淋巴细胞计数和血小板/淋巴细胞比率与急性缺血性脑血管病的关系研究
郎娅淞,张月战
·论著·
淋巴细胞计数和血小板/淋巴细胞比率与急性缺血性脑血管病的关系研究
郎娅淞,张月战
目的分析淋巴细胞计数、血小板/淋巴细胞比率(PLR)与急性缺血性脑血管病的关系。方法选取2014年3月—2016年9月南京中医药大学连云港附属医院神经内科和急诊科收治的急性缺血性脑血管病患者193例,其中短暂性脑缺血发作(TIA)患者65例(TIA组),急性脑梗死(ACI)患者128例(ACI组);另选取同期体检健康者60例作为对照组。随访1个月,根据格拉斯哥预后量表(GOS)评分将ACI患者分为预后良好组98例和预后不良组30例。比较3组受试者血小板计数(PLT)、淋巴细胞计数及PLR,比较不同预后ACI患者临床资料、PLT、淋巴细胞计数及PLR,淋巴细胞计数和PLR与ACI患者GOS评分的相关性分析采用Spearman秩相关性分析。结果3组受试者PLT比较,差异无统计学意义(P>0.05);ACI组和TIA组患者淋巴细胞计数低于对照组,PLR高于对照组(P<0.05);ACI组患者淋巴细胞计数低于TIA组,PLR高于TIA组(P<0.05)。不同预后ACI患者性别和PLT比较,差异无统计学意义(P>0.05);预后良好组患者年龄小于预后不良组,淋巴细胞计数高于预后不良组,PLR低于预后不良组(P<0.05)。协方差分析结果显示,校正年龄后,预后良好组与预后不良组患者PLT、淋巴细胞计数及PLR比较,差异均无统计学意义(P>0.05)。Spearman秩相关性分析结果显示,淋巴细胞计数与ACI患者GOS评分呈正相关(rs=0.268,P=0.002),PLR与ACI患者GOS评分呈负相关(rs=-0.336,P<0.001)。结论淋巴细胞计数、PLR可初步鉴别诊断ACI和TIA,且淋巴细胞计数和PLR均与ACI患者短期预后有关。
脑缺血;脑梗死;脑缺血发作,短暂性;淋巴细胞计数;血小板/淋巴细胞比率
卒中是全球范围内第二位致死疾病和第三位减寿疾病[1],其中缺血性脑血管病约占全部卒中的85%[2]。我国是卒中高发国家,据统计卒中年发病人数约为250万,年致死人数约为160万,已成为我国第一位致死和致残性疾病[3],给家庭和社会带来沉重的负担。急性缺血性脑血管病包括短暂性脑缺血发作(TIA)和急性脑梗死(ACI),两者均属于急诊科和神经内科常见病,但由于两者病情严重程度不一,能否早期进行鉴别诊断、给予有针对性的治疗对急性缺血性脑血管病患者预后具有重要的临床意义。既往研究证实,炎性反应参与了缺血性脑血管病的发病过程[4-6]。ALTINTAS等[7]研究显示,血小板/淋巴细胞比率(PLR)与接受血管腔内治疗的缺血性脑卒中患者预后、血管再通率及梗死面积有关,但国内外有关淋巴细胞计数、PLR与ACI、TIA患者相关性的研究报道较少。本研究旨在分析淋巴细胞计数和PLR与急性缺血性脑血管病患者的关系,旨在为ACI和TIA的早期鉴别诊断及ACI患者短期预后评估提供参考。
1 资料与方法
1.1 一般资料 选取2014年3月—2016年9月南京中医药大学连云港附属医院神经内科和急诊科收治的急性缺血性脑血管病患者193例,符合美国心脏协会/美国中风协会发布的ACI、TIA诊断标准[8],且经颅脑CT或MRI检查确诊。所有患者中TIA患者65例(TIA组),ACI患者128例(ACI组)。TIA组中男37例,女28例;年龄41~92岁,平均年龄(64.9±11.2)岁。ACI组中男80例,女48例;年龄39~95岁,平均年龄(67.6±11.8)岁。排除标准:(1)发病24 h后入院者;(2)有脑卒中病史并遗留明显后遗症者;(3)合并血液系统或风湿免疫系统疾病、急性冠脉综合征、急性脑出血、严重肝肾功能不全及肿瘤者;(4)有免疫抑制药物服用史者;(5)近两周内有创伤或手术者;(6)病历资料不完整及拒绝配合随访者。另选取同期南京中医药大学连云港附属医院体检中心体检健康者60例作为对照组,其中男37例,女23例;年龄36~87岁,平均年龄(66.1±9.8)岁。3组受试者性别(χ2=0.584)、年龄(F=1.312)比较,差异无统计学意义(P>0.05),具有可比性。所有受试者或家属知情并同意参加本研究。
