Isolation and structural elucidation of antifungal compounds from Curcuma amada
Jesmin Akter, Kensaku Takara, Md. Zahorul Islam, Md. Amzad Hossain,✉, Ayako Sano, De-Xing Hou
1The United Graduate School of Agricultural Sciences, Kagoshima University, Japan
2Faculty of Agriculture, University of the Ryukyus, Japan
Keywords:Curcuma amada Fusarium solani sensu lato Antifungal compounds Zederone Furanodienone Nuclear magnetic resonance
ABSTRACT Objective: To isolate and identify the antifungal compounds from Curcuma amada.Methods: The antifungal activity was measured by the diameter of colonies grown on Petri dish, microscopic observation, and CLSI microdilution methods. The antifungal compounds were isolated through bioactivity guided purification by using silica gel and high-performance liquid chromatography. Structural identification of the antifungal compounds was conducted using 1H NMR, 13C NMR, and liquid chromatography-tandem mass spectrometry.Results: The purified antifungal compounds were zederone and furanodienone. These two compounds showed dose-dependent antifungal activity against Fusarium solani sensu lato. The concentration required for 50% growth inhibition (IC50) of FSSL ranged from 115 to 129 µM and 82 to 91 µM for zederone and furanodienone, respectively.Conclusion: This study suggested that the isolated compounds from Curcuma amada could be promising natural antifungal agents to control the diseases caused by Fusarium solani sensu lato.
1. Introduction
Even with the marked advancement in modern medicine, plants and their derivatives with diverse biological activities are still important sources for the development of new drug. The genus Curcuma includes 80 different species, among which Curcuma amada (C.amada) is less investigated for its pharmacological potentials.C. amada is a perennial, rhizomatous herb belongs to the family Zingiberaceae[1-2]. Morphologically it is resemble to ginger (Zingiber officinale), however the rhizome possesses mango-like aroma for its volatile oil components namely, car-3-ene and cis-ocimene[3-6]. For this it is known as mango ginger[2]. C. amada has a long history of culinary usage in traditional/folk medicine in Asian countries. The rhizome of C. amada has been extensively used as alexteric, appetizer,aphrodisiac, antipyretic and laxative in traditional medicine. Moreover,it shows anti-inflammatory, antifungal, analgesic, anticancer and antihyperglyceridemic properties[7-11]. Some compounds from the rhizome of C. amada particularly, difurocumeninol, amadannulen and amadaldehyde were identified and showed antibacterial, platelet aggregation inhibition, cytotoxicity and antioxidant activities[1,12,13].Furthermore, a labdane diterpene dialdehyde from C. amada showed antitubercular activity[14]. (E)-Labda-8(17), 12-diene-15,16-dial isolated from C. amada and its synthetic triazoles analogues showed strong antiobesity effect via the inhibition of pancreatic lipase[15]. The volatile oils of Curcuma longa, C. amada, Curcuma zedoaria(C. zedoaria) and Curcuma aromatica were effective against various fungi such as Curvularia pallescens, Aspergillus niger, and Aspergillus terreus[14]. The essential oil has been documented against pathogenic fungi of sugarcane such as Physalospora tucumanensis,Sclerotium rolfsii, Helmintho sporium sacchari, Fusarium moniliforme var. subgluti- nans and Cephalosporium sacchari[16]. However, no antifungal compound has been identified from C. amada.
Fusarium solani sensu lato (FSSL) is a pathogenic fungi causes several diseases in human, animals, and plants[17,18]. Many Fusarium fungi produce mycotoxins which are harmful to animals and humans[17]. It causes keratitis, onychomycosis, endophthalmitis,and skin and musculoskeletal infections[19]. In addition, some FSSL species are resistant to commercially available antifungal agents.Usually, synthetic fungicides are used to control pathogenic fungi.However, due to negative impact on the environment and human health, their use is gradually restricted. Moreover, development of resistance to the fungicides is another reason for searching new and safer plant protectants. Plants are promising sources for new natural antifungal drugs, even though they have relatively mild effects against human pathogenic fungi compared with commercial synthetic antifungal drugs.
Recently, we isolated 6 antifungal compounds namely, turmeronol B, turmeronol A, (E)-atlantone, dihydrobisdemethoxycurcumin,demethoxycurcumin and curcumin from Curcuma longa[20]. On the other hand, our previous study reported that C. amada exhibited strong inhibitory effect against FSSL without having the major curcuminoids like curcumin and demethoxycurcumin[21]. Therefore,we hypothesized that there might be some other compounds responsible for its antifungal activity. Hence we aimed to isolate and characterize the active antifungal compounds present in C. amada.
