A Lazarus effect: A case report of Bupropion overdose mimicking brain death
Douglas Stranges, Alan Lucerna, James Espinosa, Neveen Malik, Marc Mongeau, Kelly Schiers, Syed Omar Shah, Joan Wiley, Philip Willsie
1 Department of Emergency Medicine, Department of Internal Medicine, Rowan University SOM, Kennedy University Hospital, Washington Twp, NJ, USA
2 Department of Emergency Medicine, Rowan University SOM, Kennedy University Hospital, Stratford, NJ, USA
3 Department of Pulmonary/Critical Care/Sleep Medicine, Kennedy Health Alliance, Kennedy University Hospital, Washington Twp, NJ, USA
4 Department of Pulmonary and Critical Care Medicine, Rowan University SOM, Kennedy University Hospital, Washington Twp, NJ, USA
5 Department of Neurocritical Care, Thomas Jefferson University Hospital, Philadelphia, PA, USA
Dear editor,
We report a case of a 47-year-old female who presented with a toxic bupropion ingestion leading to cardiac arrest.She initially exhibited a loss of brainstem reflexes in conjunction with burst-suppression pattern on EEG. Burst suppression is an EEG waveform pattern of alternating isoelectric suppressions and high voltage bursts.[1]Our patient ultimately made a full neurologic recovery a few days later. While there are two other cases in the literature of bupropion overdose resulting in EEG burst-suppression and loss of brainstem reflexes, we believe this is the only reported adult case complicated by cardiac arrest.[2,3]
CASE
A 47-year-old female, with a history of depression,anxiety and previous suicide attempts, presented to the emergency department (ED) one hour after intentional ingestion of an unknown quantity of extended-release 150 mg bupropion tablets. On arrival she was lethargic but arousable and able to answer questions. She denied any focal complaints. Initial laboratory data was unremarkable.EKG revealed sinus tachycardia at 108 beats/minute with a QTc interval of 485 ms and a QRS interval of 80 ms (ECG,Figure 1). Toxicology screen for alcohol, salicylate, and acetaminophen were all below detectable levels. Urine drug screen was positive for benzodiazepines only, but the patient was known to be taking alprazolam.
While in the ED, she had two witnessed generalized tonic-clonic seizures, separated by 40 minutes. She was admitted to the intensive care unit (ICU) where she was evaluated by the critical care team, a toxicologist, and a neurologist. Immediately upon arrival to the ICU,the patient had recurrent seizures consistent with status epilepticus, and required intubation for airway protection using 150 mcg of fentanyl and 30 mg of etomidate. She was treated with lorazepam and loaded with levetiracetam.Shortly thereafter, she became hypotensive, required vasopressor therapy with norepinephrine, and was given sodium bicarbonate therapy (for her now-widened QRS interval of 164 ms) (ECG, Figure 2). Despite aggressive attempts to stabilize her, she suffered a cardiac arrest with pulseless electrical activity (PEA), necessitating cardiopulmonary resuscitation, administration of intravenous epinephrine, and lipid emulsion therapy.
A computerized tomography (CT) scan of the brain was performed and demonstrated normal grey-white differentiation and no cerebral edema. Despite a very brief and witnessed arrest, her neurological exam was concerning for neurologic injury. She lacked all brain stem reflexes; her pupils were 8 mm and non-reactive.She was placed on continuous EEG monitoring, which revealed burst-suppression pattern (Figure 3). Targeted temperature management was initiated to 36 degrees Celsius.
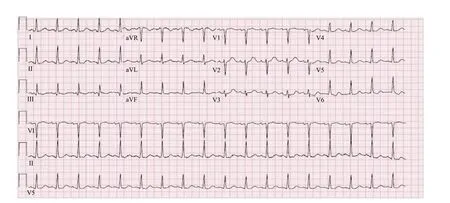
Figure 1. ECG on arrival to the ED.
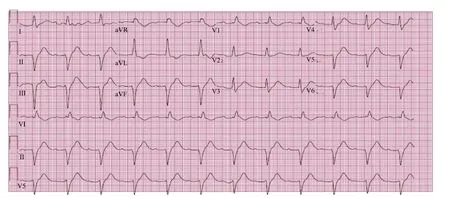
Figure 2. ECG displaying prolonged QRS interval just prior to cardiac arrest.
