Technical advances in NK cell-based cellular immunotherapy
Fang Fang, Wei Wang, Minhua Chen, Zhigang Tian, Weihua Xiao
1Department of Oncology of The First Affiliated Hospital, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei 230027, China; 2 Hefei National Laboratory for Physical Sciences at Microscale, CAS Key Laboratory of Innate Immunity and Chronic Disease, School of Life Sciences, University of Science and Technology of China,Hefei 230027, China; 3 Institute of Immunology, University of Science and Technology of China, Hefei 230027, China;4Engineering Technology Research Center of Biotechnology Drugs Anhui, University of Science and Technology of China,Hefei 230027, China
ABSTRACT Natural killer (NK) cells represent a promising future for tumor immunotherapy because of their unique biological functions and characteristics. This review focuses on technical advances in NK cell-based cellular immunotherapy and summarizes the developments of recent years in cell sources, genetic modification, manufacturing systems, clinical programs, and outcomes.Future prospects and challenges in NK cell immunotherapy are also discussed, including off-the-shelf NK cell exploitation,automatic and closed manufacturing systems, cryopreservation, and therapies involving regulatory checkpoints.
KEYWORDS Natural killer cell; immunotherapy; adoptive cell transfer; genetic modification
Introduction
Natural killer (NK) cell-based immunotherapies are an attractive approach for treating malignancies because of their characteristic recognition and killing mechanisms1-3. Despite increasing interest in NK cell immunotherapy for cancer,some challenges have emerged. Owing to the low frequency of NK cells in peripheral blood (PB; 10%—15%) and cord blood (15%—20%)4,5, expansion is necessary to obtain them in clinical quantities. Feeder cell-based NK cell expansion systems can be used to obtain highly purified and quantitative products6; however, the use of a feeder cell line may result in unpredictable risks. Although feeder-free NK cell expansion systems are relatively simple, the expansion fold is limited7. Moreover, the transduction efficiency of NK cells varies, ranging from 25% to 50% in NK cell lines8,compared with less than 20% in primary NK cells and 6%—96% in ex vivo expanded NK cells9. The quantity of NK cells in a manufactured batch is not sufficient for multipledose adoptive transfer; thus, it is appropriate to cryopreserve NK cells for clinical use. However, NK cells are more sensitive than T cells to the freeze and thaw process, and the effects of cryopreservation on their cytotoxicity remain controversial10,11. Nevertheless, recent technical advances,including successful generation of stem-cell-derived NK cells,the development of an IL-15 super-agonist that can efficiently activate NK cells without side effects, and impressive clinical results from combination therapy and immune checkpoint inhibitors, have provided great encouragement and an indication of future trends in the development of NK cell immunotherapy.
Development of NK cell manufacturing
Sources of NK cells
Allogeneic or autologous PB cells have traditionally been the major sources of NK cells for immunotherapy. However, this cell population is donor dependent and heterogeneous, and the efficiency of expansion systems varies. Recently, CD34+stem cells from sources such as cord blood and induced pluripotent stem cells (iPSCs) have been used to generate NK cells12,13. Various protocols involving xenogeneic stromal feeder cell lines14or a spin-embryoid body have been used to induce iPSC differentiation12,15, producing more than 1,000-fold expansion of NK cells with purity of ≥ 90%. More importantly, by screening single iPSC clones, this approach provides a genetically defined, homogeneous NK cell population that can be genetically modified and expanded on a large scale to produce multiple doses. Therefore, stem-cellderived NK cells represent a possible means of achieving “offthe-shelf”production, genetic modification, and defined and stable supplementation for NK cell generation.
