Can patients with non-convulsive seizure be identif i ed in the emergency department?
Gholamreza Sadeghipoor Roodsari, Geetha Chari, Bryan Mera, Shahriar Zehtabchi Department of Emergency Medicine, State University of New York, Downstate Medical Center, Brooklyn, NY, USA Department of Neurology, State University of New York, Downstate Medical Center, Brooklyn, NY, USA
Can patients with non-convulsive seizure be identif i ed in the emergency department?
Gholamreza Sadeghipoor Roodsari1, Geetha Chari2, Bryan Mera1, Shahriar Zehtabchi11Department of Emergency Medicine, State University of New York, Downstate Medical Center, Brooklyn, NY, USA2Department of Neurology, State University of New York, Downstate Medical Center, Brooklyn, NY, USA
BACKGROUND: Non-convulsive seizure (NCS) is an underdiagnosed, potentially treatable emergency with significant mortality and morbidity. The objective of this study is to examine the characteristics of patients with NCS presenting with altered mental status (AMS) and diagnosed with electroencephalography (EEG), to identify the factors that could increase the pre-test probability of NCS.
METHODS: Retrospective study using the data collected prospectively. Inclusion criteria:patients older than 13 years with AMS. Exclusion criteria: (1) immediately correctable AMS (e.g.,hypoglycemia, opiod overdose); (2) inability to undergo EEG; (3) hemodynamic instability. Outcomes compared between NCS and non-NCS cases: vital signs, lactate level, gender, witnessed seizure,use of anticonvulsive in the field or in the ED, history of seizure or stroke, head injury, abnormal neurological finding and new abnormal findings on head CT. Data presented as medians and quartiles for categorical and percentages with 95%CI for continuous variables. Univariate analyses were performed with Man-Whitney U and Fisher's Exact tests. A multivariate analysis model was used to test the predictive value of clinical variables in identifying NCS.
RESULTS: From 332 patients (median age 66 years, quartiles 50–78), 16 were diagnosed with NCS (5%, 95%CI 3%–8%). Only age was significantly different between the NCS vs. non-NCS groups in both univariate (P=0.032) and multivariate analyses (P=0.016).
CONCLUSION: Other than age, no other clinically useful variable could identify patients at high risk of NCS. ED physicians should have a high suspicion for NCS and should order EEG for these patients more liberally.
Altered mental status; Seizure; Non-convulsive; Electroencephalography
INTRODUCTION
Non-convulsive seizure (NCS) is def i ned as cerebral ictal activity with no obvious clinical sign of motor activity.[1–4]It is the underlying cause in about 5% of patients presenting to the emergency department (ED)with altered mental status (AMS). Almost half of these NCS cases are in form of non-convulsive status epilepticus (NCSE).[5]The change in mental status could be in form of confusion, lethargy, delirium, agitation,coma or even depression or inappropriate behavior.[4–10]AMS is the main clinical presentation of NCS and one of the criteria for its diagnosis.[2,4]
Electroencephalography (EEG) remains the gold standard for diagnosis of NCS. However, EEG is not available in most EDs on a regular basis.[7,11,12]Therefore,the diagnosis of this time-sensitive neurological emergency remains a challenge for emergency physicians. In fact, the studies have shown that the diagnosis of NCS is missed or delayed in approximately 50% of the cases.[4,8,11,12]In case of NCSE, this delay can lead to serious consequences including neuronal damage and cardiac arrhythmias.[2,13,14]Early treatment can be effective in preventing morbidity and mortality and therefore it is recommended to start treatment as soon as 5 minutes for generalized and 10 minutes of focal status epilepticus. However, delayed treatment is associated with decrease responsiveness to treatment and risk of subsequent neurological sequelae.[1,3,11,12,15–17]
Early diagnosis and treatment of NCS/NCSE is particularly more important in elderly population in which the mortality rate in NCES has been reported to be as high as 30%.[18]Previous studies on patients at high risk of NCS were mostly conducted on patients in the intensive care units.[2,3,11,14,16]To our knowledge,no study has examined the clinical characteristics of patients diagnosed with NCS in the ED. The objective of this study is to examine the characteristics of AMS patients who are diagnosed with NCS in the ED in order to identify the factors that could increase the pre-test probability of NCS in patients presenting with AMS.
