Prevalence and clinical characteristics associated with left atrial thrombus detection: Apixaban
Hoyle L Whiteside, Arun Nagabandi, Kristen Brown, Deepak N Ayyala, Gyanendra K Sharma
Abstract BACKGROUND The prevalence of left atrial appendage (LAA) thrombus detection by transesophageal echocardiogram (TEE) in patients with non-valvular atrial fibrillation (AF) anticoagulated with apixaban is not well defined and identification of additional risk factors may help guide the selection process for pre-procedural TEE. The purpose of our study was to retrospectively analyze the prevalence of LAA thrombus detection by TEE in patients continuously anticoagulated with apixaban for ≥ 4 wk and evaluate for any cardiac risk factors or echocardiographic characteristics which may serve as predictors of thrombus formation.AIM To retrospectively analyze the prevalence of LAA thrombus detection by TEE in patients continuously anticoagulated with apixaban.METHODS Clinical and echocardiographic data for 820 consecutive patients with AF undergoing TEE at Augusta University Medical Center over a four-year period were retrospectively analyzed. All patients (apixaban: 226) with non-valvular AF and documented compliance with apixaban for ≥ 4 wk prior to index TEE were included.RESULTS Following ≥ 4 wk of continuous anticoagulation with apixaban, the prevalence of LAA thrombus and LAA thrombus/dense spontaneous echocardiographic contrast was 3.1% and 6.6%, respectively. Persistent AF, left ventricular ejection fraction < 30%, severe LA dilation, and reduced LAA velocity were associated with thrombus formation. Following multivariate logistic regression, persistent AF (OR: 7.427; 95%CI: 1.02 to 53.92; P = 0.0474), and reduced LAA velocity (OR:1.086; 95%CI: 1.010 to 1.187; P = 0.0489) were identified as independent predictors of LAA thrombus. No Thrombi were detected in patients with a CHA2DS2-VASc score ≤ 1.CONCLUSION Among patients with non-valvular AF and ≥ 4 wk of anticoagulation with apixaban, the prevalence of LAA thrombus detected by TEE was 3.1%. This suggests that continuous therapy with apixaban does not completely eliminate the risk of LAA thrombus and that TEE prior to cardioversion or catheter ablation may be of benefit in patients with multiple risk factors.
Key words: Atrial fibrillation; Anticoagulation; Left atrial appendage thrombus;Transesophageal echocardiography
INTRODUCTION
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is associated with increased risk of systemic thromboembolism due to the development of left atrial (LA) and LA appendage (LAA) thrombi[1,2]. Among patients with nonvalvular AF, 90% of atrial thrombi are seen within the LAA[3]. Transesophageal echocardiography (TEE) is the most sensitive and specific imaging modality for the detection LA thrombi and is routinely utilized in patients undergoing elective cardioversion or catheter ablation to reduce the risk of thromboembolic events[1,2,4-7].Risk factors such as structural heart disease, left atrial size, reduced left ventricular ejection fraction (LVEF), persistent AF, an CHA2DS2-VASc score have been reported as independent predictors of LAA thrombus detection by TEE[8-13].
Several randomized trials have demonstrated the efficacy of non-vitamin K dependent oral anticoagulants (NOACs) to reduce rates of stroke and systemic thromboembolism compared to warfarin, however, their impact on the detection of LA thrombi by TEE is less well established[14,15]. In patients receiving ≥ 3 wk of continuous anticoagulation with warfarin, the prevalence of LA thrombus detection is reported to be between 1.55% and 7.7%[8,12,13,16-20]. Recent data has helped to elucidate the prevalence of LA thrombi in patients anticoagulated with NOACs, particularly in patients prescribed dabigatran or rivaroxaban prior to catheter ablation[18-20]. With regards to apixaban, data remains limited[18-22]. With at least one study reporting a decline in utilization of TEE prior to catheter ablation and prescription rates for NOACs increasing on a yearly basis, further analysis of patients prescribed apixaban could have clinically meaningful implications[22,23]. Identification of additional risk factors which may predict LAA thrombus detection in patients prescribed apixaban is of particular interest as it could help identify a population which would be at increased risk of adverse outcomes should intervention be performed without TEE.
