Effects of traditional Chinese medicine nursing combined with conventional nursing in patients with chronic obstructive pulmonary disease: a meta-analysis
Chen-Yang Li, Yan-Hui Liu*, Yu-Nan Ji, Ling-Li Xie, Zhen-Hua Hou
Postgraduate College, Tianjin University of Traditional Chinese Medicine, Tianjin 300193, China
1. Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable, and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation resulting from airway and/or alveolar abnormalities that are usually caused by significant exposure to noxious particles or gases, as defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD).1Globally, because of continued exposure to COPD risk factors and population aging, the COPD burden is expected to increase in the coming decades.2COPD is a systemic disease that is associated with a wide variety of symptoms and affects patients’ physical, psychological, and social conditions.3COPD presents high morbidity and mortality but can be decreased by proper treatment and conventional care or traditional Chinese medicine (TCM)nursing.
With the development of TCM, TCM nursing is becoming increasingly widely used in clinical practice, including in patients with COPD. Chinese medical care researchers have explored involving TCM nursing theory, education, management, practice, and so on to promote the development of TCM nursing. Currently,the clinical efficacy of conventional nursing has been recognized. There are a considerable number of nonrandomized trials and randomized controlled trials (RCTs)involving the comparison of TCM nursing combined with conventional nursing and conventional nursing alone.The sample size in current studies is limited and multicenter trials are lacking, making the evidence of TCM nursing combined with conventional nursing unreliable and lacking power.
The aim of this study was to compare the effects of TCM nursing combined with conventional nursing with conventional nursing alone in patients with COPD. The meta-analysis allows clinical outcomes to be quantified for evaluating the advantages of TCM nursing combined with conventional nursing.
2. Materials and methods
2.1 Inclusion and exclusion criteria
Criteria for inclusion and exclusion of studies were established according to the participants, interventions,comparisons, outcomes, and study design (PICOS)principles. The inclusion criteria were as follows: (1) participants: all of the included participants had a diagnosis of COPD, according to the guidelines for the diagnosis and treatment of COPD and received conventional Western medicine; (2) interventions: the participants in the study group were treated with TCM nursing combined with conventional nursing. Conventional nursing involves daily care, dietary nursing, activity nursing, oxygen therapy, assistance with coughing, condition observation, medication care, and health education. TCM nursing, characterized as dialectical nursing, includes dietetic care, emotional nursing, physical therapy of TCM, TCM health education, and TCM rehabilitation training; (3) comparisons: participants in the control group received conventional nursing; (4) outcomes: the study should have reported at least one of the following clinical outcomes: St. George’s Respiratory Questionnaire (SGRQ) score, pulmonary function index (forced expiratory volume in 1 second [FEV1], FEV1/forced vital capacity [FVC], FEV1%, and FEV1 predicted value),hospital stay, and clinical efficacy; and (5) study design:RCTs aimed at studying the effect of TCM nursing intervention on the clinical outcome of patients with COPD.Exclusion criteria were as follows: (1) literature was not designed rigorously; (2) the control group was not designed in the literature; (3) data in the literature were unknown; or (4) relevant data could not be extracted from the literature. For literature that was duplicated or reported by the same research institution, publications with higher quality or more detailed data were included.
2.2 Search strategy
A literature search was conducted in a variety of electronic databases, including PubMed, Embase, Cochrane Library, Web of Science, Google Scholar, China National Knowledge Infrastructure (CNKI), WanFang Data (WF)and VIP, for research published before January 2017.The following terms or keywords were used ((“pulmonary disease, chronic obstructive” [MeSH Terms] OR(“pulmonary”[All Fields] AND “disease”[All Fields] AND“chronic” [All Fields] AND “obstructive” [All Fields]) OR“chronic obstructive pulmonary disease” [All Fields] OR(“chronic”[All Fields] AND “obstructive” [All Fields] AND“lung” [All Fields] AND “disease” [All Fields]) OR “chronic obstructive lung disease” [All Fields] OR “chronic obstructive pulmonary disease” [All Fields] OR “COPD”[All Fields]))AND ((“medicine, Chinese traditional” [MeSH Terms] OR (“medicine” [All Fields] AND “Chinese” [All Fields] AND “traditional”[All Fields]) OR “Chinese traditional medicine”[All Fields] OR (“traditional” [All Fields]AND “Chinese” [All Fields] AND “medicine” [All Fields])OR “traditional Chinese medicine” [All Fields] OR “TCM”[All Fields]) AND (“nurses” [MeSH Terms] OR “nurses”[All Fields] OR “nurse” [All Fields] OR care [All Fields])).No language restrictions were followed.