METHODS
Study design
We performed a retrospective analysis on the data collected prospectively in our previous trials.[5,6,19]The study was approved by the joint institutional review board, which waived the requirement for informed consent. However, written consent was obtained from the patient after resolution of altered mental status or their legally authorized representative.
Population and setting
We enrolled a convenience sample of ED patients older than 13 years of age with AMS at two urban academic centers (Kings County Hospital Center and Downstate Medical Center) with annual ED censuses of 120 000 and 75 000, respectively. AMS was defined as alteration in level or content of mental status, including change in arousability, lethargy, delirium, confusion,agitation, coma, or unexpected change in behavior.
Exclusion criteria were: (1) immediately correctable cause of AMS including hypoglycemia (blood sugar less than 60 mg/dL), hypothermia (temperature below 35.0 °C), heat stroke and opioid overdose responding to naloxone; (2) inability to undergo EEG recordings(e.g., severe scalp injury, combative patients); (3)hemodynamic instability (SBP below 90 mmHg).
Patients with witnessed seizures in the ED were only included if they experienced a prolonged post-ictal period.
Outcomes
The main outcome of this study was variables that could predict NCS (including NCSE). Outcome was assessed by comparing the characteristics of NCS and non-NCS cases and by performing univariate analysis on already collected data. NCS was determined by presence of ictal activity on the EEG interpreted by the on-call epileptologist (reference standard). We defined NCS as rhythmic generalized or focal EEG pattern in an altered patient with no motor activity and NCES as continuous EEG activity lasting longer than 10 minutes or two or more activities without return to normal EEG in between.[1,5]
Independent variables: information pertaining to medical history, physical examination, present illness, and imaging were analyzed. The variables of interest included: vital signs at presentation [systolic and diastolic blood pressure in mmHg, heart rate, temperature and oxygen saturation (pulse asymmetry), finger stick glucose (mg/dL), lactate level(mmol/L), gender, witnessed seizure in the field (reported by EMS or family)] or in the ED, use of anticonvulsive in the field or in the ED, history of seizure, history of stroke, head injury, abnormal neurological finding in the exam (other than AMS), and any new abnormal findings in the head CT.
Study protocol
The data used for this study were already collected and entered into an electronic database by trained research coordinators. For the purpose of this study, 10%of the cases were cross-checked by the main author to ensure accuracy of the collected data.
The enrollment process in the original trial was as follows: upon presentation of a patient with AMS, ED attending notified the research team 24 hours a day, 7 days a week using a research hotline. A 30-minute EEG(21 EEG channels and one EKG channel) was obtained for each patient; either by using a commercially available EEG device (Nicolet Monitor, Viasys, San Carlos, CA,USA) with standard 9-mm gold-plated cup electrodes placed according to the international 10–20 system, or a new FDA-approved EEG device, called microEEG (Biosignal Group Inc., Brooklyn, NY, USA). The details of randomization process and EEG recordings have been described previously.[5,6,19]
The EEG recordings were then wirelessly transferred to an on-call epileptologist using a secure hospital server for interpretation. The EEG results were conveyed to the ED physician caring for the patient within 30 minutes of completion of recording.
Statistical analysis
Continuous variables are reported as medians and quartiles. Categorical variables are reported as percentages with 95% confidence intervals. For this analysis we created two categories of NCS/NCSE and non-NCS/NCSE (including normal EEG as well as other findings such as slowing, triphasic waves, burst suppression, etc).We compared the variables between these two groups using Mann-Whitney U and Fisher's exact tests, when appropriate (alpha 0.05, two-tailed). We also generated a multivariate analysis model to test the value of the clinical variables in predicting NCS. Variables included in the model were: age, gender, systolic blood pressure, diastolic blood pressure, heart rate, pulse-oxymetry, temperature,fingerstick glucose, serum lactate level, history of epilepsy,history of stroke, seizure activity in the field and in the ED, anticonvulsant administration in the field or in the ED, head injury, abnormal neurological examination, and new abnormal findings on head CT.