MATERIALS AND METHODS
Study population
Following institutional review board approval, we retrospectively identified 820 consecutive patients with a diagnosis of AF undergoing TEE at Augusta University Medical Center between January 1, 2014 and September 30, 2017 (Figure 1). We excluded 146 patients who were not on any anticoagulation, 183 patients anticoagulated with other NOACs (Rivaroxaban: 122, Dabigatran: 60, Edoxaban: 1),221 patients anticoagulated with Warfarin, and 15 patients who were determined to be incorrectly coded as AF and in whom TEE was performed for an alternative indication. Two hundred fifty-five patients were anticoagulated with apixaban.Within this cohort, 13 patients were excluded due to documented non-compliance with continuous oral anticoagulation in the 4 wk preceding index TEE, 8 for LAA ligation, 2 for valvular AF, and 6 patients with incomplete echocardiographic data.The final study population included 226 patients anticoagulated with apixaban.
Data extraction and baseline assessment
A detailed chart review was conducted in accordance with the study protocol targeting cardiac risk factors, anticoagulant therapy, and echocardiographic data. A CHA2DS2-VASc score was calculated for each patient in accordance with Lip et al[24]AF lasting ≤ 7 d or > 7 d was defined as paroxysmal and persistent, respectively[1,2]. All physician notes in the four weeks preceding TEE were reviewed. Any patient with documented medication noncompliance was excluded from the study.
Cardiac imaging
TEE Imaging was performed using Phillips EPIQ 7 ultrasound machine and Phillips IE33 ultrasound transducer (Andover, Massachusetts). Standard TEE images were acquired including focused imaging of the LA and LAA. Technique routinely used at our institution involves acquisition of at least two orthogonal views of the LAA. All TEEs were reviewed by at least one of two echocardiographers with strong agreement between observers (Cohen’s kappa: 0.89). A thrombus was reported if a wellcircumscribed, echo-reflective mass distinct from the LA endocardium or pectinate muscles was present in the appendage or body of the LA[4]. Spontaneous echo contrast(SEC) was classified as dense, clearing, or absent correlating with 3-4+, 1-2+, or 0 as graded by Fatkin et al[25]SEC was classified as dense if a dense swirling pattern was observed in the LAA and was detectable throughout the cardiac cycle (with variable intensity). SEC was classified as clearing if minimal echodensity was observed in the LAA and was detectable transiently during the cardiac cycle. LAA velocities were determined based on peak velocities averaged over a minimum of two full cardiac cycles in the view which was most parallel to the LAA ostium. LA size was assessed semi-quantitatively and documented as normal, mildly, moderately, or severely dilated.
Follow up
For any patient with LA or LAA thrombi identified on TEE, data was collected for 180 d following index study. If a subsequent TEE was performed between 30 and 180 d following diagnosis of LA or LAA thrombi, then follow up data was collected including changes in oral anticoagulation, antiplatelet therapy, and resolution of thrombus.
Statistical analysis
All statistical computations and hypothesis tests were performed using R 3.4.3(https://www.r-project.org/). To compare demographics and echocardiographic variables between groups, Fisher’s exact test was used for categorical variables and Welch’s t-test was used for the continuous variables. All hypothesis tests were performed at 5% significance level. Univariate logistic regression model was used to associate the odds of occurrence of an event (LAA thrombus formation, dense SEC) to demographic and echocardiographic factors. For scenarios where the odds of the event are zero, pseudo-data points were added to obtain valid estimates and test statistics. Significance of the factors was determined using a two-sided z-test. For each univariate model, a two-sided 95% confidence interval (CI) is reported. Using the variables deemed as significant, a multivariate logistic regression was fit to study independence of the variables.