1.2 随访 随访1个月,根据格拉斯哥预后量表(GOS)评分将ACI患者分为预后良好组(GOS评分4~5分)98例和预后不良组(GOS评分1~3分)30例。
1.3 观察指标 急性缺血性脑血管病患者于入院24 h内、体检健康者于体检当天采用EDTA-K2抗凝真空管采集静脉血2 ml,抽血后2 h内完成检测,采用SYSMEX XE-2100型血细胞分析仪检测血小板计数(PLT)和淋巴细胞计数,试剂盒为选用仪器公司匹配试剂盒,严格按照说明书进行操作,PLT参考范围为(125~350)×109/L、淋巴细胞计数参考范围为(1.1~3.2)×109/L。并按公式计算PLR,PLR=PLT/淋巴细胞计数。

2 结果
2.1 3组受试者PLT、淋巴细胞计数和PLR比较 3组受试者PLT比较,差异无统计学意义(P>0.05);3组受试者淋巴细胞计数和PLR比较,差异有统计学意义(P<0.05)。ACI组和TIA组患者淋巴细胞计数低于对照组,PLR高于对照组,差异有统计学意义(P<0.05);ACI组患者淋巴细胞计数低于TIA组,PLR高于TIA组,差异有统计学意义(P<0.05,见表1)。
Table1ComparisonofPLT,lymphocytecountandPLRamongthethreegroups
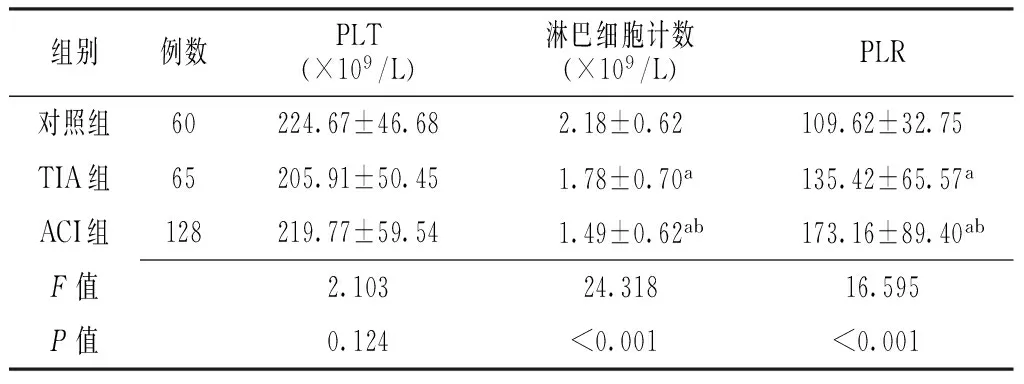
组别例数PLT(×109/L)淋巴细胞计数(×109/L)PLR对照组60224.67±46.682.18±0.62109.62±32.75TIA组65205.91±50.451.78±0.70a135.42±65.57aACI组128219.77±59.541.49±0.62ab173.16±89.40abF值2.10324.31816.595P值0.124<0.001<0.001
注:PLT=血小板计数,PLR=血小板/淋巴细胞比率,TIA=短暂性脑缺血发作,ACI=急性脑梗死;与对照组比较,aP<0.05;与TIA组比较,bP<0.05
2.2 不同预后ACI患者临床资料、PLT、淋巴细胞计数及PLR比较 不同预后ACI患者性别和PLT比较,差异无统计学意义(P>0.05);预后良好组患者年龄小于预后不良组,淋巴细胞计数高于预后不良组,PLR低于预后不良组,差异有统计学意义(P<0.05,见表2)。协方差分析结果显示,校正年龄后,两组患者PLT、淋巴细胞计数及PLR比较,差异均无统计学意义(F值分别为0.007、1.538、2.889,P>0.05)。

Table2 Comparison of clinical data,PLT,lymphocyte count and PLR in ACI patients with different prognosis
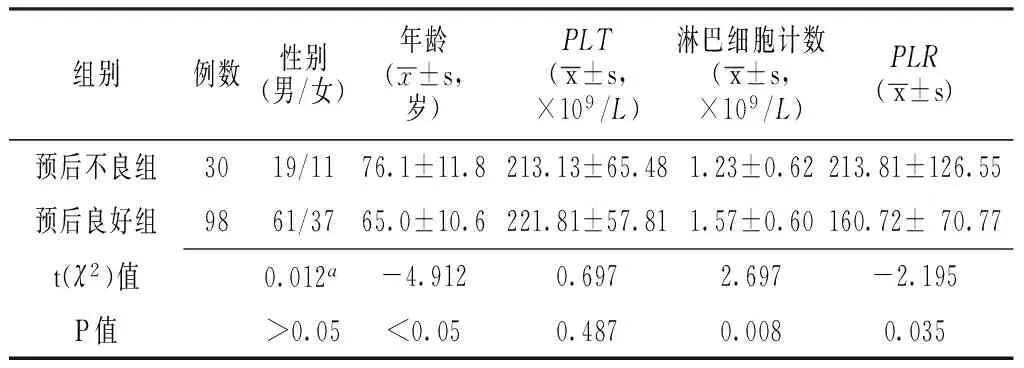
组别例数性别(男/女)年龄(x±s,岁)PLT(x±s,×109/L)淋巴细胞计数(x±s,×109/L)PLR(x±s)预后不良组3019/1176.1±11.8213.13±65.481.23±0.62213.81±126.55预后良好组9861/3765.0±10.6221.81±57.811.57±0.60160.72±70.77t(χ2)值0.012a-4.9120.6972.697-2.195P值>0.05<0.050.4870.0080.035
注:a为χ2值
2.3 相关性分析 Spearman秩相关性分析结果显示,淋巴细胞计数与ACI患者GOS评分呈正相关(rs=0.268,P=0.002);PLR与ACI患者GOS评分呈负相关(rs=-0.336,P<0.001)。
3 讨论
既往研究证实,血小板参与脑梗死的发病过程[9-10]。脑梗死后局部血管不完全或完全闭塞导致血管内皮损伤、微血管系统变形能力下降,会激活流经的血小板及促进血小板破坏,进而释放P-选择素,促使血小板表面膜糖蛋白黏附于血管壁并相互聚集,进一步加重脑缺血。由于血小板聚集破坏消耗,骨髓造血系统受刺激后可生成新的血小板,故脑梗死急性期PLT可能出现一定变化,但目前尚存在争议[11-12],推测可能与脑梗死后检测时间不同有关,具体原因有待进一步研究证实。D′ERASMO等[11]研究显示,与健康对照者相比,ACI患者发病后第3天PLT明显降低,发病后第9天PLT逐渐恢复正常。但ICME等[12]研究显示,ACI、急性脑出血和TIA患者PLT中位数间无差异,ACI与健康对照者PLT间亦无差异,本研究结果与之相一致,故推测PLT无法应用于ACI、TIA的早期鉴别诊断及ACI患者的预后评估。
