Esophagogastric junction outflow obstruction: Where are we now in diagnosis and management?
Salih Samo, Emad Qayed
Abstract Esophagogastric junction outflow obstruction (EGJOO) is a major motility disorder based on the Chicago Classification of esophageal motility disorders.This entity involves a heterogenous group of underlying etiologies. The diagnosis is reached by performing high-resolution manometry. This reveals evidence of obstruction at the esophagogastric junction, manifested by an elevated integrated relaxation pressure (IRP) above a cutoff value (IRP threshold varies by the manometric technology and catheter used), with preserved peristalsis. Further tests like endoscopy, timed barium esophagram, and cross-sectional imaging can help further elucidate the underlying etiology and rule out mechanical causes.Treatment is tailored to the underlying cause. Similar to achalasia, treatment targeting lower esophageal sphincter disruption like pneumatic dilation, peroral endoscopic myotomy, and botulinum injection are used in patients with functional EGJOO and persistent symptoms.
Key words: Esophagogastric junction outflow obstruction; High-resolution manometry
INTRODUCTION
The invention of high-resolution manometry (HRM) has substantially redefined the landscape of esophageal motility disorders. The assessment of esophagogastric junction (EGJ) obstructive physiology is fundamental in the evaluation of esophageal motility disorders, which is determined by an elevated integrated relaxation pressure(IRP). According to the Chicago Classification of esophageal motility disorders,version 3.0 (CC v3.0), a median IRP threshold of ≥ 15 mmHg on HRM performed in a supine position is indicative of failed deglutitive lower esophageal sphincter (LES)relaxation[1,2]. The cutoff values for IRP are technology dependent and vary per type of instrument (solid-state vs. water perfused). Furthermore, it has been shown that IRP is significantly lower when HRM is performed in the upright sitting position as compared to the supine position[3]. The threshold of 15 mmHg used in the CC is for the Sierra design, which is currently acquired by Medtronic (Medtronic Inc.Minnesota, USA)[1]. The CC categorizes the obstruction at the EGJ into two groups based on peristalsis pattern: 1) achalasia (with its subtypes) with absence of peristalsis and 2) EGJ outflow obstruction (EGJOO) with preserved peristalsis (fragmented or normal). The EGJOO is considered a major motility disorder in the CC[1].
ETIOLOGY OF EGJOO
A variety of conditions can lead to manometric findings consistent with EGJOO.Potential etiologies for EGJOO are summarized in Table 1[4-8]. The majority of these disorders involve mechanical obstruction at the EGJ that could be subtle and missed during the initial evaluation with endoscopy. It is very important to carefully review endoscopic records and consider repeat endoscopy, if warranted, to exclude hiatal hernia, post-surgical changes, and intraluminal processes such as strictures in the distal esophagus and eosinophilic esophagitis (EOE) before labeling someone with functional EGJOO.
PRESENTATION AND DIAGNOSIS OF EGJOO
The EGJOO varies in its presentation. The diagnosis is made on HRM while the patient is usually being evaluated for esophageal symptoms such as dysphagia, chest pain, heartburn and/or regurgitation. However, the diagnosis of EGJOO can be an incidental finding on HRM during evaluation for different indications such as routine manometry prior to anti-reflux procedures[6].
The diagnosis of EGJOO is usually reached after performing endoscopic and functional tests of the esophagus. The evaluation of esophageal symptoms usually begins with upper endoscopy, if not previously performed, to assess for mechanical causes for the presenting symptoms. The endoscopic findings may range from normal upper endoscopy with normal peristalsis and LES, tight LES, esophagitis, hiatal hernia, tumors at the EGJ, and eosinophilic esophagitis (EoE) findings like edema,rings, exudates, furrows, and strictures. It is important to carefully assess the EGJ during endoscopy for any visible lesions or abnormalities on both forward and retroflexed views. A finding of an epiphrenic diverticulum is suggestive of increased EGJ pressure and foam (saliva) and stasis in the esophagus suggests dysmotility. If the endoscopy is unrevealing for a mechanical obstruction, the HRM is the reasonable next test to perform. The HRM findings include an elevated median IRP ≥ 15 mmHg(or a different designated cutoff value based on the device used) of ten supine liquid test swallows with preserved peristalsis (Figure 1). The term “functional EGJOO” is used when there is no obvious mechanical cause for the obstruction. In achalasia, the IRP is elevated, but in contrast to EGJOO, there is failed peristalsis or absence of normal peristalsis[1].