2. Materials and methods
2.1. Chemicals and materials
Methanol (MeOH), ethyl acetate (EtOAc) and n-hexane were purchased from nacalai Tesque (Kyoto, Japan). Silica gel (63-200 µm, Kanto Chemical Co. Tokyo, Japan), MeOH-d4(CD3OD,Merck KGaA, Germany), Potato Dextrose Agar (PDA), Sabouraud Dextrose Agar (SDA) (Becton, Dickinson and Company, France),RPMI-1640 (Life Technologies, USA) and antifungal drug coated plate were purchased from Eiken Chemical Co., Ltd. Tochigi, Japan.
2.2. Microorganism
Four isolates of FSSL (1, 3, 10, and 17) were derived from skin lesions of American manatees (Trichechus manatus) with 3 different genotypes[22]. FSSL 1, 3 and 10 were isolated from the cutaneous lesion of the face (Isolate 1: genotype A, GenBank accession number AB775568) and body skin (Isolate 3: genotype B, GenBank accession number AB775569; Isolate 10: genotype C, GenBank accession number AB775570) of a male manatee-1. FSSL 17 was isolated from palm skin of a male manatee-2 (genotype A, GenBank accession number; AB775568). The genotypes based on internal transcribed spacer 1 – 5.8s – ITS 2 regions of ribosomal RNA gene sequence. The isolates 1 and 17 were genetically identical. However,the sources of the manatee were different, thus we used the above 4 isolates. All the isolates are stored in the Department of Animal Sciences, Faculty of Agriculture, University of the Ryukyus, Japan,maintained in PDA slants and stored at 24–26 ℃. These fungi were subcultured one week before being used for experiments.
2.3. Plant material
C. amada was cultivated in a field of gray soil (coarse sand 3.6%,fine sand 30.9%, silt 24.3%, clay 32.8%, pH 7.4, NO3-N 0.07%,NH4-N 0.08%, P 4.6 ng/g, K 42.9 ng/g)[23] at the Subtropical Field Science Center, University of the Ryukyus, Okinawa, Japan. The average monthly temperature, humidity, and precipitation during the cultivation period were 17–29 ℃, 61%–83% and 22–369 mm,respectively. Rhizomes were harvested on February 10, 2016, when all the shoots of the species withered completely. One and half kilogram of fresh rhizomes were washed, sliced and dried in a hot air oven at 50 ℃ for 72 h. Fine powder of dried rhizome slice was prepared and 300 g powder was used in the experiment.
2.4. Extraction of samples
The extraction was carried out by dissolving 300 g turmeric powder into MeOH at room temperature (25 ℃) with continuous magnetic stirring to prevent oxidation by air and shielding from sunlight. The solvent soluble compounds were filtered using filter paper (No. 2;Advantec, Tokyo Roshi Kaisha Ltd., Tokyo, Japan). Fresh solvents were added into the used plant material and the process was repeated three times. The filtered solutions containing plant compounds were dried on rotary evaporator under reduced pressure at 40 ℃. The yield of extract (26 g) was kept in refrigerator at 4 ℃ for experimental analyses.
2.5. Antifungal assays
2.5.1. Mycelial growth inhibition
To study the effect of different concentrations (32, 64, 128 µg/mL)of C. amada extracts against FSSL (1, 3, 10 and 17 isolates) mycelia growth, sample was incorporated into the fungal growth medium(SDA). After mixing, the amended SDA was dispensed into 9 cm diameter Petri dishes and allowed to cool. Mycelia from 7-day-old culture of FSSL were placed in the center of the Petri dishes. The plates were incubated at 25 ℃ and the radial growth of mycelium was measured after 7 days. The plates without extract were used as control. All tests were performed in triplicate. The relative growth inhibition of the treatment compared to the control was calculated as a percentage, using the following formula:
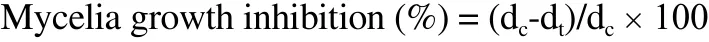
dcand dtrepresent mycelia growth diameter in control and treated Petri plates, respectively.