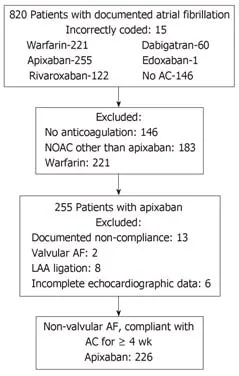
Figure 1 Study population. AC: Anticoagulation; AF: Atrial fibrillation; LAA: Left atrial appendage; NOAC: Nonvitamin K oral anticoagulant.
RESULTS
Population demographics and echocardiographic characteristics
Patient demographics, cardiac risk factors and echocardiographic characteristics for patients with and without thrombus detection are reported in Table 1. The presence of end-stage renal disease, persistent AF, reduced LAA velocities, severe LA dilation,and dense SEC were more common in patients found to have LAA thrombus. Overall,the study population was at meaningful risk of thromboembolic events as 181 (80.1%)patients had CHA2DS2-VASc score ≥ 2.
Prevalence of LAA thrombus and SEC
In patients compliant with apixaban, the prevalence of LAA thrombus and LAA thrombus/Dense SEC was 3.1% and 6.6%, respectively. Full data for the study population based on prevalence of thrombus is provided in Table 1. A similar table,based on the prevalence of thrombus/dense SEC, is available in the online materials(Supplementary Table 1). Among patients with LVEF < 30% and ≥ 50%, thrombus was detected in 9.1% and 2.0% (P = 0.074), respectively. The prevalence of LAA thrombus based on CHA2DS2-VASc score is summarized in Supplementary Table 2. Notably, no thrombi were identified in the 45 (19.9%) patients with a CHA2DS2-VASc score ≤ 1.
Univariate and multivariate predictors of LAA thrombus
In patients anticoagulated with apixaban, persistent AF, LVEF < 30%, severe LA dilation, and reduced LAA velocity were identified as univariate predictors of LAA thrombus detection (Table 2). On multivariate logistic regression, persistent AF (OR:7.427; 95%CI: 1.02 to 53.92; P = 0.0474), and reduced LAA velocity (OR: 1.086; 95%CI:1.010 to 1.187; P = 0.0489) remained independent predictors of LAA thrombus detection. On further analysis, the OR for each 10% decrease in LVEF was 1.517(95%CI: 0.971 to 2.369; P = 0.067). For the combined endpoint of LAA thrombus detection/dense SEC, reduced LAA velocity (OR: 1.131; 95% CI: 1.031 to 1.235; p =0.0061), was a significant independent predictor on multivariate logistic regression with persistent AF (OR: 4.665; 95%CI: 0.81 to 27.0; P = 0.0856) and severe LA dilation(OR: 5.915; 95%CI: 0.74 to 46.98; P = 0.0927) approaching significance (Supplementary Table 3).
Subsequent cardiac imaging and thrombus resolution
Six patients had a subsequent TEE performed 30-180 d following the diagnosis of LAA thrombus and documented compliance with continuous anticoagulation.Anticoagulation and echocardiographic data, as well as, CHA2DS2-VASc score for each patient is provided in Table 3. These patients were anticoagulated for a mean of 94.0 d and thrombus resolution occurred in 83.3%.