既往研究已证实,炎症与卒中的发生发展密切相关[5-6]。卒中后免疫抑制(淋巴细胞参与)与免疫应答间的平衡一旦被打破,会引起脑缺血进一步加重甚至导致二次损伤。HAEUSLER等[13]研究显示,ACI发生后淋巴细胞计数有减少现象,且至少持续6 d。KIM等[14]研究显示,淋巴细胞计数减少程度与ACI患者入院后1周改善程度及3个月不良预后密切相关。本研究结果显示,TIA组和ACI组患者淋巴细胞计数低于对照组,ACI组患者淋巴细胞计数低于TIA组,表明TIA和ACI分别属于缺血性脑血管病发生发展的两个不同阶段,且淋巴细胞参与的免疫抑制程度可能不同,故淋巴细胞计数可用于ACI和TIA的早期鉴别诊断。另外,本研究结果还显示,ACI预后不良组患者淋巴细胞计数低于预后良好组,提示淋巴细胞计数与ACI患者短期预后有关。但BHARDWAJ等[15]认为,年龄是脑梗死患者预后的独立影响因素,而YOO等[16]持有不同观点。因此,本研究采用协方差分析,结果显示,校正年龄后,不同预后ACI患者淋巴细胞计数间无差异。
PLR作为一个新型炎性指标,已被用于心脑血管疾病的临床研究[7,17]。但有关PLR与ACI、TIA关系的研究报道较少。本研究结果显示,TIA组和ACI组患者PLR高于对照组,ACI组患者PLR高于TIA组,提示PLR可用于ACI和TIA的早期鉴别诊断。本研究结果还显示,预后不良组患者PLR高于预后良好组,与ALTINTAS等[7]研究结果相一致;但校正年龄后,不同预后ACI患者PLR间无差异。因此,为了分析淋巴细胞计数和PLR与ACI患者预后的关系,本研究进行了Spearman秩相关性分析,结果显示,淋巴细胞计数与ACI患者GOS评分呈正相关,PLR与ACI患者GOS评分呈负相关,提示淋巴细胞计数、PLR均与ACI短期预后有关。
综上所述,淋巴细胞计数和PLR可初步鉴别诊断ACI和TIA,且淋巴细胞计数和PLR与ACI患者短期预后有关;淋巴细胞计数和PLR检测简便、经济,具有一定临床推广价值。但本研究样本量较小,未根据脑梗死类型、梗死面积进行亚组分析,未考虑抗血小板药物对检测结果的影响,且未动态观察淋巴细胞计数和PLR变化,因此研究结果结论等还需进一步研究证实。
作者贡献:张月战进行文章的构思与设计、结果分析与解释、负责文章的质量控制及审校,对文章整体负责,监督管理;郎娅淞进行数据收集、整理、分析,撰写论文。
本文无利益冲突。
[1]LOZANO R,NAGHAVI M,FOREMAN K,et al.Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010:a systematic analysis for the Global Burden of Disease Study 2010[J].Lancet,2012,380(9859):2095-2128.DOI:10.1016/S0140-6736(12)61728-0.
[2]BEVERS M B,KIMBERLY W T.Critical care management of acute ischemic stroke[J].Curr Treat Options Cardiovasc Med,2017,19(6):41.DOI:10.1007/s11936-017-0542-6.
[3]WANG Z,HU S,SANG S,et al.Age-period-cohort analysis of stroke mortality in China:data from the global burden of disease study 2013[J].Stroke,2017,48(2):271-275.DOI:10.1161/STROKEAHA.116.015031.