Clinical symptoms and HRM metrics may predict persistence of symptoms in functional EGJOO patients. Presence of dysphagia on presentation and elevated IRP(max 32.1 vs 26.2 mmHg) and distal contractile integral (DCI) (max 10353 vs 5352mmHg.s.cm) on HRM have been shown to predict persistence of dysphagia in patients with EGJOO on follow up[6]. These metrics can also help identify a subset of patients who may benefit from early LES directed therapy. A maximum DCI threshold of 11000 mmHg.s.cm showed a positive predictive value of 82% for identifying patients with dysphagia on follow up. Hence, increasing IRP and DCI suggest a higher likelihood of symptoms persistence. The combination of IRP and DCI metrics in predicting the persistence of symptoms points toward that the symptoms in functional EGJOO are the result of increased resistance at the EGJ with peristaltic dysfunction[6], which may represent early or incompletely expressed achalasia[9]. An IRP cut-off value of ≥ 20 mmHg using Sandhill HRM system and compartmentalized pressurization has been shown to segregate clinically relevant from clinically notrelevant EGJOO. It has also been shown that presence of chest pain with dysphagia increases the likelihood of symptoms persistence and progression to achalasia in EGJOO[10]. An upright IRP > 12 mmHg (using Sierra HRM system) has been demonstrated to be sensitive, although not specific, to detect EGJOO identified on timed barium esophagram (TBE) or present with dysphagia[11].
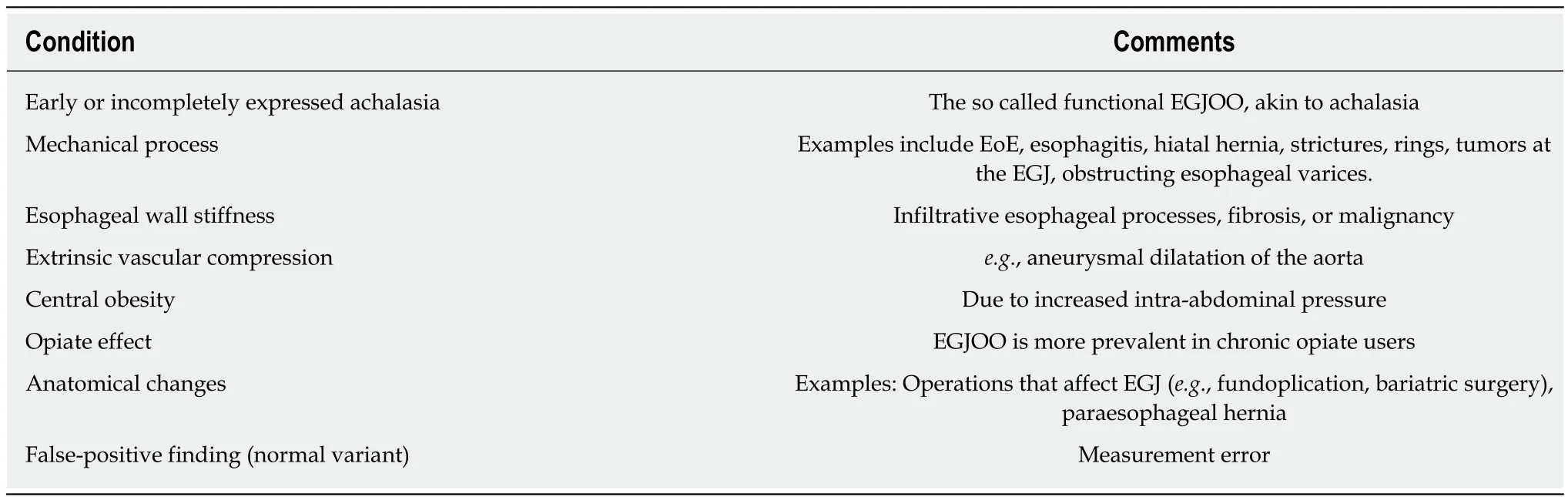
Table 1 Etiologies of esophagogastric junction outflow obstruction
In addition to endoscopy and HRM, other ancillary tests such as TBE, functional luminal imaging probe (FLIP), endoscopic ultrasound (EUS), and computed tomography (CT) scan can further elucidate the obstruction at the EGJ and point to a certain etiology[12]. The TBE is a simple test to perform with low radiation exposure.The patient drinks 100-200 ml of low-density barium sulfate in the upright position.Frontal X-ray images are obtained at 1, 2 and 5 min[13]. TBE has been shown to have its greatest value in differentiating non-treated achalasia from EGJOO/non-achalasia dysphagia. It was shown in a recent study with the barium height of 5 cm at 1 minute to have an excellent accuracy with a sensitivity of 94% and specificity of 71% (AUC =0.915; 95%CI 0.883-0.946; P < 0.0001) in differentiating non-treated achalasia from EGJOO and non-achalasia dysphagia. The diagnostic yield increased to 100% in nontreated achalasia and 60% in EGJOO when 13-mm barium tablet was added to the liquid TBE[14]. Therefore, abnormal TBE with barium tablet retention is an excellent surrogate to diagnose achalasia when HRM is intolerable, not available, or of poor quality. However, it does not eliminate the need for HRM in cases of EGJOO due to poor accuracy of liquid barium to differentiate EGJOO from non-achalasia dysphagia[14]. It is proposed that cutoff values of barium column height (≥ 5 cm at 1 min and ≥ 2 cm at 5 min) to separate untreated achalasia from EGJOO and nonachalasia dysphagia[14].