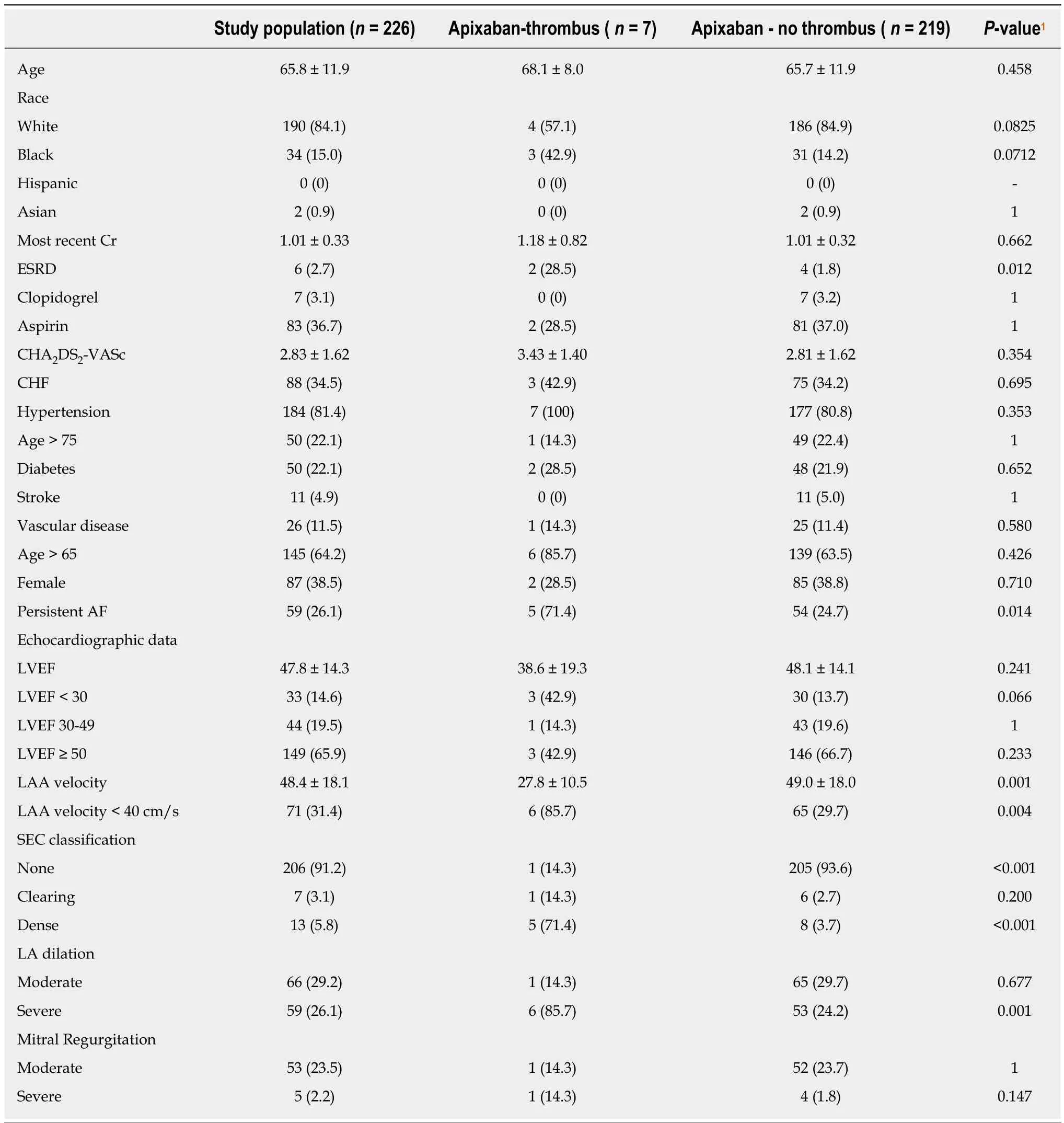
Table 1 Cardiac risk factors and echocardiographic characteristics by presence of thrombus
DISCUSSION
The purpose of our study was to retrospectively analyze the prevalence of LAA thrombus in patients continuously anticoagulated with apixaban for ≥ 4 wk and evaluate for any cardiac risk factors or echocardiographic characteristics which may serve as predictors of thrombus formation.
Prevalence of LAA thrombus detection
To date, there remains limited data on the prevalence of LAA thrombus detection by TEE amongst patients with non-valvular AF on apixaban therapy. Multiple recent retrospective analyses have helped to elucidate the prevalence of LAA thrombus in patients treated with NOACs, in particular, patients undergoing catheter ablation[18-20,22]. However, apixaban is often the least represented oral anticoagulant in these studies with a reported prevalence of 0% to 2.9%[21]. In our study population, the prevalence of LAA thrombus was 3.1% despite ≥ 4 wk of continuous anticoagulation which is consistent with previously published data from smaller cohorts when risk factors are considered. The cohort was at considerable risk given mean CHA2DS2-VASc 2.83 ± 1.62 and 80.1% of patients with CHA2DS2-VASc ≥ 2.
