He has been observed for about 1 year since surgery and there have been no recurrent symptoms.An immediate post-operative CT venogram was performed after the surgery ( Figure 4).
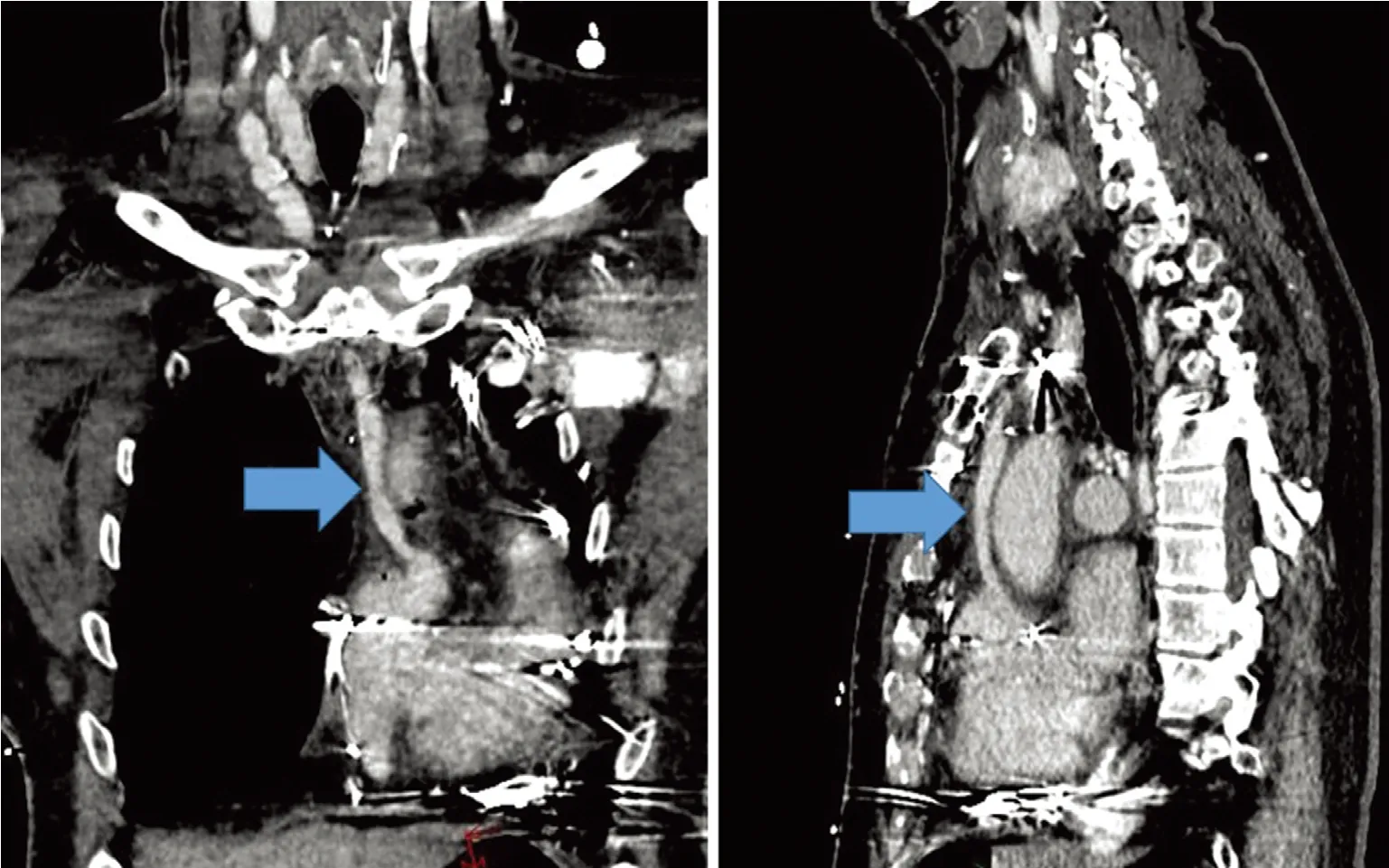
Figure 4 CT venogram showing multiple views of the patent right internal jugular vein to right atrial bypass (blue arrows).
Discussion
The pathophysiology of SVC occlusion after cardiac device implantation is not fully understood,but is thought to be mediated by endothelial damage from pacing wires leading to inflammation,thrombosis,fibrosis,and ultimately venous occlusion [4].Several factors,such as the presence of multiple leads,infection,hormone therapy,pre-existing hypercoagulable state,and others may predispose certain patients to this condition [4 ].Symptomatic presentation is typically weeks to months postdevice implantation,but can occur even years after the procedure,as in the case presented here [4].Early on,partial SVC obstruction can be asymptomatic,but as the degree of obstruction progresses,symptoms and signs classic for SVC syndrome typically occur [4].While facial swelling is the most common complaint,occurring in 82% of patients,other classic symptoms include dyspnea,head fullness or headache,arm swelling,and many other non-specific symptoms such as hoarseness,cough,stridor [5].Classic examination findings include facial edema and venous distension of the neck and chest wall [6].This case demonstrates a classic presentation of SVC syndrome;however,there was a significant delay in diagnosis due to failure of symptom recognition,likely due in part to rarity,and inappropriate initial diagnostic studies.