RESULTS
During enrollment periods for the two prospective trials (2011–2012), a total of 408 patients were enrolled.Seventy six patients who were assigned to the control group in the second trial and did not undergo EEG were excluded. Data analysis was performed on 332 cases (median age of 66 years, quartiles: 50–78; 50%male). EEGs were recorded with both standard EEG and microEEG in 259 cases (standard EEG used as reference standard) and MicroEEG alone for 73 cases. In total, 16 patients were diagnosed with NCS (5%, 95%CI 3%–8%;4 cases diagnosed with MicroEEG and 12 with standard EEG). Out of these 16 NCS cases, 8 (50%) were in form of NCSE.
Comparison between NCS/NCSE and non-NCS/NCSE cases are summarized in Tables 1 and 2. As noted in the Method section, patients with seizure in the EDwere only enrolled if they suffered from prolonged postictal period. Patients who had seizure in the ED but regained their mental status within a reasonable time,were not enrolled.
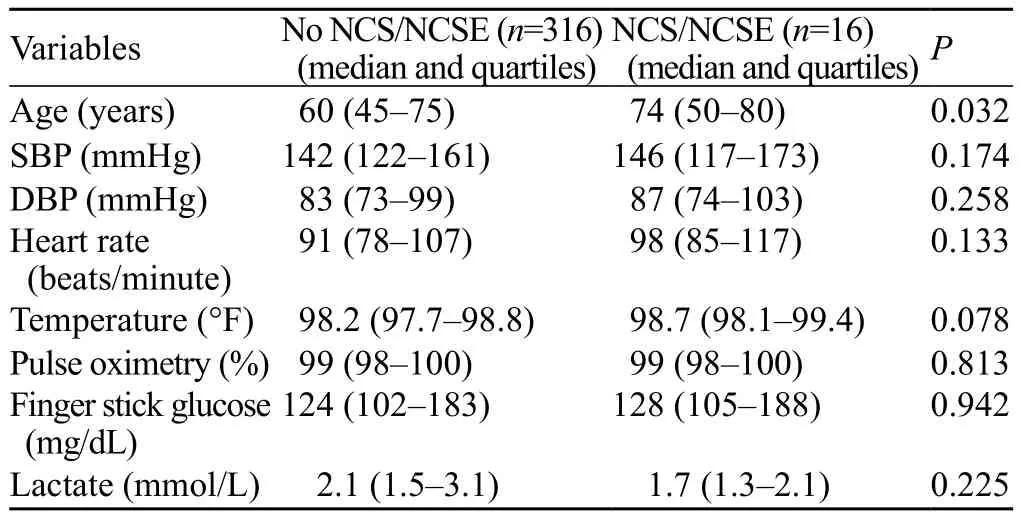
Table 1. Comparison of continuous variables between the patients with and without non-convulsive seizure (including non-convulsive status epilepticus)
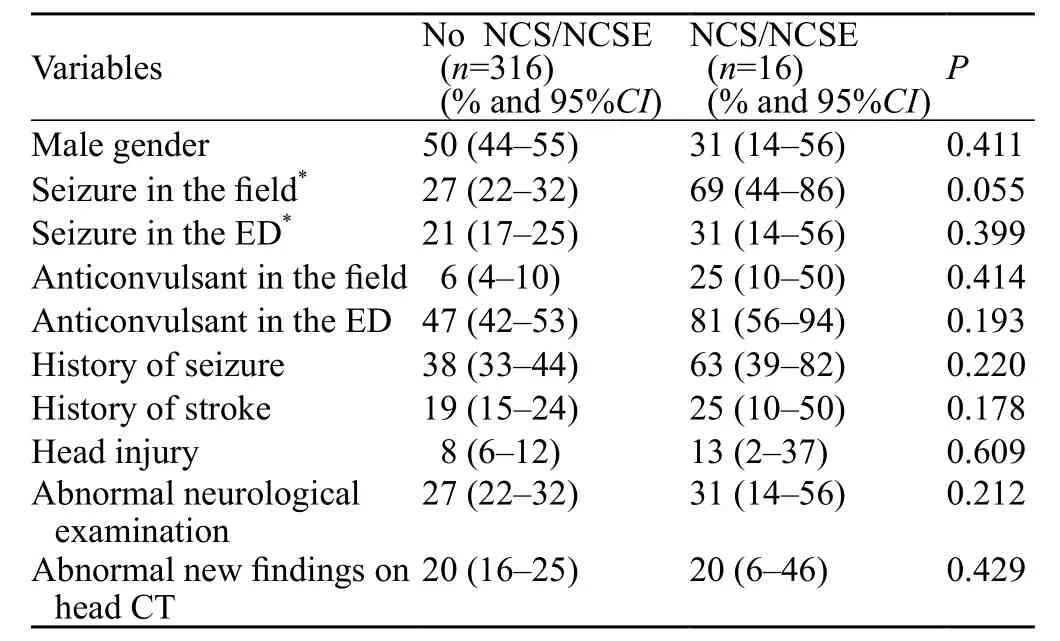
Table 2. Comparison of dichotomous variables between the patients with and without non-convulsive seizure including non-convulsive status epilepticus
As shown in the Table 1, only age was significantly different between the NCS/NCSE vs. non-NCS/NCSE groups (P=0.032). Increase in age is associated with higher risk of NCS/NCSE in AMS patients. Similarly, in multivariable analysis, only age predicted NCS: P=0.016,odds ratio 1.05, 95%CI 1.01–1.10).