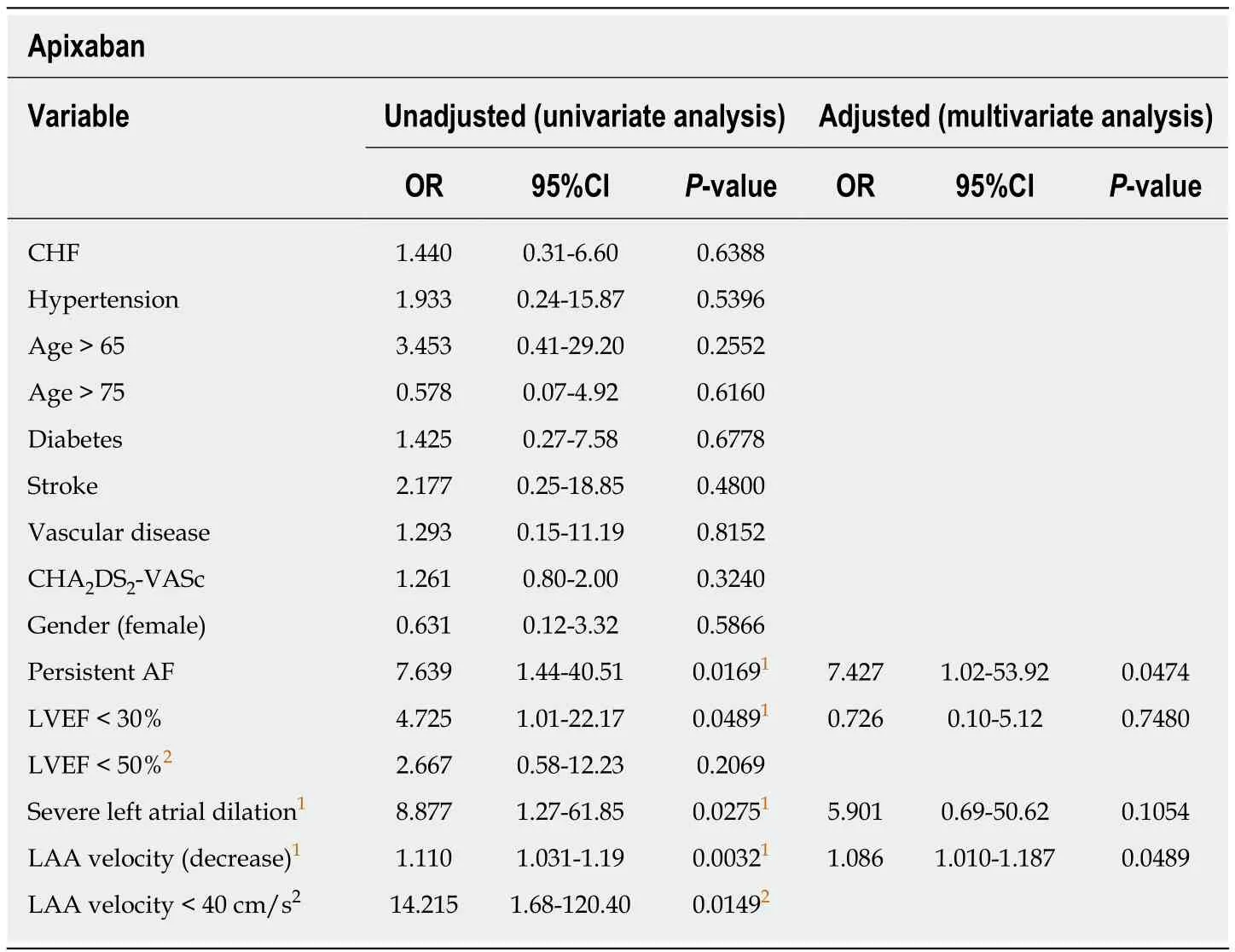
Table 2 Univariate and multivariate predictors of left atrial appendage thrombus
Predictors of LAA thrombus detection
The presence of persistent AF, reduced LVEF, severe LA dilation, and reduced LAA velocity were identified as univariate predictors of LA thrombus detection in the apixaban cohort. Following evaluation with multivariate logistic regression, persistent AF and reduced LAA velocity were identified as independent predictors of LA thrombus detection. Commonly identified independent predictors of thrombus formation in recent studies include CHF, persistent AF, reduced LVEF, and elevated CHA2DS2-VASc score[18-20]. Of note, apixaban was often the least represented NOAC in these studies and made minimal contribution to the population with thrombus.Finally, these analyses pooled vitamin K antagonist and NOAC data in order perform multivariate analysis with one exception, in which the authors describe only 1 independent predictor and report small sample size as a limitation[18-20]. CHA2DS2-VASc score was not identified as a univariate predictor which is likely a result of the relatively small number of low-risk patients in our study population as only 19.9% of patients had CHA2DS2-VASc score < 2. Of note, reduced LVEF < 30% was identified as a significant univariate predictor in both analyses, however was not determined to be a significant independent predictor. We believe that reduced LVEF is a significant predictor of thrombus formation as identified in similar studies with variable anticoagulation strategies and rates of compliance[9,13,19,20]. However, our result likely reflects a limitation of sample size as well as an inherent relationship between advanced cardiomyopathy and clinical/echocardiographic findings most prevalent in high-risk patients with AF.
Rate of LAA thrombus resolution
Data regarding thrombus resolution in patients prescribed apixaban has thus far been limited to case reports and small cohorts[19,20,26,27]. While data regarding thrombus resolution in patients prescribed warfarin is more prevalent, rates of resolution range from 55% to 82%[16,17,28]. In our limited cohort, we identified thrombus resolution in 83.3% of patients anticoagulated with apixaban (n = 6). Although all patients were confirmed to be compliant with continuous anticoagulation throughout the