Another diagnostic test which has not made its way widely to the clinical arena yet is the functional luminal imaging probe (FLIP) technology. FLIP measures the crosssectional area of the esophagus during volume-controlled distension (balloon catheter filled with liquid) which then leads to a software-created high-resolution impedance planimetry with simultaneous measurement of pressure and diameter of the esophagus. This technique assesses the opening dynamics at the EGJ, in addition to esophageal wall stiffness and compliance[15]. However, this technology is not widely available and is limited to esophageal centers of excellence as an exploratory method with data mostly focused on assessment and outcomes in achalasia and EoE[16].
In most cases, a mechanical cause of obstruction at the GE junction can be detected by performing endoscopy and cross-sectional imaging studies[5]. However,Endoscopic Ultrasound (EUS) should be considered as a complementary imaging technique if there is a suspicion of an infiltrating or submucosal tumor of the EGJ or cardia. This is especially true in older individual with relatively recent onset of symptoms (< 6 mo).
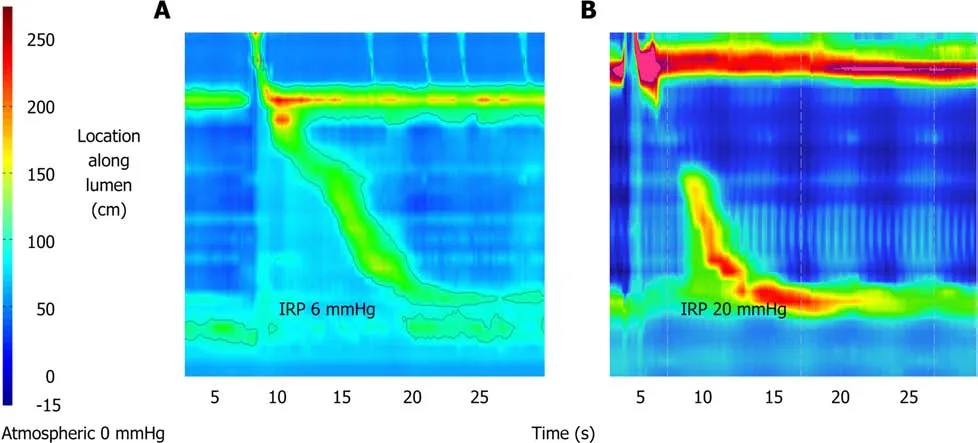
Figure 1 High-resolution manometry image. Panel A represents a normal high-resolution manometry (HRM) image of the esophagus with normal integrated relaxation pressure of 6 mmHg. Panel B represents an HRM image of esophagogastric junction outflow obstruction with IRP of 20 mmHg and reserved peristalsis.