Optimization of CARs for NK cells
Chimeric antigen receptor (CAR) autologous T cells have shown promising clinical outcomes against hematopoietic malignancies. NK cells have been explored as candidates for CAR engineering, enabling them to be directed to specific targets16. In recent years, several researchers have focused on the optimization of CAR constructs, including the extracellular antigen recognition domain and intracellular costimulatory signaling domain. Previously, CARs were designed to recognize tumor cells using the extracellular part;more recently, the targeting of CARs has focused on suppressor cells in the tumor microenvironment. NK cells engineered with a CAR that recognizes myeloid-derived suppressor cells (MDSCs) with overexpression of molecular NKG2D ligands can efficiently kill intra-tumoral MDSCs.This is a viable way to relieve immunosuppression and support other forms of immunotherapy17. Currently, most intracellular signaling domains of CARs are CD3-ζ chains incorporated with costimulatory signaling domains such as CD28. However, CD28 is not naturally expressed in NK cells,so the function of the CD28 signaling domain in NK cells is not clearly defined. Therefore, CAR constructs in NK cells suited to costimulatory signaling domains are needed.Kaufman’s group reported that CAR constructs in NK cells typically expressing costimulatory signaling domains NKG2D-2B4ζ showed greater capacity to induce NK cell cytotoxicity against targets. Notably, T cells engineered with T-CAR showed better activity than those engineered with NK-CAR12. Optimization of CAR intracellular costimulatory signaling domains is needed, in order to find CARs suited to NK cells and T cells, respectively.
Currently, the NK cell line, PB-NK, and stem-cell-derived NK cells can all be engineered with CARs. However, the efficiency of CAR gene transfer is lower in PB-NK, ranging from 10% to 60%, compared with the NK cell line and stemcell-derived NK cells, which have efficiencies of up to 90%18.Moreover, which type of CAR-NK cell provides the greatest benefit is still the subject of research. The latest report shows that CAR-NK-92 cells have stronger cytotoxic activities compared with CAR-engineered PB-derived NK cells from healthy donors in vivo19. However, NK cell lines must be irradiated before infusion, resulting in reduced cytotoxicity and migration. Overall, CAR-NK strategies require further study.
The extracellular part of CARs is usually a single-chain variable fragment, designed to rely on the antibody. This extracellular part enables the cells to recognize specific antigens only expressed on the target cell surface. However,this recognition model represents a bottleneck in CARengineering of cells. Recently, the T cell receptor (TCR),which can recognize antigenic peptides, has been used to establish a TCR-NK cell. The transgenic NK-92 cell line expressing the CD3 signaling complex acquired a T-cell-like profile and showed pMHC-specific cytotoxic function20.TCR-NK cells can recognize all cellular proteins, enabling them to break through the bottleneck and expanding the range of potential applications.
Expansion systems for NK cells
Stem-cell-derived NK cells generation systems usually have two stages: the hematopoietic progenitor differentiation stage and the NK cell differentiation/expansion stage. Most early studies used two murine stromal cell lines, S17 or M210 in stage 1 and EL08-1D2 or AFT024 in stage 221. However, the heterogeneity of these cell lines limited the clinical use of NK cells derived from such systems. A feeder-free system for differentiation and expansion of NK cells was established recently. This led to the development of a spin-dependent hematopoietic progenitor enrichment system that did not require sorting and could produce about 10 times more progenitor cells compared with a feeder-dependent sorting system. These two systems yielded a 1—2-log expansion of stem-cell-derived CD45+CD56+NK cells in about 4 weeks15.
Most of the protocols for PB-derived NK cell expansion fall into two categories: feeder-cell systems and feeder-free systems. Several type of cells, including EBV-transformed lymphoblastoids and genetically modified HEK293 or K562 cell lines, are used as feeder cells22,23. Genetically modified K562 is used most often. Expression of membrane-bound IL-21 in K562 feeder cells has significantly improved the expansion efficiency to 40,000-fold and the NK cell purity to 95% for 2—3-week cultures24. However, there are safety concerns regarding the clinical application of cancer cellderived feeder cells, although the feeder cells are lethally irradiated before use. Recently, irradiated autologous PBMCs combined with anti-CD16 antibodies have been used as feeder cells, resulting in a greater than 5,000-fold expansion rate23. Furthermore, collected cell lysis particles from feeder cells have been used instead of whole cells for NK cell expansion in vitro and in vivo; this may become an effective alternative to feeder-cell systems25. On the other hand,feeder-free systems based on cytokines and antibodies have been developed to expand NK cells, but their expansion efficiencies range from hundreds- to thousands-fold, and the purity of the resulting NK cells ranges from 30% to 90%.Thus, the major focus for feeder-free NK cell expansion protocols is improving their reliability and efficiency. An IL-15 super-agonist complex, ALT-803, has shown NK cellspecific proliferation and cytotoxicity stimulate activities than its nature form IL-1526. The development of these new artificial stimulators could improve feeder-free NK cell expansion systems and facilitate the production of NK cells of clinical grade in appropriate quantities.