2.5.2. Hyphal morphology of FSSL
The morphological aspects of FSSL mycelia treated by different concentration (32, 64, 128 µg/mL) of C. amada extracts were examined by an automated inverted fluorescent microscope (Leica, Model No.4000B, Germany). Photomicrographs of the mycelia of FSSL were taken after 48 h of treatment with C. amada extracts and the effect of the extract on hyphal growth was compared with that of control.
2.5.3. Antifungal susceptibilities to commercial compounds
Susceptibility test was performed in a commercially available antifungal drug-coated plate, based on the CLSI standard M38-A2 broth microdilution method[24]. Liquid RPMI-1640 medium buffered to pH 7.0 with 1.0M NaOH, was filter sterilized. Four isolates were cultured on PDA slants at 25 ℃ for 7 days. The inoculum was prepared by rubbing the surface of fungal colonies with 3 mL of sterile liquid RPMI-1640 from PDA slant using a loop. The suspension was then filtered to remove the hyphae and adjusted to a final inoculum of 103colony-forming units/mL using hemocytometer (Neubauer chamber). Seven antifungal drugs including micafungin (MCFG), amphotericin B (AMPB), flucytosine(5-FC), fluconazole (FLCZ), itraconazol (ITCZ), voriconazol (VRCZ),miconazole (MCZ) were used in this study. A total of 100 µL fungal suspensions was added into 96 wells of antifungal drug plates and incubated at 25 ℃. The medium without fungal strain was used as negative control and fungal strain without drugs was used as positive control. After 48 h, hyphal growth was monitored and compared with control. All tests were performed in triplicate. The susceptibility of FSSL isolates was graded inhibitory concentration of 100% (IC100), inhibitory concentration of 50%(IC50) and minimum effective concentration(MEC). The IC100was de fined as the lowest concentration of an agent that completely inhibited the growth of FSSL. IC50was de fined as the lowest concentration of an agent that inhibited approximately 50%of the drug-free growth control. The MEC was defined as the lowest concentration of an agent that led to abnormal growth, such as leading to small, rounded, compact hyphal forms of the fungus. Susceptibilities to amphotericin B, itraconazole and voriconazole were evaluated by IC100.Susceptibility to micafungin was evaluated by the MEC. Susceptibility to flucytosine, fluconazole, and miconazole were evaluated by IC50[24].
2.6. Isolation of bioactive compounds from crude extract of C. amada
The crude extract (26 g) was diluted with 200 mL distilled water and extracted with an equal volume of n-hexane and then with EtOAc. All fractions were concentrated to dryness on rotary evaporator at 40 ℃. Antifungal activity of these three fractions were determined using mycelial growth inhibition assay according to the aforementioned procedure. As EtOAc fraction showed the strongest antifungal activity, it was selected for the isolation and purification of the bioactive compounds. The dried extract from EtOAc fraction was subjected to chromatography on a silica gel (75 g) column (30 cm × 3 cm). Elution was carried out using n-hexane and EtOAc with increasing portion of EtOAc [100:0 (F1), 80:20(F2), 60:40 (F3), 40:60 (F4), 20:80 (F5) and 0:100 (F6) (v/v)].Antifungal activity was carried out on all six fractions and fraction 3 (F3)showed the strongest antifungal activity. For this, F3 was purified by C18 reversed-phase HPLC (COSMOSIL 5C18-AR-II; Nacalai Tesque, Inc.,Kyoto, Japan) eluted with 50% acetonitrile in water (v/v) (50%) at a flow rate of 2.5 mL/min, monitored at absorbance at 280 nm. Three peaks from F3 eluted at 9.55, 13.66 and 16.47 min (Figure 1) as colorless white substances were shown, of which antifungal activity was detected in two peaks fraction eluted at 9.55 and 16.47 min. The isolated compounds (approximately 10 mg each) were dissolved in MeOH-d4and then subjected to spectroscopic analyses. Nuclear magnetic resonance (NMR) spectra were recorded on BRUKER NMR spectrometers (500 MHz for1H and 125 MHz for13C) at room temperature. Chemical shifts (δ) were recorded as parts per million(ppm) relative to tetramethylsilane (TMS) as the internal standard.Mass Spectrometry experiments were carried out on Waters mass spectrometer (Quattro Micro, USA) with an electrospray ionization probe under the following instrumental conditions:Column: COSMOSIL 5C18-AR-II, (2×150) mm. Solvent A: Water(0.1% Formic acid), Solvent B: Acetonitrile, Flow rate: 4 mL/min,Injection volume: 100 µL, Run time: 35 min, Pump mode: Binary gradient. Time program: 75% B (0 min) →75% B (20 min) → 100% B(20.1 min) →100% B (27 min) →75% B (27.1 min) →75% B (35 min).Oven details: CTO-20AC, temperature 40 ℃. MS ionization mode: ES(+), Capillary voltage: 4.0 kV, Cone voltage: 20 V, Source temp.: 120 ℃,Desolvation temp.: 350 ℃, Cone Gas flow: 100 L/h, Desolvation Gas flow:800 L/h.

