Traumatic axonal injury of the cingulum in patients with mild traumatic brain injury: a diffusion tensor tractography study
Sung Ho Jang, Seong Ho Kim, Han Do Lee,
1 Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
2 Department of Neurosurgery, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
AbstractThe cingulum, connecting the orbitofrontal cortex to the medial temporal lobe, involves in diverse cognition functions including attention, memory, and motivation. To investigate the relationship between the cingulum injury and cognitive impairment in patients with chronic mild traumatic brain injury, we evaluated the integrity between the anterior cingulum and the basal forebrain using diffusion tensor tractography in 73 patients with chronic mild traumatic brain injury (39 males, 34 females, age 43.29 ± 11.42 years) and 40 healthy controls (22 males, 18 females, age 40.11 ± 16.81 years). The patients were divided into three subgroups based on the integrity between the anterior cingulum and the basal forebrain on diffusion tensor tractography: subgroup A (n = 19 patients) - both sides of the anterior cingulum were intact; subgroup B (n= 36 patients) - either side of the anterior cingulum was intact; and subgroup C (18 patients) - both sides of the anterior cingulum were discontinued. There were significant differences in total Memory Assessment Scale score between subgroups A and B and between subgroups A and C. There were no significant differences in diffusion tensor tractography parameters (fractional anisotropy, apparent diffusion coefficient, and fiber volume) between patients and controls. These findings suggest that the integrity between the anterior cingulum and the basal forebrain, but not diffusion tensor tractography parameter, can be used to predict the cognitive function of patients with chronic mild traumatic brain injury. This study was approved by Yeungnam University Hospital Institutional Review Board (approval No. YUMC-2014-01-425-010) on August 16, 2017.
Key Words: mild traumatic brain injury; brain trauma; diffusion tensor tractography; diffusion tensor imaging;cognitive impairment; cingulum; memory; Glasgow Coma Scale; neural regeneration
Introduction
Traumatic brain injury (TBI) is classified as mild, moderate, and severe according to loss of consciousness (LOC),post-traumatic amnesia (PTA), and Glasgow Coma Scale(GCS): mild TBI (mTBI, LOC < 30 minutes, PTA > 24 hours and GCS score: 13-15), moderate TBI (LOC 30 minutes-6 hours, PTA 1-7 days, and GCS score 9-12), and severe TBI(LOC > 6 hours, PTA > 7 days, and GCS score 3-8) (Alexander, 1995; Ruff et al., 2009). mTBI has been reported in 75-85% of patients with TBI (De Kruijk et al., 2001; Styrke et al., 2007; Andelic, 2013). Cognitive impairment is a main sequela of mTBI, with previously reported incidence of more than 30% in mTBI (Stulemeijer et al., 2007; Silver et al.,2009). Many studies investigated injury of the neural tracts associated with cognition such as the fornix, cingulum, and the thalamocingulate tract of the Papez circuit in patients with mTBI (Kraus et al., 2007; Niogi et al., 2008a, b; Rutgers et al., 2008; Maruta et al., 2010; Wu et al., 2010; Mac Donald et al., 2011; Davenport et al., 2012; Shenton et al., 2012;Lee and Jang, 2014; Jang and Kwon, 2015; Kim et al., 2015;Veeramuthu et al., 2015; Yang et al., 2016). However, the relationship between injuries of the neural tracts and cognitive impairment in mTBI has not been clearly elucidated.
The cingulum, connecting the orbitofrontal cortex to the medial temporal lobe, involves in diverse cognition functions including attention, memory, and motivation (Bush et al., 2000). Especially, it is important in memory because it supplies cholinergic innervations to the cerebral cortex by getting cholinergic input from the cholinergic nuclei in the basal forebrain; the medial septal nucleus (Ch 1), the vertical nucleus of the diagonal band (Ch 2), and the nucleus basalis of Meynert (Ch 4) (Selden et al., 1998; Mesulam, 2004; Nieuwenhuys R, 2008; Naidich and Duvernoy, 2009; Hong and Jang, 2010). Anatomically, the cingulum is long and large,and located deep within the brain, and shows less discriminability with adjacent neural structures. Thus, precise assessment of the cingulum using conventional brain MRI was limited.