2.3 Quality assessment
The Jadad scale4was used to assess the quality of the selected publications that met the inclusion criteria. All of the eligible RCTs were assessed by three reviewers(Chenyang Li, YuNan Ji, and ZhenHua Hou) independently. The criteria of Jadad were as follows: (1) Generation of random sequences (appropriate: 2 points; unclear:1 point; inappropriate: 0 points); (2) Allocation concealment(appropriate: 2 points; unclear: 1 point; inappropriate: 0 points; unused: 0 points); (3) Double blinding (appropriate: 2 points; unclear: 1 point; inappropriate: 0 points); and(4) Withdrawal (describes the number and rationale for the withdrawal: 1 point; The number and rationale of withdrawal are not described: 0 points). Four aspects of the evaluation quality were used: 1–3 points were regarded as low quality, and 4–7 points were regarded as high quality.
2.4 Data extraction
Two investigators (Chenyang Li and Lingli Xie) extracted the data independently. The following data were extracted from each publication: first author, year of publication, type of study, selection criteria, age, number of participants, randomness in method, SGRQ scores,pulmonary function, hospital stay, and clinical efficacy.
2.5 Statistical analysis
Meta-analysis was performed using Stata12.0 software(StatCorp, College Station, TX, USA). Weighted mean differences (WMDs) were used to compare SGRQ scores,pulmonary function, and hospital stay. Clinical efficacy was compared using odds ratios (ORs), and subgroup analysis was performed. Statistical heterogeneity was evaluated by the use of Cochran Q and I2statistics. A value of P≤0.10 was considered statistically significant, and a randomeffect model was used. Otherwise, a fixed-effect model was used. Begg’s test and Egger’s linear regression test were performed to evaluate the publication bias.
3. Results
3.1 Study selection and characteristics
Using the search strategies described, 753 potential articles were initially retrieved, and 662 studies were excluded after screening the titles. Fifty studies(reviews or case reports) were excluded after assessing the abstracts. Upon full-text review, 18 reports were excluded because the control groups were missing.Therefore, 23 studies were eligible for this meta-analysis (Figure 1); the characteristics and quality assessment of eligible studies are shown in Table 1. These eligible articles involved 3116 participants (TCM nursing combined with conventional nursing group: 1559,conventional nursing group: 1557). All included studies were reported in the Chinese language.
3.2 Statistical results
3.2.1 SGRQ scores
Four studies5-8reported indications for SGRQ scores,and a fixed-effect model was used for studying interstudy heterogeneity (I2= 0.0%, P=0.990). TCM nursing combined with conventional nursing was associated with lower SGRQ scores than conventional nursing(WMD = –15.06, 95% confidence interval [CI]: –16.56 to–13.55, P=0.000) (Table 2).
3.2.2 Pulmonary function
Significant heterogeneity was observed in six studies8-13that reported data on the FEV1 value (I2= 95.7%, P=0.000),11 studies6-10,12-17that reported data on the FEV1/FVC value (I2= 96.2%, P=0.000), and four studies8,14,15,18that reported data on the FEV1% value (I2= 97.8%, P=0.000);a random-effect model was used for analysis. There was a higher FEV1 value (WMD = 0.29, 95% CI: 0.13–0.45,P=0.000), a higher FEV1/FVC value (WMD = 4.95, 95% CI:2.71–7.19, P=0.000), and a higher FEV1% value (WMD =9.20, 95% CI: 4.71–13.68, P=0.000) compared with those with conventional nursing (Table 2). Four studies6,7,16,17reported data on the FEV1 predicted value; the FEV1 predicted value in TCM nursing combined with conventional nursing was higher than that in conventional nursing alone(WMD = 4.13, 95% CI: 3.44–4.82, P=0.000) with interstudy heterogeneity (I2= 0.0%, P=0.725) (Table 2).