Diagnosis of SVC syndrome is made clinically based on the patient' s symptoms and examination findings,and confirmed with appropriate imaging studies.CT imaging of the chest can be useful,but in most cases catheter-based venography is necessary to confirm the diagnosis,and is essential for determining the most appropriate therapies [4].
Optimal management of device-associated SVC syndrome is unclear,as the data to this point have been limited to case studies and retrospective analyses.Anticoagulation or thrombolysis with or without extraction of the implanted leads was described initially and remain viable therapeutic options,but as treatment strategies have evolved,these have been replaced with angioplasty,stenting,and surgical options [7].A surgical approach was previously common but eventually gave way to less invasive percutaneous methods [7].As venoplasty alone demonstrated high rates of recurrence,stenting became increasingly used and has now become the most commonly reported method to treat pacemaker-related SVC syndrome [7].Currently,limited data have suggested that the most durable long-term results can be achieved with either stent implantation or surgery,with percutaneous stent implantation being the less invasive,and therefore often preferred option [7].There remains very little available prospective data regarding optimal management and therefore therapeutic decisions should be made on a case-by-case basis.In this case,surgical management was the preferred therapy.
The management of preexisting or retained leads presents an additional challenge.While lead extraction may theoretically reduce the risk of recurrence after recanalization [7],this may not always be feasible.Furthermore,stent implantation without lead extraction would lead to jailing of existing leads,making future lead extraction even more difficult and thereby complicating decision-making.In a pooled analysis by Riley et al.,original pacemaker leads were retained in 72% of patients treated by stenting and in 43% of patients undergoing surgical reconstruction,with no adverse events related to lead erosion reported in the limited follow-up period [7].As it is difficult to draw conclusions due to the limited follow-up,we chose to defer stenting in order to prevent erosion of the previous leads.Unfortunately,with venoplasty and DOAC anticoagulation alone,the patient had symptomatic recurrence less than two weeks later and ultimately required surgical intervention.It is unknown what would have happened if warfarin was used for anticoagulation.Further studies focused on long-term outcomes in patients with jailed and/or retained leads may therefore be helpful in guiding future treatment.
Overall,SVC syndrome remains a rare complication of transvenous cardiac device implantation,and requires an individualized and complex approach to management.Due to its rarity,recognition of the classic presenting signs and symptoms is essential.More research is needed in order to develop a more standardized treatment approach.
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
1.Wertheimer M,Hughes RK,Castle CH.Superior vena cava syndrome.Complication of permanent transvenous endocardial cardiac pacing.J Am Med Assoc 1973;224(8):1172- 3.
2.Chamorro H,Rao G,Wholey MH.Superior vena cava syndrome:a complication of transvenous pacemaker implantation.Radiology 1978;126(2):377- 8.
3.Bolad I,Karanam S,Mathew D,John R,Piemonte T,Martin D.Percutaneous treatment of superior vena cava obstruction following transvenous device implantation.Catheter Cardiovasc Interv 2005;65(1):54- 9.
4.Klop B,Scheffer MG,McFadden E,Bracke F,van Gelder B.Treatment of pacemaker-induced superior vena cava syndrome by balloon angioplasty and stenting.Neth Heart J 2011;19(1):41- 6.
5.Rice TW,Rodriguez RM,Light RW.The superior vena cava syndrome:clinical characteristics and evolving etiology.Medicine (Baltimore) 2006;85(1):37- 42.
6.Nickloes TA,Kallab AM,Dunlap AB.Superior Vena Cava Syndrome:Clinical Presentation [Internet].Medscape;updated 2018 Mar 26.Available from:https://emedicine.medscape.com/article/460865-clinical#b2.
7.Riley RF,Petersen SE,Ferguson JD,Bashir Y.Managing superior vena cava syndrome as a complication of pacemaker implantation:a pooled analysis of clinical practice.Pacing Clin Electrophysiol 2010;33(4):420- 5.
 Cardiovascular Innovations and Applications2019年4期
Cardiovascular Innovations and Applications2019年4期
- Cardiovascular Innovations and Applications的其它文章
- Cardiovascular Innovations and Applications
- Giant Aneurysm of a Coronary-Pulmonary Artery Fistula:A Rare Cause of a Diastolic Murmur
- The Relationship Between Mean Platelet Volume and ln-Hospital Mortality in Geriatric Patients with ST Segment Elevation Myocardial lnfarction Who Underwent Primary Percutaneous Coronary lntervention
- Ultrasound:The Potential Power for Cardiovascular Disease Therapy
- Predictive Value of Resting Pd/Pa for Fractional Flow Reserve Assessed with Monorail Pressure Microcatheter in Real-World Practice
- Systemic Vasculitis:An Important and Underestimated Cause of Malignant Hypertension