Diffusion tensor tractography (DTT), which is derived from diffusion tensor imaging (DTI), has recently enabled three-dimensional estimation of the cingulum (Malykhin et al., 2008). A previous study suggested that DTT is superior to DTI for demonstrating the cingulum injury in TBI (Kurki et al., 2014). Many studies using DTT have reported on the cingulum injury in intracerebral hemorrhage, hypoxic-ischemic brain injury, subarachnoid hemorrhage, and TBI (Hong and Jang, 2010; Lee et al., 2012; Kurki et al., 2014; Kwon et al., 2014; Yoo et al., 2014). Regarding mTBI, although many studies have demonstrated the cingulum injury by measuring DTI parameters on DTI, only a few studies using DTT demonstrated the cingulum injury (Kraus et al., 2007; Niogi et al., 2008a, b; Rutgers et al., 2008; Maruta et al., 2010; Niogi and Mukherjee, 2010; Wu et al., 2010; Mac Donald et al.,2011; Davenport et al., 2012; Shenton et al., 2012; Kim et al.,2015; Veeramuthu et al., 2015).
In the current study, we investigated the relationship between cingulum injury and cognitive impairment in chronic mTBI patients using DTT.
Subjects and Methods
Subjects
Seventy-three patients (34 males, 39 females, age 43.29 ±11.42 [range 21-60] years) with mTBI who visited the Rehabilitation Department of Yeungnam University Hospital and 40 healthy subjects who showed no history of previous head trauma, neurologic or psychiatric disease (22 males, 18 females, age 40.11 ± 16.81 [20-58] years) were included in this study. The patients were recruited consecutively with the inclusion criteria: (1) LOC for < 30 minutes, PTA for ≤ 24 hours, and initial GCS score of 13-15 (Alexander, 1995; Ruffet al., 2009), (2) more than 1 month after onset of TBI to rule out the effect of the secondary traumatic axonal injury following mTBI (Povlishock and Christman, 1995; Buki and Povlishock, 2006; Jang, 2010; Kwon and Jang, 2014), (3) age:20-60 years. Exclusion criteria were as follows: (1) no specific lesion on brain MRI (T1-weighted, T2-weighted, and fluid attenuated inversion recovery [FLAIR], (2) patients with any history of previous head trauma, neurologic or psychiatric disease. This study was conducted retrospectively and in accordance with the Declaration of Helsinki and the study protocol was approved by Yeungnam University Hospital Institutional Review Board (YUMC-2014-01-425-010) on August 16, 2017. All participants or patients' guardians signed the written informed consent.
DTT acquisition and analysis
DTT (Amsterdam, The Netherlands) data was obtained at 3.1 ± 2.9 months after the onset of TBI. Imaging parameters were as follows: field of view = 240 mm × 240 mm, repetition time = 10,398 ms, echo time = 72 ms, parallel imaging reduction factor = 2, echo-planar imaging factor = 59 and b =1000 s/mm2, number of excitations = 1, thickness = 2.5 mm.Reconstruction was performed using the fiber assignment continuous tracking algorithm (Philips Extended MR Work Space 2.6.3 [Philips, Amsterdam, The Netherlands]) (Mori et al., 1999; Behrens et al., 2007). To analyze the cingulum, the first region of interest (ROI) was placed on the middle part of the cingulum on the coronal view. The second ROI was placed in the posterior part of the cingulum on the coronal view (Concha et al., 2005). Termination criteria were fractional anisotropy (FA) < 0.15 and angle change > 27o. The FA, apparent diffusion coefficient (ADC), and tract number were measured.
The patients were classified into three subgroups based on the integrity between the anterior cingulum and the basal forebrain on DTT; subgroup A: both sides of the anterior cingulum showed intact continuity to the basal forebrain,subgroup B: either side of the anterior cingulum was discontinued to the basal forebrain, and subgroup C: both sides of the anterior cingulum were discontinued to the basal forebrain (Figure 1A). Among 73 patients, 19 patients belonged to subgroup A (26.0%, ten males, nine females, and mean age 46.4 ± 15.1 years), 36 patients to subgroup B (49.3%, 16 males, 20 females, and mean age 43.0 ± 10.1 years), and 18 patients to subgroup C (24.6%, eight males, ten females, and mean age 43.7 ± 13.3 years). No significant differences in all demographic data were observed between the patient and control groups (Figure 1A: patients, Figure 1B: healthy subjects), and between three patient subgroups (P > 0.05). Demographic data of the patient groups (subgroups A, B, and C)and control group are summarized in Table 1.