follow up period, there was significant heterogeneity in the duration of therapy prior to repeat cardiac imaging which limits our ability to draw conclusions regarding the optimal duration of anticoagulation. Regardless, apixaban appears to be a reasonable anticoagulation strategy in this population and warrants further investigation in prospective trial.

Table 3 Clinical characteristics and thrombus resolution
Application of study findings
A recent expert consensus statement recommends that current anticoagulation guidelines as they pertain to cardioversion of AF should be observed for patients presenting with AF prior to catheter ablation and that TEE is reasonable despite ≥ 3 wk of continuous anticoagulation[1,2,7]. Two recent surveys, one including 16 Canadian centers and the other including 521 ablation centers in 24 countries, report that > 70%of ablation centers routinely utilized pre-procedure TEE in all patients[29,30]. One costeffectiveness analysis reports an incremental cost-effectiveness ratio of $226608 per quality-adjusted life year for routine use of TEE in an unselected population prior to pulmonary vein isolation modeled with a 4% prevalence of thrombus. While the prevalence is likely overestimated, this analysis highlights the need to better identify patients with a high pretest probability of LAA thrombus despite continuous anticoagulation in order to improve the cost-benefit ratio of the procedure[31]. A trend toward more conservative use of pre-procedural TEE appears to be underway as one large ablation center reports a significant decline in the routine utilization of TEE from 86% to 42% over a 5 year period[22]. While another recent study completely eliminated pre-procedural TEE in favor of intracardiac echocardiography prior to AF ablation.Despite adequate imaging of the LAA in only 71% of patients, the authors report excellent outcomes[32]. This study is retrospective and meant to explore variables which could be predictors of thrombus formation in patients treated with apixaban. A prospective randomized trial would be needed to conclusively determine and validate a scoring system and/or various cutoffs. However, this may not be practical given the low event rate in this population. Nonetheless, we hope that our work can provide evidence to help guide the selection of patients for pre-procedural TEE.