Subsets of NK cells exert different cytotoxicities27.CD56brightNK cells harbor superior antitumor function compared with CD56dimcells28,29in general, although a subset defined as CD56dimFE-1H10-exhibited higher cytotoxicity than their CD56dimFE-1H10+counterparts30. In addition, NK cell subsets with memory or memory-like profiles exhibited robust responses to tumor cells31-33. These NK cell subsets could be exploited to improve NK cell-based immunotherapy, although strategies for their expansion require further study.
Clinical programs for NK cell-based cellular immunotherapy in cancer
NK cell adoptive transfer monotherapy
Owing to the pan-specific tumor cell recognition model of NK cells34, adoptive transfer has been widely used in tumor immunotherapy clinical research. There are several clinical schemes for NK cell adoptive transfer. Some of the reported studies employed a single NK cell infusion scheme, with 1 —10 × 107NK cells/kg35-37, which was sufficient to evaluate safety and NK cell retention in vivo. However, considering that NK cells survive for about 2 weeks in vivo38, a single infusion may not be sufficient to maximize the effect. Other studies employed an infusion scheme of 1 — 4 × 107NK cells/kg three times weekly39; this may guarantee the safety of each return, while increasing the dose of NK cells for total infusion. In addition, an infusion scheme of 1 — 4 × 107NK cells/kg in 2 — 4 infusions once per week was employed40.This infusion scheme may achieve the persistence and quantity of NK cells in vivo required for long-term therapeutic effect. However, this infusion scheme requires a weekly NK cells supply; considering the challenges of NK cells cryopreservation, the feasibility of this scheme is uncertain. Both autologous and allogenic NK cells can be used in adoptive transfer cell therapy. However, the impaired development and function of patient-derived autologous NK cells and cell lines limit the clinical applications41,42.Therefore, allogeneic NK cells have been employed in the majority of clinical trials of NK cell-based adoptive cell transfer43. In addition to allogeneic PB-NKs, stem-cellderived and iPSC-derived NK cells have been developed, and their tumor suppression effects have been confirmed in preclinical models13,44. Clinical trials of stem-cell-derived and iPSC-derived NK cells against tumors are also ongoing(www.clinicaltrials.gov). Therefore, the optimization of the NK cells infusion scheme requires further study.
NK cell monotherapy has different clinical outcomes for different indications. Early clinical trials showed better clinical outcomes for allogeneic NK cell immunotherapy against hematopoietic malignancies, with complete and partial response rates of about 50%, compared with about 20% for NK cell immunotherapy against solid tumors38,45. In recent years, the clinical scheme for NK cells immunotherapy has been optimized, and clinical outcomes have gradually improved (Table 1).
Although NK cell therapy has shown a promising tumor suppressive effect, the clinical outcomes of NK cell monotherapy are still limited. Hence, studies using NK cell therapy in combination with other therapies to maximize effectiveness have become mainstream.