Neuropsychological tests
The Wechsler Intelligence Scale (WAIS) [measurement of intelligence and cognitive ability, 0-130 scores] and Memory Assessment Scale (MAS) [comprehensive battery short-term,verbal and visual memory function, 0-120 scores] were used for evaluation of cognitive function (Wechsler, 1981; Williams, 1991). The MAS consisted of total, short-term, verbal,and visual memories (Williams, 1991).
Statistical analysis
SPSS software (version 18.0; SPSS, Chicago, IL, USA) was used for statistical analyses. One-way analysis of variance followed by the Least Significant Difference (LSD) post hoc test was used to detect difference between three patient subgroups (MAS and IQ score, and DTT parameters). Statistical significance was accepted for P-value of < 0.05.
Results
Memory function
The MAS and IQ scores for three patient subgroups are summarized in Table 2. No significant differences in terms of verbal IQ, performance IQ, total IQ, short term MAS, verbal MAS, and visual MAS were observed between three patient subgroups (P > 0.05). On the contrary, significant difference in total MAS was detected between subgroups A and B, and between subgroups A and C (P < 0.05). By contrast, significant difference was not detected between subgroups B and C(P > 0.05).
DTT parameters
The results for DTT parameters of the patient and control groups are summarized in Table 3. Significant differences in terms of FA, ADC, and tract number were observed between the patient and control groups, between three patient subgroups and control group, and between three patient subgroups (P > 0.05).

Table 1 Demographic data of included patients
Subgroup A: Both sides of the anterior cingulum showed intact continuity to the basal forebrain; subgroup B: either side of the anterior cingulum was discontinued to the basal forebrain; and subgroup C: both sides of the anterior cingulum were discontinued to the basal forebrain. LOC: Loss of consciousness; PTA: post-traumatic amnesia; DTT: diffusion tensor tractography.aValues indicate the mean ± SD.

Figure 1 DTT for the cingulum in patients with mild traumatic brain injury and the healthy control.(A) DTT for the cingulum in the subgroup A (both sides (red color:the cingulum on the right hemisphere; yellow color: the cingulum on the left hemisphere) of the cingulum showed intact anterior cingulum and basal forebrain), subgroup B (either side of the cingulum showed discontinuation to the anterior cingulum and the basal forebrain (green arrow)), and subgroup C (both sides of the cingulum were discontinued to the anterior cingulum and the basal forebrain (green arrows)).(B) DTT for the cingulum in a normal subject. DTT: Diffusion tensor tractography; A: anterior.
Discussion
In this study, the relationship between the anterior cingulum injury and cognitive impairment was investigated in patients with mTBI, and the results were as follows: 1) no significant differences in all DTT parameters were observed between the patient and control groups, between each subgroup and the control group, and between three patient subgroups, 2)total MAS scores of the patient group differed according to the integrity of the anterior cingulum with the basal forebrain; in detail, patients with discontinuation of integrity to the basal forebrain in either cingulum showed lower total MAS score than patients with intact integrity in both cingulums. However, no difference was observed between patients with discontinuation in both cingulums and one cingulum in total MAS score. Because the cingulum is the passage of acethylcholine to the cerebral cortex, any discontinuation of this passage appeared to cause memory impairment in terms of total MAS rather than general cognition impairment in terms of IQ (Selden et al., 1998; Mesulam, 2004; Hong and Jang, 2010). Discontinuation of the anterior cingulum indicates traumatic axonal injury because no abnormality was shown in the brain MRI in the patient group (Povlishock,1992; Alexander, 1995; Povlishock and Christman, 1995).