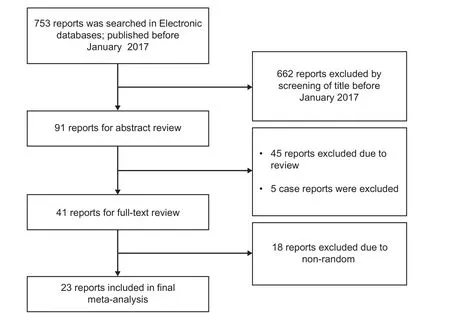
Figure 1. Flow chart of eligible studies.

Table 1. Study characteristics and inclusion criteria
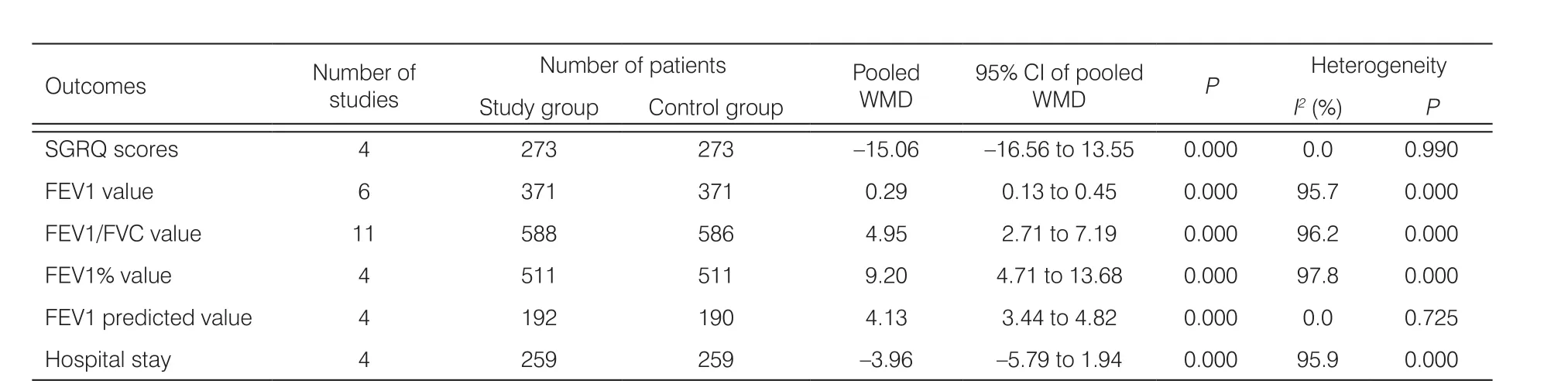
Table 2. Results of meta-analysis of outcomes
3.2.3 Hospital stay
Four studies19-22recorded hospital stay. There was significant heterogeneity (I2= 95.9%, P=0.000), and a random-effect model was used. There was a shorter hospital stay in the TCM combined with conventional nursing group (WMD = –3.96, 95% CI: –5.79 to –1.94,P=0.000) (Table 2).
3.2.4 Clinical efficacy
Clinical efficacy was reported by ten studies.10,13,18,20,22-27The analysis of clinical efficacy did not exhibit heterogeneity (I2= 0.0%, P=0.606). The difference in clinical efficacy was statistically significant between the groups,and there was a preferable clinical efficacy in the TCM combined with conventional nursing group (OR = 4.41,95% CI: 2.85–6.82, P=0.000) (Figure 2). Subgroup analysis was conducted to compare the clinical efficacy of TCM nursing combined with conventional nursing between patients with acute exacerbation of COPD(AECOPD) and patients with stable COPD. There was no significant heterogeneity (I2= 0.0%, P=0.448), and a fixed-effect model was used. For patients with AECOPD,TCM nursing combined with conventional nursing had greater clinical efficacy (OR = 10.42, 95% CI: 4.11–26.42, P=0.000), relative to patients with stable COPD(OR = 2.89, 95% CI: 1.43–5.86, P=0.003) (Figure 3).
3.2.5 Publication bias
Evaluation of publication bias was performed using Begg’s test and, based on clinical efficacy, showed no significance (P=0.325). Figure 4 shows that there is no publication bias and depicts the distribution of ORs comparing the clinical efficacy for the ten studies included in this meta-analysis.