Combinational therapy with NK cell adoptive transfer
In previous studies, NK cell therapy was usually combined with conventional cancer treatments such as chemotherapy or radiotherapy. Patients treated with 2 Gy whole-body irradiation followed by an infusion of 2 × 107NK cells/kg 1 day later had significantly prolonged overall survival46.Patients who received chemotherapy were subsequently infused with 1 — 3 × 107NK cells/kg three times a week,leading to progression-free survival of about 4 months47. For hematological malignancies, NK cell therapy was usually combined with hematopoietic stem cell transplantation(SCT); transferring 1 × 107NK cells/kg 1 — 3 months after allo-SCT transplantation enhanced hematopoietic stem cell engraftment48,49. However, several factors including dosage,intensity, and sequential order affect the outcomes of NK cells therapy. Therefore, increasing attention has focused on NK cell combination therapies in recent years (Table 1).Combined with chemotherapy, infusion of an increased dosage of 5 × 107NK cells/kg prolonged the average disease-free survival time to 23.5 months50. In addition, NK cell infusion 1 week before hematopoietic stem cell transplantation benefited the regeneration of hematopoietic stem cells51. Moreover, patients with hematopoietic malignancies treated with radiotherapy followed by hematopoietic stem cell transplantation and three courses of 1 × 108NK cells/kg achieved 85% remission lasting for about 14.7 months52. Based on the regulation of other cells by NK cells53,54, NK cell therapy can be combined with novel immunotherapies. Copik’s group reported that adoptive transfer NK cells could induce the expression of PD-L1 on tumor cells; thus, NK cell infusion combined with anti-PDL1 treatment could significantly improve the NK cells’ antitumor efficacy, with prolonged NK cell persistence and retention55. However, this has only been shown in animal models, with no clinical trial outcomes reported as yet.
Recently, a case study showed that a combination of radiochemotherapy, NK cell adoptive transfer, and PD-1 inhibition could effectively induce long-term tumor control in a patient with stage IIIb non-small cell lung cancer56.However, NK cell combination therapies require further study and clinical verification.
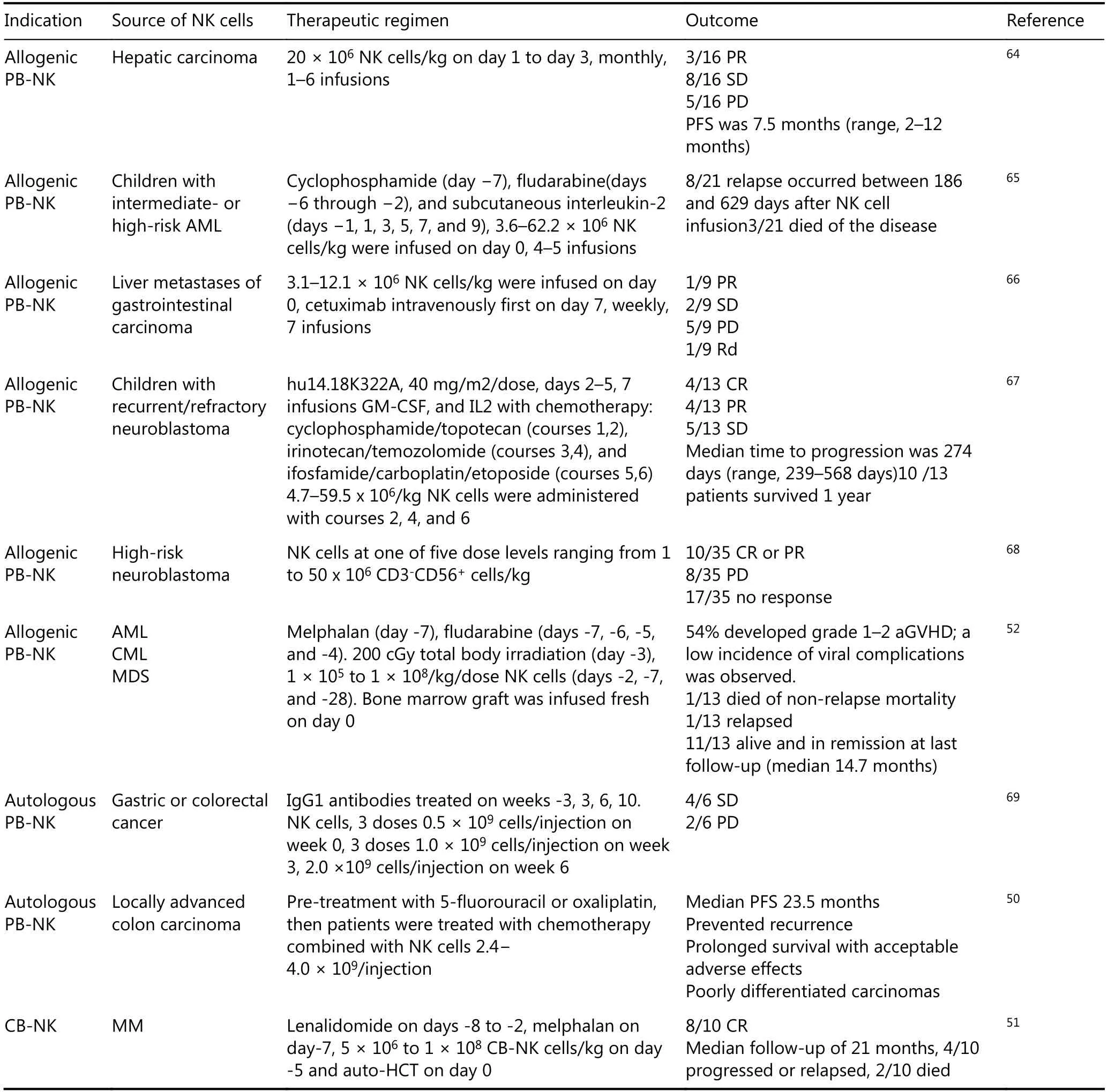
Table 1 Clinical outcomes of NK cell immunotherapy (2017-2019)
Future prospects
Exploitation of off-the-shelf NK cells