The FA, ADC, and tract number indicate the degree of directionality of water diffusion, the magnitude of water diffusion, and the total number of voxels existing in a neural tract, respectively (Mori et al., 1999; Neil, 2008; Jang et al., 2013). Therefore, our results showed no difference in all DTT parameters for the cingulum between the patient and control groups, between three patient subgroups and the control group, and between three patient subgroups, suggesting that the DTT parameters of the cingulum in mild TBI cannot be used as a marker for traumatic axonal injury of the cingulum in chronic mTBI patients. By contrast, results from the patient subgroup showed that any discontinuation of the anterior cingulum has a lower total MAS score,indicating that the discontinuity of the cingulum to the basal forebrain on DTT configuration can be used as a marker for traumatic axonal injury of the cingulum. The above mentioned difference in the results on DTT parameters and configuration might indicate that DTT configuration is superior to DTT parameters in the diagnosis of the cingulum injury in mTBI patients. Furthermore, these results appeared to be attributed to the fact that the cingulum injury cannot result in an abnormality on DTT parameters because the cingulum is a large and long neural tract. A previous study involving TBI patients (mainly severe TBI: mean LOC was 8.9 days)reported that DTT parameters (FA, ADC, and VN) showed correlation with the IQ or MAS as well as integrity of the anterior cingulum (Baek et al., 2013). We believe that this discrepancy on DTT parameters between two studies can be ascribed to the fact that mTBI patients have milder injury of the cingulum compared with all TBI patients. In addition,our results appeared to coincide with those of Kurki's study,which demonstrated that DTT based analysis of the cingulum, performed from volumes defined by tractography, was superior to measurement of FA value of DTT in TBI patients(Kurki et al., 2014).

Table 2 Correlates of clinical data according to the types of patients
Subgroup A: Both sides of the anterior cingulum showed intact continuity to the basal forebrain; subgroup B: either side of the anterior cingulum was discontinued to the basal forebrain; and subgroup C: both sides of the anterior cingulum were discontinued to the basal forebrain. MAS:Memory Assessment Scale; IQ: Intelligence index. Values indicate the mean ± standard deviation. *P < 0.05 (one-way analysis of variance followed by the Least Significant Difference post hoc test).
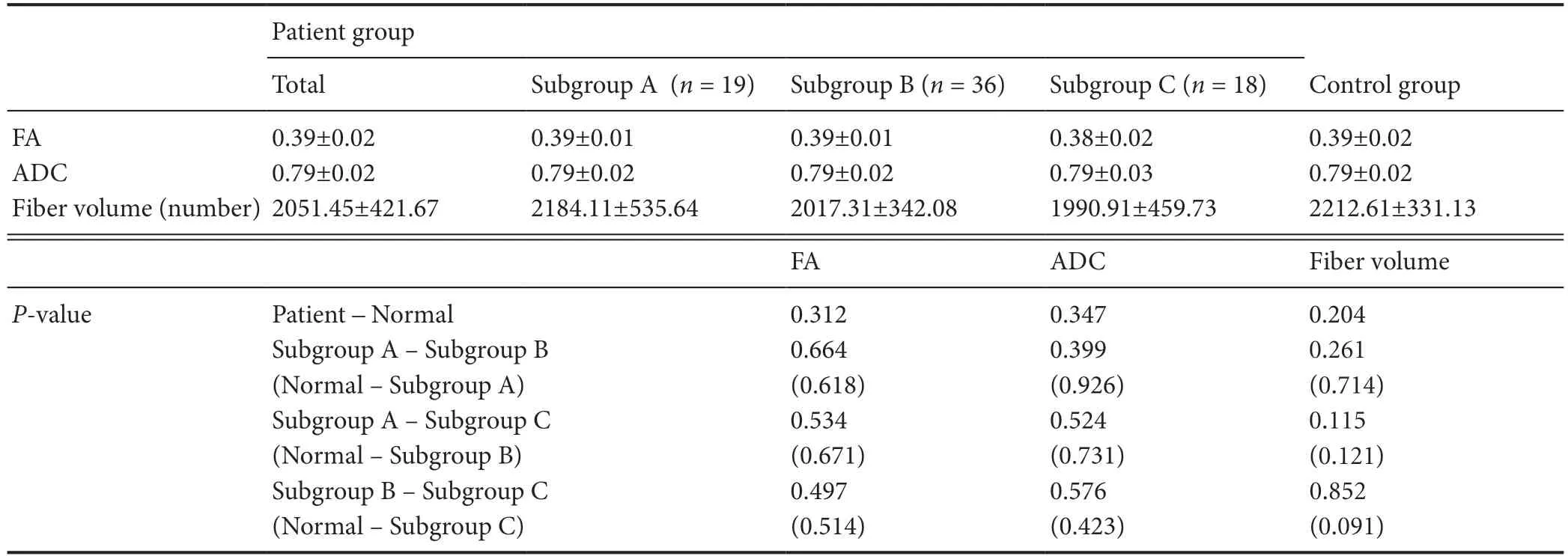
Table 3 DTT parameters in three types of TBI patients and normal controls
Since introduction of DTI, many studies have demonstrated the cingulum injury in mTBI patients (Kraus et al., 2007;Niogi et al., 2008a, b; Rutgers et al., 2008; Maruta et al., 2010;Mac Donald et al., 2011; Davenport et al., 2012; Kim et al.,2015; Veeramuthu et al., 2015). Most of these studies investigated the cingulum injury by measuring DTI parameters two-dimensionally using the ROI method and reported controversial results: no change or significant change in DTI parameters including mainly FA value (Kraus et al., 2007; Niogi et al., 2008a, b; Rutgers et al., 2008; Maruta et al., 2010; Mac Donald et al., 2011; Veeramuthu et al., 2015). A few DTT based studies on the cingulum injury in mTBI have been reported (Davenport et al., 2012; Kim et al., 2015). Davenpot et al. (2012) demonstrated a global pattern of lower white matter integrity including the cingulum using probabilistic DTT in 25 patients with blast-related mTBI. A recent case study reported on three patients who showed bilateral discontinuations of the anterior cingulum on DTT following