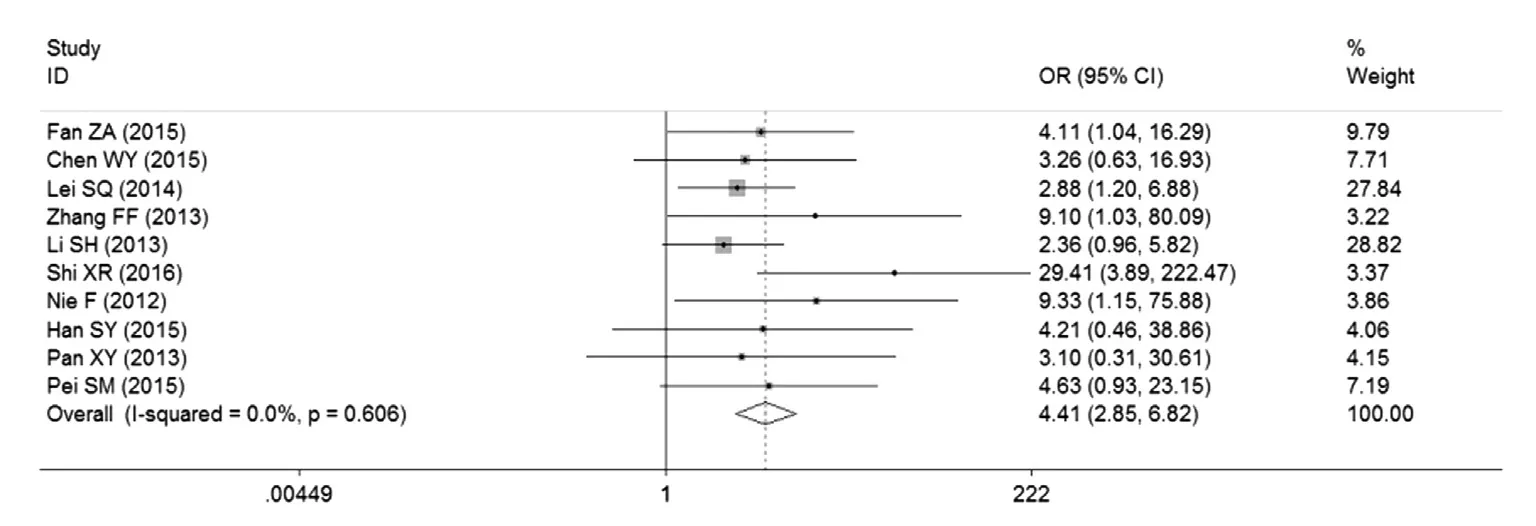
Figure 2. Forest plots of analysis of study group versus control group for clinical efficacy. The results are presented as individual and pooled ORs and 95% CIs. CI = confidence interval; OR = odds ratio.
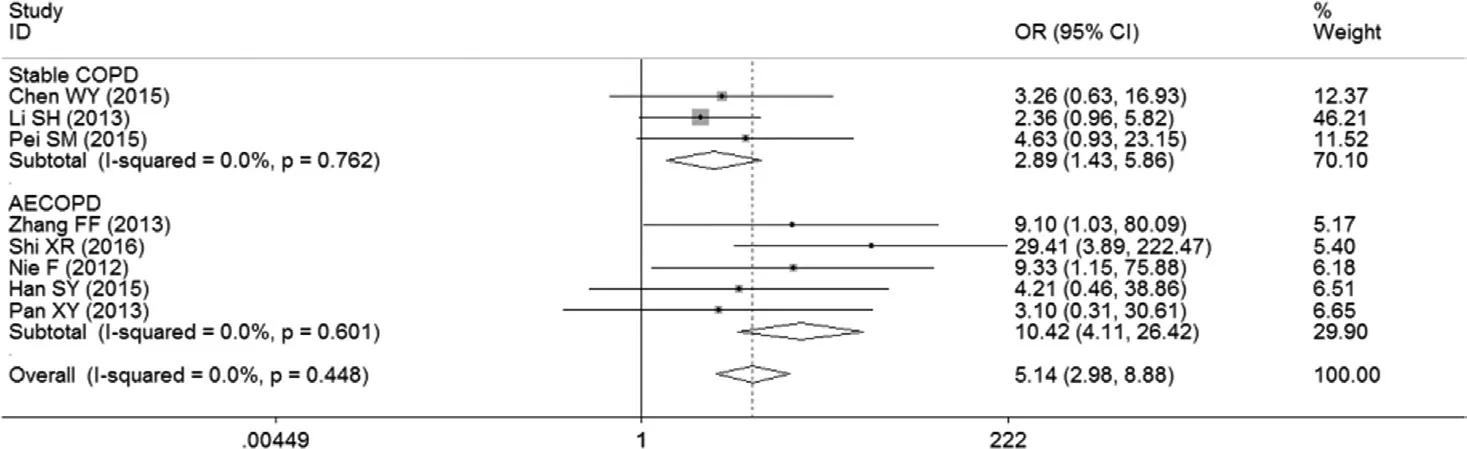
Figure 3. Forest plots of subgroup analysis of stable COPD versus AECOPD for clinical efficacy. The results are presented as individual and pooled ORs and 95% CIs. AECOPD = acute exacerbation of COPD; CI = confidence interval; COPD = chronic obstructive pulmonary disease; OR = odds ratio.
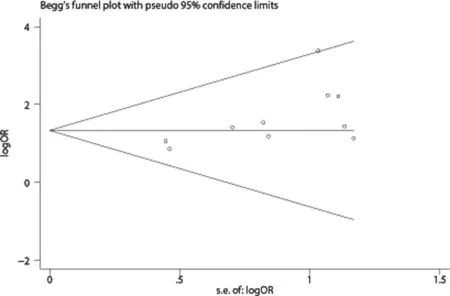
Figure 4. Funnel plots of the evaluation of potential publication bias in the efficacy of TCM nursing combined with conventional nursing in patients with COPD. COPD = chronic obstructive pulmonary disease; s.e. = standard error; TCM = traditional Chinese medicine.
4. Discussion
To our knowledge, this comprehensive and detailed meta-analysis is the first to evaluate the association between TCM nursing combined with conventional nursing and conventional nursing alone in treating COPD.This meta-analysis presents us with the evidence that TCM nursing combined with conventional nursing can provide patients with COPD a higher life quality, better lung function, preferable clinical efficacy, and a shorter hospital stay. Furthermore, subgroup analysis indicates that TCM nursing combined with conventional nursing has greater clinical efficacy in patients with AECOPD and stable COPD.