Figure 1. HPLC chromatogram of F3, detected at the absorbance at 280 nm.
2.7. Antifungal activity of the isolated compounds
Isolated compounds were dissolved in MeOH for making the concentrations of 10, 20, 50, 100 and 500 µM for each compound.Different concentrations of the isolated compounds were incorporated into the fungal growth medium (SDA). After mixing,the amended SDA was dispensed into 9 cm diameter Petri dishes and allowed to cool. Mycelia from 7 days old culture of FSSL were placed in the center of the Petri dishes. The plates were incubated at 25 ℃ and the radial growth of mycelium was measured after 7 days. The plates without compounds were used as a negative control.All the tests were performed in triplicate. The relative growth inhibition of the treatment compared to the control was calculated as a percentage, using the following formula:

Where dcand dtrepresent mycelia growth diameter in control and treated Petri plates, respectively.
2.8. Statistical analysis
Results are expressed as the means ± standard error of the mean(SEM) of three independent experiments. Multiple comparisons were performed using one-way analysis of variance followed by Duncan’s multiple range test. Differences were considered statistically significant at P < 0.05. The concentration required for IC50and isolated compounds in the assay was determined from the regression equation of the concentration response curves. All the experiments were carried out three times.
3. Results
3.1. Mycelial growth inhibition
MeOH extract of C. amada inhibited the growth of all the strains of FSSL in a concentration dependent manner (Figure 2). At 128 µg/mL concentration, C. amada inhibited about 55% growth of all the strains of FSSL. There was no significant difference among these four isolates of FSSL under the same concentration.
3.2. Microscopic observation of hyphal growth
Our result showed that different concentrations (32, 64 and 128 µg/mL) of C. amada had strong effect on the hyphal growth of FSSL (Figure 3).
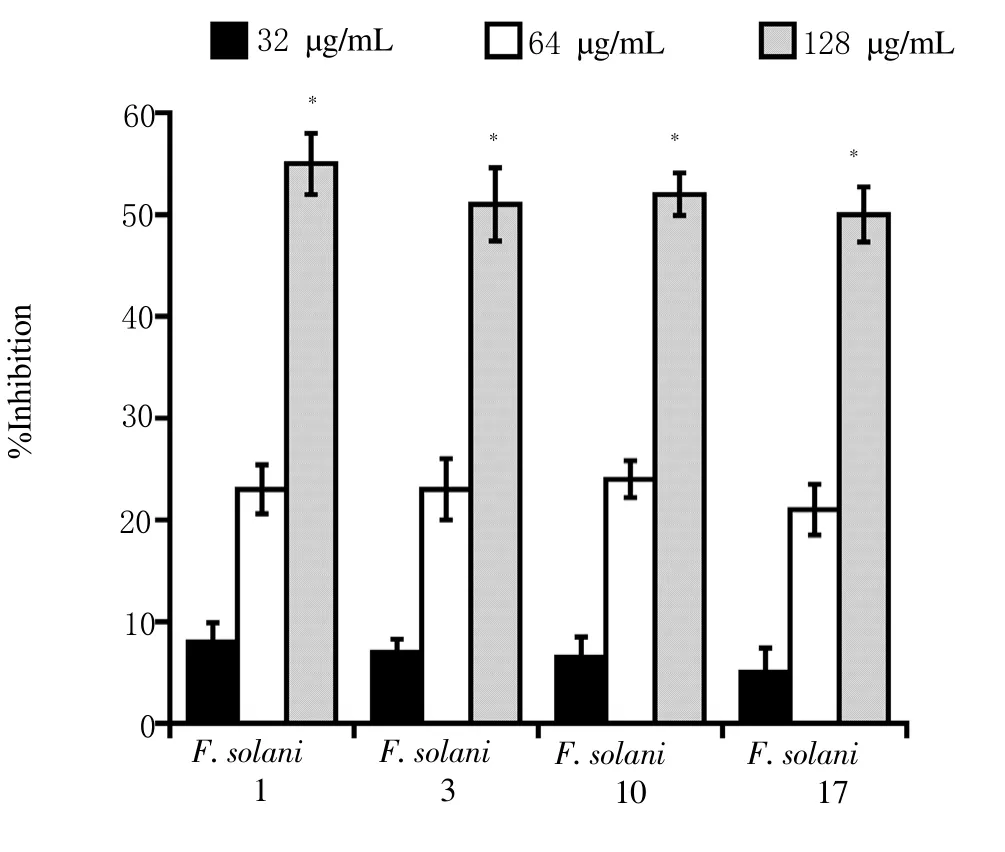
Figure 2. Effect of different concentrations of C. amada on the four isolates of FSSL.