[4]JIN R,YANG G,LI G.Inflammatory mechanisms in ischemic stroke:role of inflammatory cells[J].J Leukoc Biol,2010,87(5):779-789.DOI:10.1189/jlb.1109766.
[5]ANRATHER J,IADECOLA C.Inflammation and stroke:an overview[J].Neurotherapeutics,2016,13(4):661-670.
[6]BREA D,SOBRINO T,RAMOS-CABRER P,et al.Inflammatory and neuroimmunomodulatory changes in acute cerebral ischemia[J].Cerebrovasc Dis,2009,27(Suppl 1):48-64.DOI:10.1159/000200441.
[7]ALTINTAS O,ALTINTAS M O,TASAL A,et al.The relationship of platelet-to-lymphocyte ratio with clinical outcome and final infarct core inacute ischemic stroke patients who have undergone endovascular therapy[J].Neurol Res,2016,38(9):759-765.DOI:10.1080/01616412.2016.1215030.
[8]SACCO R L,KASNER S E,BRODERICK J P,et al.An updated definition of stroke for the 21st century a statement for healthcare professionals from the American heart association/American stroke association[J].Stroke,2013,44(7):2064-2089.DOI:10.1161/STR.0b013e318296aeca.
[10]KOZUBSKI W.Role of blood platelets in pathogenesis of ischemic cerebral infarction[J].Postepy Hig Med Dosw,1992,46(3):309-318.
[11]D′ERASMO E,ACCA M,CELI F S,et al.Plasma fibrinogen and platelet count in stroke[J].J Med,1993,24(2/3):185-191.
[12]ICME F,ÖZGÜR D N,YÜCEL Y,et al.Prognostic relationship between complete blood count parameters and transient ischemic attack,ischemic stroke and hemorrhagic stroke[J].Turk Geriatri Dergisi,2014,17(1):23-28.
[13]HAEUSLER K G,SCHMIDT W U,FÖHRING F,et al.Cellular immunodepression preceding infectious complications after acute ischemic stroke in humans[J].Cerebrovasc Dis,2008,25(1/2):50-58.
[14]KIM J,SONG T J,PARK J H,et al.Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction[J].Atherosclerosis,2012,222(2):464-467.DOI:10.1016/j.atherosclerosis.2012.02.042.