According to the TCM syndrome differentiation standard,28COPD can be divided into several types, such as exterior cold and interior heat, obstructed lung-Qi by retention of phlegm, stagnated lung-Qi, stagnation of phlegm-heat in the lung, and so on. TCM nursing is based on the theoretical system of TCM, which mainly embodies the concept of wholism and treatment determination based on syndrome differentiation. Tuinaology of TCM is a form of Chinese manipulative therapy that prevents and treats diseases. Currently, it is best known as “Tuina” and “Anmo”. The active principles of Tuina therapy can be considered to keep the balance of Yin and Yang, dredge the meridians and collaterals, regulate the Qi and blood, regulate the Zang-Fu organ function, restore and treat injured soft tissue to reduce the displacement, and lubricate joints. For regulation on the material level, Tuina can regulate the respiration system. When conducting Tuinaology, Feishu, Fenglong, Neiguan, Pishu, Qihai, Zhongji, and Tiantu can be selected to treat patients with COPD.Each procedure is performed for 3 minutes, once a day, until a local acid bilge feeling is reported. Studies29suggest that Tuina can improve lung function and the quality of life of patients with COPD; this finding is consistent with the results of this meta-analysis. Apart from Tuinaology, acupuncture treatment is also important for COPD patients’ rehabilitation.30The COPD rehabilitation guideline recommends that effective exercise can be ensured with moderate intensity.31Traditional rehabilitation exercises such as six words, eight brocade, and Tai chi are relevant to improvements in exercise capacity, respiratory function, and respiratory muscle strength. Additionally, because COPD is a prolonged disease, patients with COPD are prone to be depressed and anxious. TCM emotional care is necessary.