3.3. Antifungal susceptibilities to commercial compounds
Among the 7 commercial antifungal drugs, FSSL were susceptible to AMPB and MCZ. However, FSSL isolate 3 was resistant to AMPB. 5-FC, FLCZ, ITCZ, and VCZ were not effective against FSSL (Table 1).
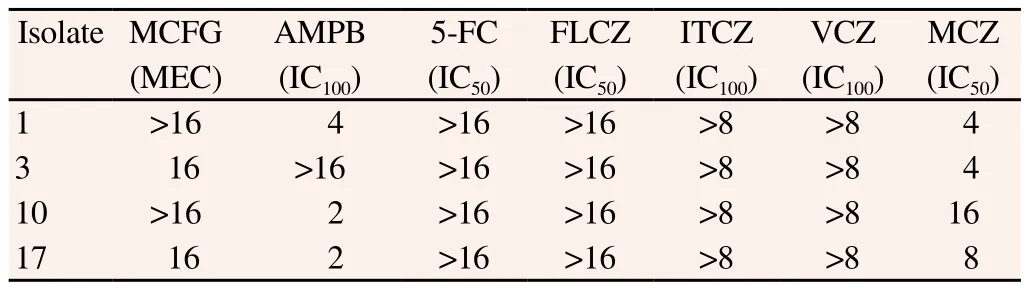
Table 1. Antifungal susceptibilities to commercial compounds evaluated by CLSI method(µg/mL).
3.4. Identification of antifungal compounds
3.4.1. Antifungal activity of water, n-hexane and EtOAc fraction of MeOH extract of C. amada
EtOAc fraction obtained from C. amada resulted in 74% inhibitory activity, which is significantly higher than that of n-hexane and water fraction (49% and 17% inhibitory activity), respectively.
3.4.2. Antifungal activity of different fractions of EtOAc part of C. amada
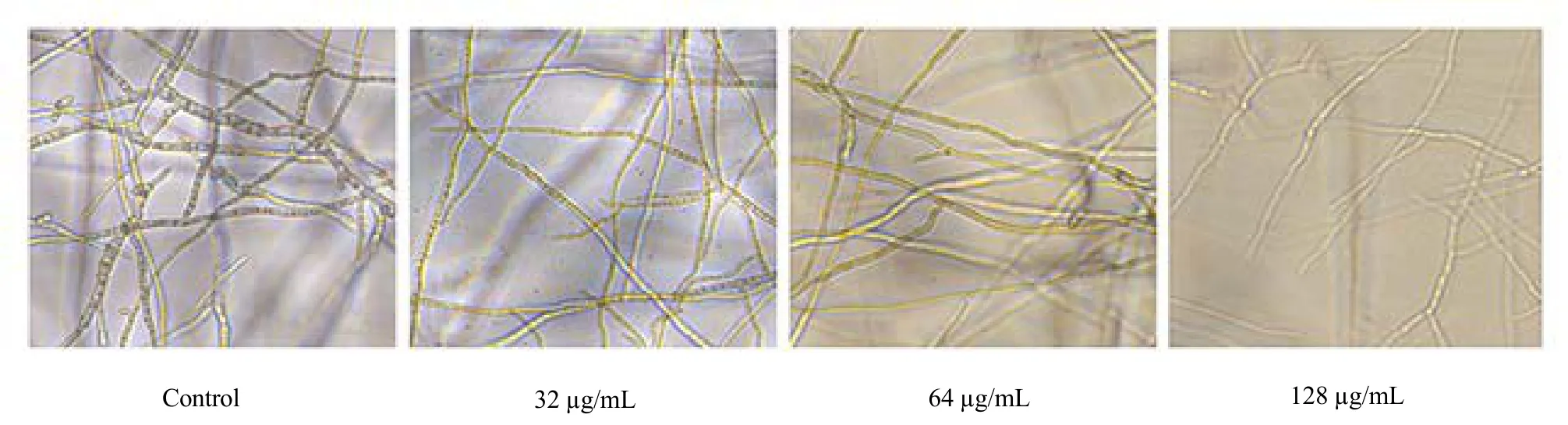
Figure 3. Microscopic examination of the hyphal growth of FSSL (F3) after 48 h of treatment with different concentrations of C. amada.