DISCUSSION
Our fi ndings show that increase in age is associated with higher risk of NCS (including NCSE) in AMS patients. This finding is in consistent with other studies reporting higher probability of NCS with increase age.[11,20]Aside from age,there is no other clinically useful variable that could affect pre-test probability of NCS/NCSE in patients with AMS.It is well documented that certain number of convulsive seizures convert to non-convulsive seizure during their clinical course. Therefore, it is reasonable to conclude that patients who have seizure in the field or in the ED are at higher risk of NCS or even NCSE. However in our analysis, reported seizure in the field or in the ED could not predict NCS. It is likely that a larger study with larger number of patients with NCS/NCSE will be able to prove this correlation.
Other studies on patients with AMS with similar objective have reported various results. A retrospective study of 21 cases of NCSE, out of a total of 215 EEGs,found three independent clinical risk factors for NCSE:seizure (s) in the acute setting, ocular movements(nystagmus and/or gaze deviation) and ongoing CNS infection.[21]Another study reported history of epilepsy as the only predictive criteria for NCSE in history and exam.[9]However, a prospective study on 44 patients with 7 NCSE cases found no significant differences between NCSE patients and others for age, medications,vital signs or clinical presentations. They reported a significant difference only for gender.[22]
Another study comparing 12 NCS with 36 non-NCS patients found a significant difference between the two groups in remote (not recent) history of seizure and ocular movement abnormalities (nystagmus and sustained eye deviation). There was no difference between the two groups in term of history of epilepsy or even subtle motor activities. In this study, no factor was found to be sensitive or specif i c enough for predicting NCS.[23]
In a recent study reviewing the presentation of 68 cases of NCS (confirmed by EEG) from 12 previously published papers, authors concluded that female sex, a history of epilepsy or tonic clonic seizure, and recent discontinuation of benzodiazepines are risk factors for
NCS.[8–11,17,20–22]
Similar to our study, the number of patients identif i ed with NCS/NCSE in these trials was small. However,our study has two advantages over most of the previous reports. First, our trials[5,6]were conducted prospectively and involved patients with undifferentiated AMS. Second,the trials were conducted in the emergency department.Therefore, the findings could be more applicable to ED patients. NCS can lead to NCSE, a potentially treatable, time sensitive neurological emergency with significant increase in morbidity and mortality if not diagnosed or treated immediately.[2,4,8,11–14,17,24]This puts the ED physicians in the frontline, facing the challenge of identifying patients at high risk of this entity as soon as possible. Therefore, developing criteria to help ED physicians increase or decrease their pre-test probability for the disease to an actionable level, could have significant impact on management of patients at risk.Currently, EEG remains the main tool for diagnosing of NCS/NCSE.[4,11,22,24–26]Our retrospective analysis confirms that ED physicians should have a high index of suspicion for NCS/NCSE in ED patients with AMS and should have a low threshold for ordering EEG. The importance of availability of EEG in evaluation of AMS has been suggested by several other studies.[6–8,26,27]In a prospective study on 198 EEGs, Privitera et al[27]found that EEG is necessary since prior history and clinical findings could not predict which patients are going to show NSE on EEG. Two other studies reported that EEG contributes to diagnosis of patients with AMS in 56%–77% of the patients, and change the treatment plan in 38%–42% of the cases.[5,6]
The main limitation of our study is its retrospective design. Also, our NCS sample size was not large enough to perform a conclusive multivariate analysis. Therefore,the results of our multivariable analysis should be interpreted with caution. Prospective studies with a larger sample size are needed to confirm the findings.