Because of the significant heterogeneity of the eligible studies, random-effects models were used during pooling of data. Significant heterogeneity persisted during the sensitivity analysis, especially when comparing the FEV1 value, FEV1/FVC value, and FEV1% value between the two groups. The significant heterogeneity was likely a result of the differences in some potentially confounding variables that were not specifically considered, such as disease type, demographic characteristics, or methodology differences among studies.6-10,12-17In addition, the studies did not use the same TCM nursing methods, and the severity of illness was also different, leading to potential heterogeneity. COPD severity might affect the rehabilitation of lung function, so there was a significant heterogeneity, especially in comparing the FEV1 value, FEV1/FVC value, and FEV1% value.Thus, more rigorous RCTs should be conducted to evaluate the parameters that have significant heterogeneity in this meta-analysis.
This meta-analysis suggests that for the treatment and rehabilitation of COPD, TCM nursing combined with conventional nursing can be performed preferably. We attempted to search the literature as thoroughly as possible to minimize publication bias. Begg’s test and Egger’s linear regression test, as well as the funnel plots,showed that there was no publication bias, indicating that this meta-analysis approximated the actual results.However, there are some limitations as follows. First,the study of the application of Chinese and Western medicine nursing care in patients with COPD is limited to Chinese language texts; relevant English literature was not retrieved. Second, because some evaluation indicators that were included in the studies are not uniform, data extraction was limited and further subgroup analysis could not be performed. Third, the sample size of the studies was relatively small; a large-scale multicenter RCT comparing TCM nursing integrated with conventional nursing with conventional nursing alone in patients with COPD is warranted.
5. Conclusions
TCM nursing combined with conventional nursing can achieve maximum optimization by integrating the advantages of TCM nursing with conventional nursing.This meta-analysis shows that for patients with COPD,TCM nursing combined with conventional nursing emphasized that dialectical nursing can be preferably performed. However, because there is significantly high heterogeneity among studies, further studies should be undertaken to confirm this evidence.
Acknowledgments
We thank Tianjin University of Traditional Chinese Medicine for offering us their library for this study.
Conflicts of interest
All contributing authors declare no conflicts of interest.
References
1. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med.2013;187:347-365.
2. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
3. Barnes PJ. Against the Dutch hypothesis: asthma and chronic obstructive pulmonary disease are distinct diseases. Am J Respir Crit Care Med.2006;174:240-243.
4. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12.
5. Dai JJ. Integrated traditional Chinese and western nursing management of chronic obstructive pulmonary disease in 20 patients. Nurs Integr Trad Chin Western Med. 2016;2:66-67. 70 (in Chinese).
6. Li MX. To investigate the effects of TCM nursing intervention on respiratory muscle strength, lung function and quality of life in patients with stable COPD. World Latest Med Inf (Electronic Version).2015;15:120. (in Chinese).
7. He XM. Study on application of TCM nursing in pulmonary function and quality of life of patients with COPD stable phase. J Sichuan Trad Chin Med.2014;32:169-171. (in Chinese).
8. Zheng XH, Liu J, Luo Y, Jing XR, Qiu F. The application of holistic nursing with traditional Chinese medicine in patients with stable chronic obstructive pulmonary disease. Contemp Med Forum.2014;12:20-22. (in Chinese).
9. Peng J. Effects of syndrome differentiation on quality of life and pulmonary function in patients with chronic obstructive pulmonary disease. Guid J Trad Chin Med Pharm. 2009;15:71-72. (in Chinese).
10. Chen WY, Wan JF, Liu LL. Combining traditional Chinese and western medicine nursing on stability of chronic obstructive pulmonary disease. Liaon J Trad Chin Med. 2015;42:619-621. (in Chinese).
11. Li J. Study on TCM nursing on the improvement of pulmonary function of patients with COPD in stable stage. Chin Med Mod Distance Educ China.2015;13:120-121. (in Chinese).
12. Zuo AW, Xiong GZ. Effects comparison of integrated traditional Chinese medicine nursing and routine nursing application to chronic obstructive pulmonary disease. Chin Med Mod Distance Educ China. 2015;13:121-122. (in Chinese).