The antifungal activity of the six fractions [n-hexane: EtOAc;100:0 (F1), 80:20 (F2), 60:40 (F3), 40:60 (F4), 20:80 (F5) and 0:100(F6) (v/v)] differed significantly. Among these, the F3 showed 79%inhibitory activity, whereas the remaining fractions, F1, F2, F4, F5 and F6 resulted in 0.0%, 2.2%, 63.5%, 38.2% and 22.3% inhibitory activity, respectively. The antifungal compounds from F3 showed two effective peaks at 280 nm at a retention time of 9.55 and 16.47 min in the HPLC Chromatogram.
3.4.3.Chemical structures of the isolated compounds
The chemical structures of the two antifungal compounds isolated from F3 were identified according to their1H NMR and13C NMR spectra. Peak data were as follows:
Compound 1: Colourless needle shape crystal, UV λmax: nm 234,285. ESI-MS (+) m/z: 247.3 [M+H]+, 229.4 [M+H-H2O]+.1H-NMR(CD3OD): δ 7.22 (1H, s, H-12), 5.59 (1H, br d, J = 12 Hz, H-1), 3.99(1H, s, H-5), 3.85 (1H, d, J = 16 Hz, H-9a), 3.69 (1H, d, J = 16 Hz,H-9b), 2.57 (1H, dddd, J = 13, 13, 12, 4 Hz, H-2a), 2.26 (1H, m,H-3a), 2.20 (1H, m, H-2b), 2.09 (3H, s, H-13), 1.57 (3H, s, H-15),1.32 (1H, ddd, J = 13, 13, 4 Hz, H-3b), 1.28 (3H, s, H-14).13C-NMR(CD3OD): δ 194.2(C-6) 160.2(C-8), 139.7(C-12), 132.8 (C-1),132.0(C-10), 124.3(C-11), 123.0(C-7), 67.8(C-5), 65.2(C-4), 42.5(C-9),39.0(C-3), 25.4(C-2), 15.7(C-15), 15.4(C-14), 10.7(C-13). From the comparison of these data with those reported in the literature by Giang et al.[25] and Asem et al.[26], the substance was identified as zederone (Figure 4).
Compound 2: Colourless oil, UV λmax: nm 243, 280. ESI-MS(+) m/z: 231.0 [M+H]+, 223.3 [M+H-H2O]+.1H-NMR (CD3OD):δ 7.16 (1H, s H-12), 5.83 (1H, s, H-5), 5.21 (1H, dd, J = 12 Hz, 5 Hz, H-1), 3.73 (1H, d, J = 16 Hz, H-9a), 3.63 (1H, d, J = 16 Hz,H-9b), 2.45 (1H, ddd, J = 15 Hz, 11 Hz, 4 Hz, H-3a), 2.31 (1H, m,H-2a), 2.20 (1H, dddd, J = 12 Hz, 12 Hz, 12 Hz, 4 Hz, H-2b), 2.06(3H, s, H-13), 1.92 (3H, s, H-14), 1.89 (1H, m, H-3b), 1.25 (3H,s, H-15). 13 C-NMR (CD3OD): δ 191.8 (C-6), 158.6 (C-8), 147.6(C-4), 140.0 (C-12), 136.1 (C-10), 133.3 (C-5), 132.0 (C-1), 124.6(C-11), 123.1(C-7), 42.4 (C-9), 41.4 (C-3), 27.3 (C-2), 19.3 (C-14),15.9 (C-2), 9.9 (C-13). From the comparison of these data with those reported in the literature by Dekebo et al.[27] the substance was identified as furanodienone (Figure 4).