Another limitation is low reliability among EEG interpretations. This issue has been addressed in the literature extensively.[18]We chose to use the interpretation by the on-call epileptologist because they had access to clinical information.
The objectives of our original trails were to assess the prevalence of EEG abnormalities in ED patients with AMS[5]and also to assess the impact of microEEG on clinical management of AMS patients.[6]Therefore, we did not study the etiology or treatment of NCS/NCSE.We are currently embarking on a new study with the objective of measuring the impact of early diagnosis and treatment of NCS/NCSE on patient-oriented outcomes.Also, we only compared NCS to all other types of EEG readings (including normal and abnormal) and did not compare presentation of other abnormal types of EEG(Interictal epileptiform waves in 8% and diffuse slowing in 79% of the EEG readings).[6]CONCLUSION
In conclusion, other than age, there is no other clinically useful variable from medical history, physical examination, or laboratory testing that could identify patients at high risk of NCS/NCSE. Therefore, ED physicians should have a high index of suspicion for NCS/NCSE in ED patients with AMS and should order EEG for these patients more liberally.
Funding: The study was supported by NIH grant 1RC3NS070658 to Bio-Signal Group Inc.
Ethical approval: The study was approved by the joint institutional review board, which waived the requirement for informed consent.Conflicts of interest: First and last authors received salary support through a subcontract to Downstate Medical Center. Presented in abstract form at the 2015 annual meeting of the Society for Academic Emergency Medicine (San Diego, CA).
Contributors: SZ and GSR designed the study. All authors were involved in data collection and analysis. GSR drafted the manuscript. All others had significant input in revising the manuscript.
1 Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, et al. A definition and classification of status epilepticus: Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015;56(10):1515–23.
2 Meierkord H, Holtkamp M. Non-convulsive status epilepticus in adults: clinical forms and treatment. Lancet Neurol.2007;6(4):329–39.
3 Shneker BF, Fountain NB. Assessment of acute morbidity and mortality in nonconvulsive status epilepticus. Neurology.2003;61(8):1066–73.
4 Drislane FW. Presentation, evaluation, and treatment of nonconvulsive status epilepticus. Epilepsy Behav. 2000;1(5):301–14.
5 Zehtabchi S, Abdel Baki SG, Omurtag A, Sinert R, Chari G,Malhotra S, et al. Prevalence of non-convulsive seizure and other electroencephalographic abnormalities in ED patients with altered mental status. Am J Emerg Med. 2013;31(11):1578–82.
6 Zehtabchi S, Abdel Baki SG, Omurtag A, Sinert R, Chari G,Roodsari GS, et al. Effect of microEEG on clinical management and outcomes of emergency department patients with altered mental status: a randomized controlled trial. Acad Emerg Med.2014;21(3):283–91.
7 Praline J, Abdel Baki SGP, Lucas B, Hommet C, Autret A,et al. Emergent EEG in clinical practice. Clin Neurophysiol.2007;118(10):2149–55. Epub 2007 Aug 20.
8 Kaplan PW. Nonconvulsive status epilepticus in the emergency room. Epilepsia 1996;37(7):643–50.
9 Chicharro-Ciuffardi A, González-Silva M, de Marinis-Palombo A, Gabler-Santalices G. Psychiatric disorders secondary to nonconvulsive status epilepticus of frontal origin. Two clinical case reports. Actas Esp Psiquiatr. 2012;40(3):155–60.
10 Korn-Lubetzki I, Steiner-Birmanns B, Galperin I, Benasouli Y,Steiner I. Nonconvulsive status epilepticus in older people: a diagnostic challenge and a treatable condition. J Am Geriatr Soc.2007;55(9):1475–6.