Study limitations
Our study is limited by the retrospective nature of the data collected. In addition, we cannot objectively confirm 100% compliance with apixaban therapy as quantitative assays are not routinely used in clinical practice. Although we took great effort to exclude any patients with documented non-compliance, our ability to do so would be limited by the history provided and documentation of health care professionals.
In patients with non-valvular AF and a minimum of 4 wk continuous oral anticoagulation with apixaban, the prevalence of LAA thrombus and LAA thrombus/dense SEC detected by TEE was 3.1% and 6.6%, respectively. Both persistent AF and reduced LAA velocity were identified as independent predictors of LA thrombus detection in patients anticoagulated with apixaban. In addition, LVEF <30% and severe LA dilation were identified as univariate predictors. We hope that the presence or absence of these clinical findings in addition to established risk factors can help guide the selection process for utilization of pre-procedural TEE in future patients with non-valvular AF anticoagulated with apixaban.
ARTICLE HIGHLIGHTS
Research background
The prevalence of left atrial appendage (LAA) thrombus detection by transesophageal echocardiogram (TEE) in patients anticoagulated for ≥ 4 wk with apixaban is not well defined and predictors of LAA thrombus detection are not completely understood. Furthermore, the efficacy of apixaban to resolve pre-existing LAA thrombi is not well documented.
Research motivation
Prescriptions rates for non-vitamin K dependent oral anticoagulants are increasing on a yearly basis and further analysis of patients prescribed apixaban could have clinically meaningful implications. We aimed to identify significant predictors of LAA thrombus detection on TEE to aid in the selection process for screening in future patients undergoing direct current cardioversion or catheter ablation.
Research objectives
The purpose of our study was to retrospectively analyze the prevalence of LAA thrombus detection by TEE in patients continuously anticoagulated with apixaban for ≥ 4 wk and evaluate for any cardiac risk factors or echocardiographic characteristics which may serve as predictors of thrombus formation.
Research methods
Clinical and echocardiographic data for 820 consecutive patients with atrial fibrillation (AF)undergoing TEE at Augusta University Medical Center over a four-year period were retrospectively analyzed. All patients (apixaban: 226) with non-valvular AF and documented compliance with apixaban for ≥ 4 wk prior to index TEE were included.
Research results
Following ≥ 4 wk of continuous anticoagulation with apixaban, the prevalence of LAA thrombus and LAA thrombus/dense spontaneous echocardiographic contrast was 3.1% and 6.6%,respectively. Persistent AF, left ventricular ejection fraction < 30%, severe LA dilation, and reduced LAA velocity were associated with thrombus formation. Following multivariate logistic regression, persistent AF (OR: 7.427; 95%CI: 1.02 to 53.92; P = 0.0474), and reduced LAA velocity(OR: 1.086; 95%CI: 1.010 to 1.187; P = 0.0489) were identified as independent predictors of LAA thrombus. No Thrombi were detected in patients with a CHA2DS2-VASc score ≤ 1.
Research conclusions
Among patients with non-valvular AF and ≥ 4 wk of anticoagulation with apixaban, the prevalence of LAA thrombus detected by TEE was 3.1%. This suggests that continuous therapy with apixaban does not completely eliminate the risk of LAA thrombus and that TEE prior to cardioversion or catheter ablation may be of benefit in patients with multiple risk factors.
Research perspectives
Compliance with non-vitamin K oral anticoagulants reduces but does not eliminate the prevalence of thrombus detection by TEE. However, available cost-effectiveness analysis reports that pre-procedural TEE is unlikely to be cost-effective in an unselected population. Therefore,there is a need to better identify patients with increased pretest probability of LAA thrombus in order to improve the cost-benefit ratio of the procedure. It is our hope that identification of additional clinical and echocardiographic characteristics; in addition to established risk factors,can help guide the selection process for utilization of pre-procedural TEE