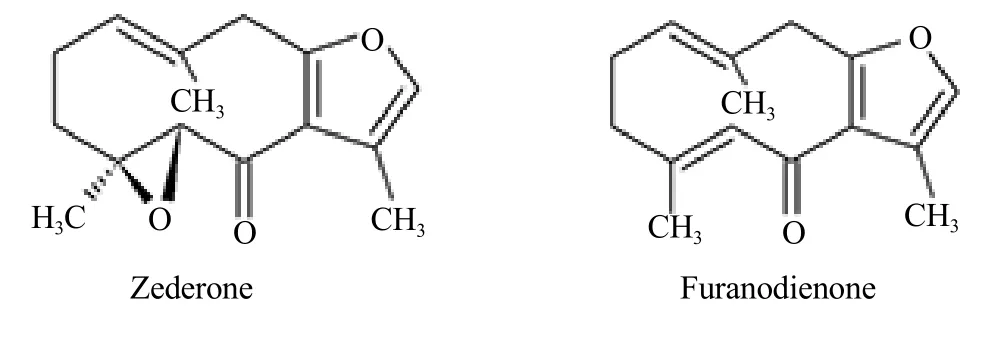
Figure 4. Chemical structures of the two antifungal compounds isolated from C. amada were identified according to their 1H NMR and 13C NMR spectra;zederone (1) and furanodienone (2).
3.5. Antifungal activity of isolated compounds
Two compounds namely zederone and furanodienone were isolated from the fraction F3. The isolated compounds inhibited fungal growth in a concentration-dependent manner. The calculated IC50values of zederone and furanodienone were ranging from (115.0± 5.7) to (129.0 ± 6.0) µM and (82.0 ± 4.8) to (91.0 ± 3.9) µM,respectively for the four genetically different isolates of FSSL(Figure 5).
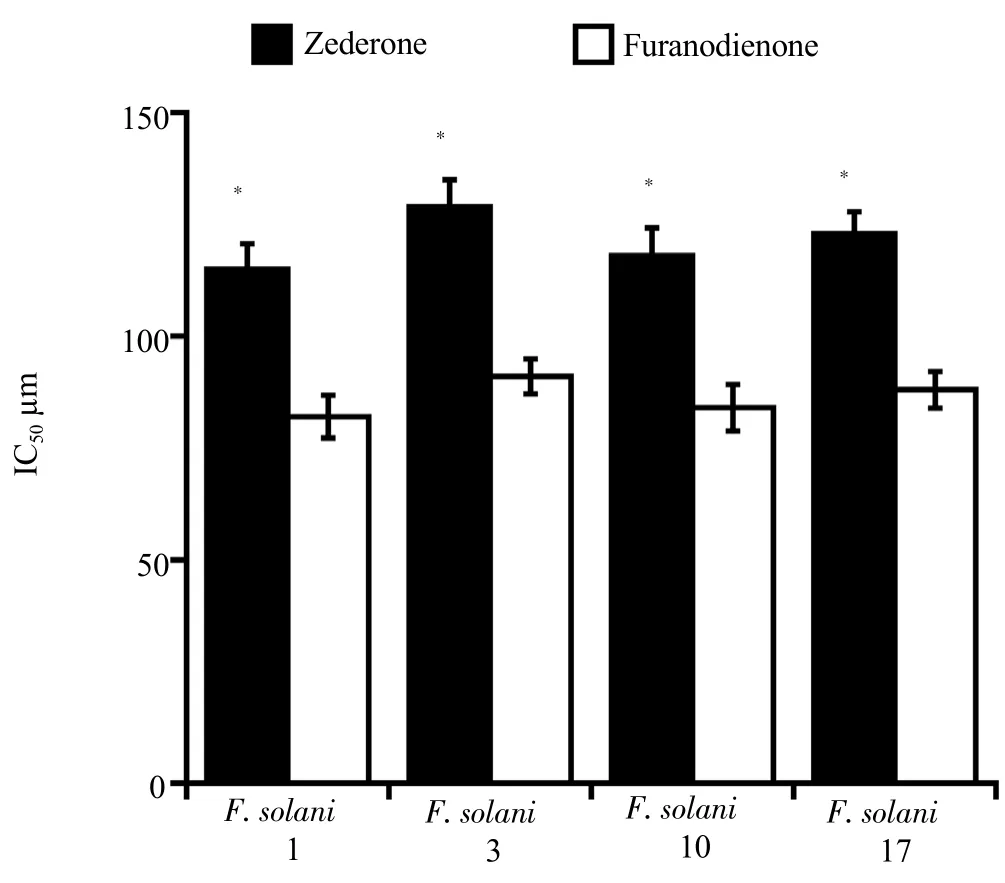
Figure 5. IC50 of zederone and furanodienone on FSSL.