Owing to the one-donor, one-patient strategy, the manufacture of clinical grade NK cells is a labor-intensive process. In addition, each batch of cell product may differ in yield, purity, and cell activity. In clinical applications, this requires a huge amount of work on product verification and a resulting lag-time to patient infusion. Although researchers have tried to introduce some criteria to predict or guarantee the success rate of cell production, it remains difficult to guarantee 100% cell infusion in less than 3—5 weeks. This may greatly limit the clinical applications of cell therapy.Therefore, there is a great need for an “off-the-shelf”product. Such a product should have sufficient cells for clinical use, and a clearly illustrated cell profile. Taking into account these quality and quantity criteria, monoclonal CD34+stem cells, including iPSC-derived NK cells, may be suitable candidates. CD34+stem cells are an unlimited NK cell source. NK cells derived from monoclonal CD34+stem cells are homogeneous and can be clearly genetically defined.Kaufman’s group has established a manufacturing system for clinical grade iPSC-derived NK cells. Using genetic modification, they established a CAR-iPSC-NK cell line. A xenograft mouse model showed that CAR-iPSC-NK cell infusion could significantly inhibit tumor growth and prolong survival12. This manufacturing strategy for monoclonal CD34+stem-cell-derived NK cells may represent a feasible off-the-shelf cell product system, although this awaits confirmation through clinical research.
Manufacturing cell products
Currently, NK cells used for preclinical studies or clinical applications are usually cultured in T-flasks or bags.Handling these culture vessels is labor-intensive work and requires highly skilled experts. Using these culture vessels for every batch product leads to low levels of standardization.Thus, there is a great need to explore closed and automatic manufacturing systems, with the aim of achieving highly standardized cell manufacturing and reducing dependency on specialized cell manufacturing centers. Miltenyi Biotech has developed a fully automated, large-scale NK cell expansion system, in which centrifugation, magnetic cell separation, and cell cultivation are performed in a closed system. NK cells produced by this automated system have similar yield and cell function to manually produced NK cells57. Although this system was developed before 2015, its application is not universal. This is probably owing to the diversity of NK cell manufacturing processes with different initial cells, stimulators, and cell passaging principles.Currently, Boya Beijing, Novartis, and Kite Pharma are developing closed and automatic cell manufacturing systems.It is both challenging and necessary to develop an automated system suitable for diverse expansion systems.