MANAGEMENT OF EGJOO
Since the etiologies of EGJOO are diverse, the treatment strategy relies on accurate diagnosis and treatment of the underlying etiology. Proton pump inhibitors are the treatment for reflux esophagitis and the first step in the management algorithm for EoE before escalating to further therapy such as topical steroids and dietary therapy[17]. Esophageal strictures and rings should be treated with esophageal dilation.Patients with post -fundoplication dysphagia usually respond to redo operations by conversion to partial fundoplication or complete reversal. Functional EGJOO (when no structural abnormality is found) seems to carry a benign course[6,18], especially if it is an incidental diagnosis. In one study, despite that only 15/30 (50%) patients with EGJOO received any specific treatment, 19/30 (68%) patients had symptomatic improvement after a mean follow up period of 30 wk[6]. In another study, among the 13 patients with EGJOO who did not receive any specific therapy, 12 (92%) patients had spontaneous symptomatic resolution of their symptoms over a follow up period of 6 mo[18]. Since asymptomatic or minimally symptomatic cases may resolve without any intervention, observation with a follow up manometry is a reasonable approach before deciding on any therapy directed at the LES in cases of functional EGJOO.When there is retention of barium tablet at the EGJ, bougie dilation to 18-20 mm may be indicated and failure may need to be treated with pneumatic dilation and/or botulinum injection[19]. Peroral endoscopic myotomy (POEM) has shown promise in the management of functional EGJOO when symptoms persist[20], but more data are needed at this time. Pharmacologic management with calcium channel blockers or other drugs that have an effect on smooth muscle relaxation are generally ineffective.Therefore, treatment of EGJOO should be personalized and based on the severity of the patient’s symptoms, age, and local expertise[5]. Figure 2 represents a proposed algorithm for the management of EGJOO.
Choosing which treatment modality to apply in cases of functional EGJOO depends on patient’s factors (overall health condition and patient preference) and availability of center expertise. Botulinum toxin injection adds little time to endoscopy and is safe.Patients my experience chest pain after injection and, rarely, mediastinitis and allergic reaction to egg protein may develop. It is important to note that treatment efficacy of botulinum injection is limited to less than one year and may make subsequent myotomy more difficult[21,22]. Therefore, botulinum toxin injection should be reserved for patients who are poor surgical candidates or unclear diagnosis. Pneumatic dilation has been used for the treatment of achalasia and can be considered in cases of functional EGJOO with persistent symptoms. The initial approach is to start with 30-mm dilator with subsequent dilation using 35-mm dilator (graded dilation) in 2-4 wk if initial dilation was insufficient. When performed by experienced operator following conservative approach, the risk of perforation with PD is < 1%[23]. Graded pneumatic dilation has been shown to be non-inferior to surgical Heller myotomy in term of long-term efficacy[24]. POEM is a novel technique that was shown to be a safe and effective modality (> 90% success rate) for the treatment of achalasia[25,26]. However,post-POEM reflux is a major concern and is frequently seen[8]. Most of adverse events that are associated with POEM are mild and severe adverse events area rare. Serious adverse events are preformation, pneumothorax, and bleeding[27].

Figure 2 A proposed algorithm for the management of esophagogastric junction outflow obstruction. HRM: High resolution manometry; TBE: Time barium swallow; LES: Lower esophageal sphincter; EGJOO: Esophagogastric junction outflow obstruction; DCI: Distal contractile integral; IRP: Integrated relaxation pressure;PPI: Proton pump inhibitor.
CONCLUSION
EGJOO is a distinct motility disorder that encompasses a heterogenous group of underlying etiologies. It is a manometric diagnosis and further adjunctive tests (e.g.,endoscopy, TBE, and CT scan) can help further reveal the cause of the obstruction at the EGJ. The course of action depends on the underling etiology and the therapeutic strategy should be personalized to each individual patient’s case. In cases of functional EGJOO, therapies directed at the LES (e.g., pneumatic dilation, PEOM, and botulinum injections) are usually needed for patients with persistent symptoms.Perhaps the definition of EGJOO needs to be revised based on the manometric predictors and taking into consideration the IRP value in the upright position, as these implicate the course of action regarding treatment and timing of intervention.
 World Journal of Gastroenterology2019年4期
World Journal of Gastroenterology2019年4期
- World Journal of Gastroenterology的其它文章
- lntestinal permeability after Mediterranean diet and low-fat diet in non-alcoholic fatty liver disease
- Endoscopic identification of endoluminal esophageal landmarks for radial and longitudinal orientation and lesion location
- Outcomes of endoscopic sphincterotomy vs open choledochotomy for common bile duct stones
- Treatment for gastric ‘indefinite for neoplasm/dysplasia’ lesions based on predictive factors
- Feasibility of gastric endoscopic submucosal dissection with continuous low-dose aspirin for patients receiving dual antiplatelet therapy
- Adenoma and advanced neoplasia detection rates increase from 45 years of age