4. Discussion
The present study demonstrated that MeOH extract of the fresh rhizome of C. amada had a dose-dependent inhibitory effect on the hyphal growth of FSSL. For this, we conducted the bioactivity guided purification procedure and identified two antifungal sesquiterpene from C. amada namely, zederone and furanodienone.There are more than 80 species of turmeric have been identified that might be different in their chemical and pharmacological properties.However, researches on turmeric have mainly focused on C. longa and its active compounds such as curcumin, demethoxycurcumin and bisdemethoxycurcumin. We previously reported that there was a significant variation in curcumin, demethoxycurcumin and bisdemethoxycurcumin content in different species and varieties of turmeric[21]. Some of the turmeric for example C. amada did not contain any of these compound. Therefore, researches on different species and varieties of turmeric could explore more pharmacological activities and active compounds. Zederone, a sesquiterpene was previously isolated from C. amada and C. zedoaria and studied its analgesic, anti-inflammatory and cytotoxic effects[28-30]. On the other hand, furanodienone was isolated from Lindera pulcherrima(Nees.) Benth. ex hook. f[31], Curcuma zedoaria[30] and Curcuma wenyujin[32]. It is a furanosesquiterpenoids, exhibited antiinflammatory[30], anti-cancer[33], antibacterial and antioxidant activities[31]. However, we isolated this compound for the first time from C. amada. Though zederone and furanodienone are not newly discovered compounds, their antifungal activity has never been reported. The concentration of zederone and furanodienone was 1.4 and 1.7 µmol/g of dry C. amada, respectively. The IC50of furanodienone was lower than that of zederone. The effectiveness and concentration of furanodienone was 1.4 and 1.2 fold higher than that of zederone. Antifungal susceptibility test showed that FSSL was resistant to the most of the commercially available antifungal agents. Amphotericin B and miconazole were found effective against FSSL. However, FSSL isolate 3 was resistant to amphotericin B. In contrast, our present study suggested that the crude extract and the isolated compounds from C. amada had strong effect on FSSL isolate 3. A few studies have reported antifungal activity of sesquiterpenoid against Fusarium sp. Rufuslactone, a lactarane sesquiterpene, isolated from fruiting bodies of the basidiomycete Lactarius rufus, costunolide, and parthenolide sesquiterpene lactones, from leaves and bark of Magnolia grandiflora, 3-betaacetoxysolavetivone, 3-hydroxysolavetivone, solavetivone, and lubimin sesquiterpenoid from the root of Solanum abutiloides found effective against Fusarium graminearum, Fusarium oxysporum and Fusarium culmorium[34-36]. Beside, antifungal activity, sesquiterpenes have been reported for analgesic, anti-inflammatory, anticancer,antibacterial and antioxidant activities[28-33]. Therefore, our isolated compounds could be the source of alternative natural drug or lead molecules for the synthesis of new drug. Moreover, further pharmacological activity of these compounds could be explored based on the traditional use of their mother plant C. amada.
In conclusion, we strongly suggest that zederone and furanodienone isolated from C. amada can play an important role for controlling diseases caused by FSSL. Further research is necessary to explore their mode and site of action, screening of other pharmacological activities, and synthesis of chemical analogues.
Conflict of interest statement
The authors declare no conflict of interest.
Acknowledgement
We would like to thank Mr. Shinichi Gima, Center for Research Advancement and Collaboration, University of the Ryukyus for his kind assistance in carrying out HPLC analysis.
 Asian Pacific Journal of Tropical Medicine2019年3期
Asian Pacific Journal of Tropical Medicine2019年3期
- Asian Pacific Journal of Tropical Medicine的其它文章
- SARS and its treatment strategies
- Phyllanthus acidus (L.) Skeels and Rhinacanthus nasutus (L.) Kurz leaf extracts suppress melanogenesis in normal human epidermal melanocytes and reconstitutive skin culture
- Antihydatic and immunomodulatory effects of Algerian propolis ethanolic extract: In vitro and in vivo study
- Chemical composition of Mentha suaveolens and Pinus halepensis essential oils and their antibacterial and antioxidant activities
- Status of intestinal parasitic infections among rural and urban populations, southwestern Iran
- X-linked Toll-like receptor 7 polymorphism associated with susceptibility to Chikungunya Fever