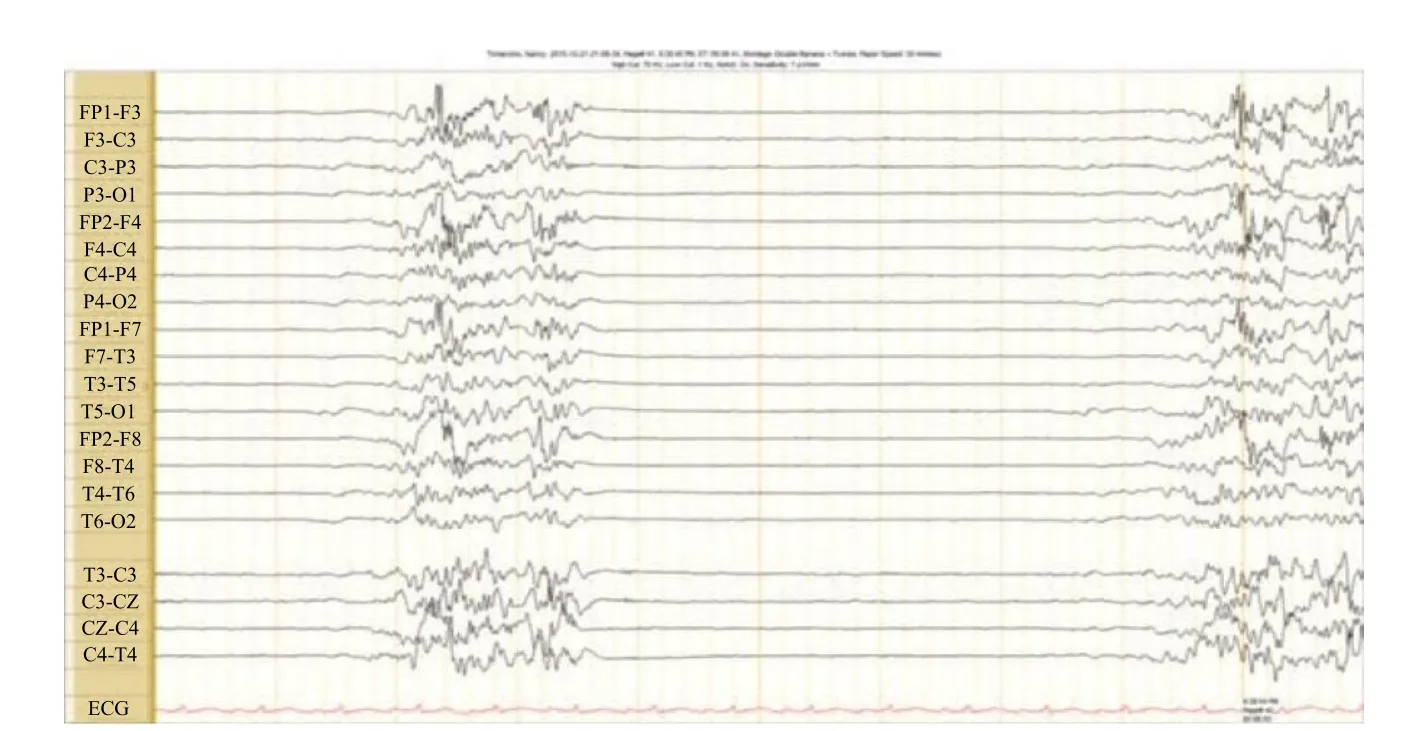
Figure 3. EEG recording showing burst-suppression. This tracing was taken within 24 hours of the patient’s initial presentation, following her cardiac arrest.
On hospital day 3, she began initiating respirations on the ventilator and had faint corneal reflexes. By hospital day 4, she was moving all extremities to command. She required tracheostomy placement for failure to wean,but was eventually discharged with complete neurologic recovery. She has since returned to the hospital for minor respiratory complaints but has maintained completely normal neurologic status and full cognitive function.
DISCUSSION
Bupropion is a dopamine reuptake inhibitor, used for depression, smoking cessation, attention deficit/hyperactivity disorder, and neuropathic pain.[4–6]It has an incompletely understood mechanism of action that includes selective inhibition of the neuronal reuptake of dopamine.[7]Bupropion has a well-documented list of adverse effects including sinus tachycardia, ECG changes including QRS prolongation, and other arrhythmias.[8]It has a particularly high incidence of seizures; exceeding that of other commercially available antidepressants by up to 4-fold.[9]
In a toxic ingestion, the effects of bupropion are known to include the most dramatic forms of these above side effects: status epilepticus, and wide-complex tachycardia leading to cardiac arrest.8 More commonly,the clinical syndrome is equivocal; featuring tachycardia,agitation, and hallucinations.[10]It is normally managed supportively; and with antiepileptic therapy if seizure activity is present.[11]In the case described above, we observed a deep coma in which a patient exhibited a loss of brainstem reflexes in association with burstsuppression pattern on EEG. Although she suffered a short cardiac arrest, her poor exam preceded it and was related to the overdose rather than the arrest.