NK cells cryopreservation
The condition of a patient, especially in cases of hematopoietic malignancy, may change at any time. It is difficult to guarantee that an NK cell product can be delivered to the patient at the appropriate time during the stable period of NK cell product quality, meaning that every newly started course of NK cell therapy needs the NK cells to be re-produced. Thus, there is a great need for NK cell cryopreservation technologies; these would increase the convenience of NK cell therapy in clinical applications, while reducing production costs and promoting the development of off-the-shelf products. However, current cryopreservation technology for NK cells has some limitations. The optimization of the cryoprotectant formula is ongoing,including the usage and proportion of autologous plasma,dimethyl sulfoxide (DMSO), and plasma substitution58,59. A recent study showed that NK cells cryopreserved using freezing media containing RPMI1640, albumin, dextran, and DMSO retained about 90% viability and had no reduction in cytotoxicity after thawing. Moreover, viability and cytotoxicity were not significantly influenced after thawing when the cells were incubated in the presence of IL-259. This is a promising result for NK cell immunotherapy, although it requires verification.
Investigating the regulatory checkpoints of NK cell therapies to ensure safety and efficacy
Until now, regardless of whether autologous or allogeneic NK cell therapy was used, most clinical trials have shown better safety, less severe uncontrollable graft-versus-host disease (GVHD), and fewer severe adverse effects above grade 4. However, other cells in the final product used for NK cell therapy represent a potential risk in clinical infusion; these include CD4+T cells and B cells. At present, there are no criteria for the composition of NK cell therapy products. It is necessary to establish standards to define the proportion of NK cells and other immune cell subsets to avoid potential risks. NK cells can pan-specifically recognize malignant cells and have a broad-spectrum cytotoxicity to various malignant cells. However, clinical trial outcomes show that NK cell therapy has different effects on different tumors. Activation of NK cell function is determined by the integration of the received activating and inhibitory signals, so the activation trigger of NK cells is partially affected by the number and abundance of activating and inhibitory ligands expressed on the surface of target cells. In addition, various factors including cytokines and immunosuppressive cells in the tumor microenvironment affect NK cell activation and the clinical outcomes of NK cell therapy27,60-63. Therefore, some regulatory checkpoints from the perspective of tumor cells and the tumor microenvironment will be beneficial to improve the outcomes of NK cell therapy. Establishing molecular and cell indices for NK cell therapy will also promote its clinical applications. The overall goal is to maximize the benefits of NK cell therapy while minimizing the risk.
Acknowledgments
This work was supported by grants from the Chinese Academy of Sciences (Grant No. XDB29030201,XBD29030202); the Ministry of Science and Technology of China (Grant No. 2016YFC1303503); the National Natural Science Foundation of China (Grant No. 81788101,81671558, 31571440, 81821001, 91542000); Major Projects of Science and Technology in Anhui Province (Grant No.17030801024) and the Fundamental Research Funds for the Central Universities (Grant No. YD2070002004).
Conflict of interest statement
No potential conflicts of interest are disclosed.
 Cancer Biology & Medicine2019年4期
Cancer Biology & Medicine2019年4期
- Cancer Biology & Medicine的其它文章
- Interpretation of breast cancer screening guideline for Chinese women
- Breast cancer screening guideline for Chinese women
- Erratum to Simultaneous inhibition of PI3Kα and CDK4/6 synergistically suppresses KRAS-mutated non-small cell lung cancer
- The correlation and overlaps between PD-L1 expression and classical genomic aberrations in Chinese lung adenocarcinoma patients: a single center case series
- Nomogram based on albumin-bilirubin grade to predict outcome of the patients with hepatitis C virus-related hepatocellular carcinoma after microwave ablation
- Omics-based integrated analysis identified ATRX as a biomarker associated with glioma diagnosis and prognosis