11 Woodford HJ, George J, Jackson M. Non-convulsive status epilepticus: a practical approach to diagnosis in confused older people. Postgrad Med J. 2015; 91(1081):655–61.
12 Abdel Baki SG, Omurtag A, Fenton AA, Zehtabchi S. The new wave: time to bring EEG to the emergency department. Int J Emerg Med. 2011;4:36.
13 DeGiorgio CM, Heck CN, Rabinowicz AL, Gott PS, Smith T,Correale J. Serum neuron-specific enolase in the major subtypes of status epilepticus. Neurology 1999;52(4):746–9.
14 Fountain NB. Status epilepticus: risk factors and complications.Epilepsia 2000;41 Suppl 2:S23–30.
15 Krumholz A. Epidemiology and evidence for morbidity of nonconvulsive status epilepticus. J Clin Neurophysiol.1999;16(4):314–22.
16 Young GB, Jordan KG, Doig GS. An assessment of nonconvulsive seizures in the intensive care unit using continuous EEG monitoring: an investigation of variables associated with mortality.Neurology. 1996;47(1):83–9.
17 Bottaro FJ, Martinez OA, Pardal MM, Bruetman JE, Reisin RC.Nonconvulsive status epilepticus in the elderly: a case-control study. Epilepsia. 2007;48(5):966–72.
18 de Assis T, Costa G, Bacellar A, Orsini M, Nascimento O. Status epilepticus in the elderly: epidemiology, clinical aspects and treatment. Neurol Int. 2012; 4(3): e17.
19 Grant AC, Abdel-Baki SG, Omurtag A, Sinert R, Chari G,Malhotra S, et al. Diagnostic accuracy of microEEG: a miniature,wireless EEG device. Epilepsy Behav. 2014;34:81–5.
20 Shavit L, Grenader T, Galperin I. Nonconvulsive status epilepticus in elderly a possible diagnostic pitfall. Eur J Intern Med. 2012;23(8):701–4.
21 Tu TM, Loh NK, Tan NC. Clinical risk factors for non-convulsive status epilepticus during emergent electroencephalogram.Seizure. 2013;22(9):794–7.
22 Marjan A, Mahtab R, Ehsan K, Hadi M. Generalized seizure,the only manifestation of a small ischemic atherothrombotic infarction. World J Emerg Med. 2016;7(1):71–3.
23 Husain AM, Horn GJ, Jacobson MPJ. Non-convulsive status epilepticus: usefulness of clinical features in selecting patients for urgent EEG. Neurol Neurosurg Psychiatry. 2003;74(2):189–91.
24 Fernández-Torre JL, Kaplan PW, Hernández MA. New understanding of nonconvulsive status epilepticus in adults:treatments and challenges. Expert Rev Neurother. 2015;15(12):1455–73.
25 Tomson T, Lindbom U, Nilsson BY. Nonconvulsive status epilepticus in adults: thirty-two consecutive patients from a general hospital population. Epilepsia. 1992;33(5):829–35.
26 Ziai WC, Schlattman D, Llinas R, Venkatesha S, Truesdale M, Schevchenko A, et al. Emergent EEG in the emergency department in patients with altered mental states. Clin Neurophysiol. 2012;123(5):910–7.
27 Privitera M, Hoffman M, Moore JL, Jester D. EEG detection of non tonic–clonic status epilepticus in patients with altered consciousness. Epilepsy Res. 1994;18(2):155–66.
Accepted after revision April 29, 2017
Gholamreza Sadeghipoor Roodsari, Email: roodsaris@gmail.com
World J Emerg Med 2017;8(3):190–194
10.5847/wjem.j.1920–8642.2017.03.005
November 6, 2016
 World journal of emergency medicine2017年3期
World journal of emergency medicine2017年3期
- World journal of emergency medicine的其它文章
- A case of exercise induced rhabdomyolysis from calf raises
- Instructions for Authors
- Iatrogenic Horner's syndrome: A cause for diagnostic confusion in the emergency department
- Ocular mutilation: A case of bilateral self-evisceration in a patient with acute psychosis
- Blunt injury to the thyroid gland: A case of delayed surgical emergency
- Validation of different pediatric triage systems in the emergency department