13. Pei SM, Zheng XY, Bo SP, Yao JJ. Effect of integrated traditional and western medicine nursing intervention on stable chronic obstructive pulmonary disease. Med Inf. 2015;28:118-119. (in Chinese).
14. Shi PF, Long B, Pan MZ, Li ZQ, Zhou Y, Peng YF.Clinical application and study of traditional Chinese medicine nursing care in patients with asthma(acute attack of chronic obstructive pulmonary disease). National Training Course on Hypertension Prevention and Knowledge Promotion and Healthy Blood Pressure. Chin J Integr Trad Chin Western Med. 2014. (in Chinese).
15. Liu QH. Impact analysis of exerting traditional Chinese medicine nursing to the quality of life among patients with COPD. J Sichuan Trad Chin Med.2014;32:161-163. (in Chinese).
16. Wang HY, Wang L. Application of Chinese medicine nursing program in elderly patients with chronic obstructive pulmonary disease. Clin J Chin Med.2015;7:24-25. (in Chinese).
17. Huang XT. Effects of TCM nursing on pulmonary function and quality of life in stable stage COPD patients. J Baotou Med College. 2016;32:119-120.(in Chinese).
18. Li SH, Li JQ, Li WQ, et al. Clinical observation of combine traditional Chinese and western medicine nursing in stable stage chronic obstructive pulmonary.Shanxi J Trad Chin Med. 2013;29:55-57. (in Chinese).
19. Fu XF, Li L, Cao X. Clinical nursing pathway of Chinese and western medicine in nursing of patients with AECOPD. J Emerg Trad Chin Med.2014;23:1769-1772. (in Chinese).
20. Lei SQ. Effects of holistic nursing intervention on chronic obstructive pulmonary disease. Chin Med Mod Distance Educ China. 2014;12:122-123. (in Chinese).
21. Liang GX, Zeng L. Nursing based on the differences of symptoms in acute exacerbation of chronic obstructive pulmonary disease. Mod Hosp.2010;10:96-98. (in Chinese).
22. Pan XY. Clinical nursing pathway in the treatment of patients with acute chronic obstructive pulmonary disease. Today Nurse. 2015;2:30-32. (in Chinese).
23. Fan ZA. To study the comprehensive nursing intervention of patients with chronic obstructive pulmonary disease. Nei Mongol J Trad Chin Med.2015;34:166. (in Chinese).
24. Zhang FF, Lin S. Effect of integrated traditional Chinese and western medicine on acute exacerbation of chronic obstructive pulmonary disease. Health Required. 2013;12:409. (in Chinese).
25. Nie F, Duan YY. Nursing of patients with acute exacerbation of chronic obstructive pulmonary disease with integrated traditional Chinese and western medicine. J Emerg Trad Chin Med. 2012;21:853-854. (in Chinese).
26. Han SY. Effect of integrated traditional Chinese and western medicine on acute exacerbation of chronic obstructive pulmonary disease. Cardio Dis J Integr Trad Chin Western Med (Electronic). 2015;3:175-176. (in Chinese).
27. Shi XR. The application effect of integrated western and Chinese nursing in acute episode chronic occlusive pulmonary disease. Today Nurse. 2016;8:21-22. (in Chinese).
28. Tian DL, Cai G. Chinese Internal Medicine. Shanghai: Shanghai Scientific & Technical Publishers;2013. (in Chinese).
29. Zhang W. Effect of massage on chronic obstructive pulmonary disease. Guide China Med. 2015;13:195.(in Chinese).
30. Suzuki M, Namura K, Ohno Y, et al. The effect of acupuncture in the treatment of chronic obstructive pulmonary disease. J Altern Complement Med.2008;14:1097-1105.
31. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13-e64.
- Frontiers of Nursing的其它文章
- Role of academic self-efficacy in the relationship between self-directed learning readiness and problem-solving ability among nursing students
- Effect of a new health education model on continuous nursing in elderly patients with diabetes mellitus
- Women’s experiences of formula feeding their infants: an interpretative phenomenological study
- Job burnout and turnover intention among nurses in China: the mediating effects of positive emotion†
- An empirical study on evaluation indexes of scientific research achievements in nursing†
- A literature review of research exploring the experiences of overseas nurses in the United Kingdom (2002–2017)