Electroencephalography can play an important role in the management of some overdoses, as in the case presented. It is a common diagnostic modality when an overdose presentation includes a seizure, but also has practical utilization in brain death, coma, and focal brain disorders.[12]Within the examination of EEG recordings,there are characteristic patterns. One of these patterns is the aforementioned burst-suppression. These alternating periods of isolectricity and high voltage have been studied in numerous scenarios. Burst suppression waveforms have been associated with the inactivated brain, lesions underlying the cortex, large dosages of anesthetics/sedatives, cerebral anoxia, hypothermia, and coma.[13]They are considered by the neurology community to be a poor prognostic marker for neurologic recovery in the context of overdose, post-cardiac arrest and coma.[1,12,14]
Despite the EEG and clinical findings, our patient had a full neurologic recovery once the medication was metabolized and excreted. This emphasizes the importance of a thorough evaluation and utilization of all diagnostic modalities prior to prognostication. While the clinical scenario may show a grim prognosis and while preliminary diagnostic and monitoring tools may suggest brain death, conclusion of brain death should be deferred until enough time has elapsed for the medication to be fully systemically eliminated. In our case, the full neurologic recovery seen would not have been realized if brain death had been prematurely declared.
CONCLUSION
Extreme care should be taken in scenarios of bupropion overdose. We suggest that early prognostication should be avoided in such cases, patients should be continuously monitored and enough time must be allowed for drug clearance prior to any neurological forecasting.
Funding:None.
Ethical approval:The study was approved by the Institutional Review Board.
Conflicts of interest:The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors:DS proposed the study and wrote thefirst draft. All authors read and approved the final version of the paper.
1 Lewis LD, Ching S, Weiner VS, Peterfreund RA, Eskander EN,Cash SS, et al. Local cortical dynamics of burst suppression in the anaesthetized brain. Brain. 2013; 136(9): 2727-37.
2 Mundi JP, Betancourt J, Ezziddin O, Tremayne B, Majic T,Mosenifar Z. Dilated and unreactive pupils and burst-suppression on electroencephalography due to bupropion overdose. J Intensive Care Med. 2012; 27(6): 384-8.
3 Farias-Moeller R, Carpenter JL. Coma with absent brainstem reflexes and burst suppression after bupropion overdose in a child. Neurocrit Care. 2017;26(1):119-21.
4 Wilens TE, Haight BR, Horrigan JP, Hudziak JJ, Rosenthal NE,Connor DF, et al. Bupropion XL in adults with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled study.Biol Psychiatry. 2005;57(7):793-801.
5 Semenchuk MR, Sherman S, Davis B. Double-blind, randomized trial of bupropion SR for the treatment of neuropathic pain.Neurology. 2001;57(9):1583-8.
6 American Psychiatric Association. Practice guidelines for the treatment of patients with major depressive disorder. Am J Psychiatry. 2000; 157(4):1-45.
7 Bryant SG, Guernsey BG, Ingrim NB. Review of bupropion.Clin Pharm. 1983;2(6):525-37.
8 GlaxoSmithKline: Wellbutrin SR (bupropion) package insert Website. https://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Wellbutrin_Tablets/pdf/WELLBUTRIN-TABLETS-PI-MG.PDF. Published April 2016. Accessed November 1, 2016.
9 Skowron DM, Stimmel GL. Antidepressants and the risk of seizures. Pharmacotherapy. 1992;12(1):18-22.
10 Shepherd G, Velez L, Keyes D. Intentional bupropion overdoses.J Emerg Med. 2004;27(2):147-151.
11 Storrow A. Bupropion overdose and seizure. Am J Emerg Med.1994;12(2):183-184.
12 Niedermeyer E, da Silva FL. Electroencephalography: Basic Principles, Clinical Applications, and Related Fields. Fifth Edition. Philadelphia: Lippincott, Williams & Wilkins; 2005.
13 Niedermeyer E. The burst-suppression electroencephalogram.Am J Electroneurodiagnostic Technol. 2009;49(4):333-41.
14 Reeves AL, West morel and BF, Klass DW. Clinical accompaniments of the burst-suppression EEG pattern. J Clin Neurophysiol. 1997;14(2):150-3.
 World journal of emergency medicine2018年1期
World journal of emergency medicine2018年1期
- World journal of emergency medicine的其它文章
- Understanding the effect of propofol and electrical cardioversion on the systolic blood pressure of emergency department patients with atrial fibrillation
- Perimortem caesarean section: A case report of an out-of-hospital arrest pregnant woman
- Drug calculation ability of qualified paramedics:A pilot study
- Ischemic stroke due to carbon monoxide intoxication:Two case reports
- First-in-man implantation of the retrievable and repositionable VenusA-Plus valve
- Dose-related effects of dexmedetomidine on immunomodulation and mortality to septic shock in rats