[15]BHARDWAJ A,SHARMA G,RAINA S K,et al.Advanced age and higher national institutes of health stroke scale score as predictors of poor outcome in ischemic stroke patients treated with alteplase:A study from a tertiary care centre in rural north-west India[J].J Neurosci Rural Pract,2017,8(2):236-240.DOI:10.4103/jnrp.jnrp_431_16.
[16]YOO B R,YOO C J,KIM M J,et al.Analysis of the outcome and prognostic factors of decompressive craniectomy between young and elderly patients for acute middle cerebral artery infarction[J].J Cerebrovasc Endovasc Neurosurg,2016,18(3):175-184.
[17]TEMIZ A,GAZI E,GÜNGÖR Ö,et al.Platelet/lymphocyte ratio and risk of in-hospital mortality in patients with ST-elevated myocardial infarction[J].Med Sci Monit,2014,20(233):660-665.DOI:10.12659/MSM.890152.
(本文编辑:谢武英)
RelationshipbetweenLymphocyteCount,Platelet/LymphocyteRatioandAcuteIschemicCerebrovascularDisease
LANGYa-song,ZHANGYue-zhan
EmergencyICU,LianyungangHospitalAffiliatedtoNanjingUniversityofTraditionalChineseMedicine,Lianyungang222000,China
Correspondingauthor:ZHANGYue-zhan,E-mail:zhangyz1979@sohu.com
ObjectiveTo analyze the relationship between lymphocyte count,platelet/lymphocyte ratio(PLR) and acute ischemic cerebrovascular disease.MethodsFrom March 2014 to September 2016,a total of 193 patients with acute ischemic cerebrovascular disease were selected in the Department of Neurology and Emergency,Lianyungang Hospital Affiliated to Nanjing University of Traditional Chinese Medicine,thereinto 65 patients with transient ischemic attack were served as TIA group,other 128 patients with acute cerebral infarction were served as ACI group;meanwhile a total of 60 healthy people were selected as control group.Patients of ACI group were divided into A group(with good prognosis,n=98) and B group(with poor prognosis,n=30) according to the GOS score after 1-month follow-up.Blood platelet count(PLT),lymphocyte count and PLR were compared among the TIA group,ACI group and control group.Clinical data,PLT,lymphocyte count and PLR were compared in acute cerebral infarction patients with different prognosis;correlations lymphocyte count and PLR with GOS score in patients with acute cerebral infarction were analyzed by Spearman rank correlation analysis.ResultsNo statistically significant differences of PLT was found among TIA group,ACI group and control group(P>0.05);lymphocyte count of ACI group and TIA group was statistically significantly lower than that of control group,respectively,while PLR of ACI group and TIA group was statistically significantly higher than that of control group,respectively(P<0.05);lymphocyte count of ACI group was statistically significantly lower than that of TIA group,while PLR of ACI group was statistically significantly higher than that of TIA group(P<0.05).No statistically significant differences of gender or PLT was found between A group and B group(P>0.05);age of A group was statistically significantly younger than that of B group,lymphocyte count of A group was statistically significantly higher than that of B group,while PLR of A group was statistically significantly lower than that of B group(P<0.05).Covariance analysis results showed that,no statistically significant differences of PLT,lymphocyte count or PLR was found between A group and B group after correction of age(P>0.05).Spearman rank correlation analysis results showed that,lymphocyte count was positively correlated with GOS score in patients with acute cerebral infarction(rs=0.268,P=0.002),while PLR was negatively correlated with GOS score in patients with acute cerebral infarction(rs=-0.336,P<0.001).ConclusionLymphocyte count and PLR have preliminary differential diagnostic value between transient ischemic attack and acute cerebral infarction,meanwhile lymphocyte count and PLR are significantly correlated with short-term prognosis in patients with acute cerebral infarction.
Brain ischemia;Brain infarction;Ischemic attack,transient;Lymphocyte count;Platelet/lymphocyte ratio
张月战,E-mail:zhangyz1979@sohu.com
R 743.31
A
10.3969/j.issn.1008-5971.2017.08.005
2017-05-23;
2017-08-14)
222000江苏省连云港市,南京中医药大学连云港附属医院急诊ICU
郎娅淞,张月战.淋巴细胞计数和血小板/淋巴细胞比率与急性缺血性脑血管病的关系研究[J].实用心脑肺血管病杂志,2017,25(8):20-23.[www.syxnf.net]
LANG Y S,ZHANG Y Z.Relationship between lymphocyte count,platelet/lymphocyte ratio and acute ischemic cerebrovascular disease[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2017,25(8):20-23.