mTBI (Kim et al., 2015). Therefore, to the best of our knowledge, our study is the first original study to demonstrate the relationship between the integrity of the anterior cingulum to the basal forebrain and memory function in mTBI patients. However, limitation of DTT should be considered: DTT can produce a false negative result throughout the white matter of the brain due to crossing fiber or partial volume effect (Parker and Alexander, 2005). In addition, the fact that we did not confirm the neural injury in the other neural structures which are involved in the memory function is a limitation of this study. Therefore, further studies on this limitation should be warranted.
In conclusion, we investigated the relationship between the cingulum injury and cognitive impairment in chronic mTBI patients and found that the integrity between the anterior cingulum and the basal forebrain, rather than DTT parameters, can play a predictive role in assessing cognitive impairment. This result suggests that DTT would be a useful technique for detection of traumatic fiber injury of the cingulum in chronic mTBI patients, which could not be detected on conventional brain MRI. As a result, DTT reconstruction of the cingulum can be recommended for mild TBI patients who complain of memory impairment.
Author contributions:Concept and design of this study and funding acquisition: SHJ, SHK; data acquisition: SHJ, SHK, HDL; manuscript development and writing: SHJ, SHK, HDL; manuscript authorization:HDL; approval of final manuscript for publication: all authors.
Conflicts of interest:The authors declare that they have no competing interests.
Financial support:This work was supported by the Medical Research Center Program (2015R1A5A2009124) through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (to SHJ and SHK).
Institutional review board statement:Approval for the study was obtained from the Institutional Review Board of Yeungnam University Hospital (approval No. YUMC-2014-1425-010) on August 16, 2017.
Declaration of participant consent:The authors certify that they have obtained the appropriate participant consent forms. In the form the participants or patients' guardians have given their consent for participants'images and other clinical information to be reported in the journal. The participants or patients' guardians understand that participants' names and initials will not be published and due efforts will be made to conceal their identity.
Reporting statement: This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Biostatistics statement:The statistical methods of this study were reviewed by the biostatistician of Yeungnam University in Korea.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Individual participant data will be available(including data dictionaries). All of the individual participant data collected during the trial, after deidentification. Study protocol, statistical analysis plan and informed consent form will be available. Data will be available immediately following publication, no end date. Data are available indefinitely at http://www.nrronline.org.
Plagiarism check: Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Additional file:
Additional file 1:Model Consent Form (Korean).
- 中国神经再生研究(英文版)的其它文章
- Novel miRNA, miR-sc14, promotes Schwann cell proliferation and migration
- Role of behavioral training in reducing functional impairments after stroke
- Remodeling dendritic spines for treatment of traumatic brain injury
- Acute drivers of neuroinflammation in traumatic brain injury
- More than anti-malarial agents: therapeutic potential of artemisinins in neurodegeneration
- Why microglia kill neurons after neural disorders?The friendly fire hypothesis

