急性缺血性脑卒中患者阿司匹林致上消化道出血情况及其影响因素研究
范 琳,刘 颖,黄 晶,黄玉静,吴正刚
·论著·
急性缺血性脑卒中患者阿司匹林致上消化道出血情况及其影响因素研究
范 琳,刘 颖,黄 晶,黄玉静,吴正刚
目的 分析急性缺血性脑卒中(AIS)患者阿司匹林致上消化道出血情况及其影响因素。方法 选取2012-01-01至2015-06-30泰州市人民医院收治的AIS患者907例,住院期间均常规给予阿司匹林治疗,出院后随访18个月,记录其出血情况,AIS患者阿司匹林致上消化道出血的影响因素分析采用多因素Logistic回归分析。结果 907例患者随访过程中剔除85例,最终纳入822例患者,阿司匹林致上消化道出血发生率为6.4%(53/822);出血时间:AIS后0~3个月20例(占37.7%),AIS后4~6个月12例(占22.6%),AIS后7~9个月6例(占11.4%),AIS后10~12个月6例(占11.4%),AIS后13~15个月4例(占7.5%),AIS后16~18个月5例(占9.4%);出血原因:急性胃黏膜损伤26例(占49.1%),十二指肠溃疡17例(占32.1%),胃溃疡8例(占15.0%),食管炎1例(占1.9%),胃癌1例(占1.9%)。有无阿司匹林致上消化道出血患者男性比例、吸烟史、服药规律者所占比例及联用氯吡格雷者所占比例比较,差异无统计学意义(P>0.05);有无阿司匹林致上消化道出血患者年龄、饮酒史、幽门螺杆菌(Hp)感染发生率、既往有消化道不适症状者所占比例、有消化道出血史及联用质子泵抑制剂(PPI)者所占比例比较,差异有统计学意义(P<0.05)。多因素Logistic回归分析结果显示,年龄〔OR=2.246,95%CI(1.162,4.339)〕、饮酒史〔OR=1.900,95%CI(1.065,3.390)〕、Hp感染〔OR=9.013,95%CI(5.008,16.232)〕及有消化道出血史〔OR=3.196,95%CI(1.632,6.261)〕是AIS患者阿司匹林致上消化道出血的危险因素(P<0.05),联用PPI是AIS患者阿司匹林致上消化道出血的保护因素〔OR=0.467,95%CI(0.250,0.873),P<0.05〕。结论 AIS患者阿司匹林致上消化道出血发生率较高,出血主要发生在AIS后6个月内,主要出血原因为急性胃黏膜损伤和十二指肠溃疡;年龄、饮酒史、Hp感染及有消化道出血史是AIS患者阿司匹林致上消化道出血的危险因素,联用PPI是AIS患者阿司匹林致上消化道出血的保护因素。
脑缺血;阿司匹林;上消化道出血;影响因素分析
范琳,刘颖,黄晶,等.急性缺血性脑卒中患者阿司匹林致上消化道出血情况及其影响因素研究[J].实用心脑肺血管病杂志,2017,25(7):53-56.[www.syxnf.net]
FAN L,LIU Y,HUANG J,et al.Incidence of aspirin-induced upper gastrointestinal hemorrhage and the influencing factors in patients with acute ischemic stroke[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2017,25(7):53-56.
急性缺血性脑卒中(acute ischemic stroke,AIS)是严重威胁人类健康的常见疾病,具有发病率高、复发率高、致残率高、病死率高等特点,目前,抗血小板聚集已成为AIS二级预防的重要内容[1]。阿司匹林(aspirin)是最常见的抗血小板聚集药物,其能有效降低脑卒中复发率[2],但长期使用阿司匹林可增加上消化道出血风险[3],进而导致患者住院率及经济负担增加等。本研究旨在分析AIS患者阿司匹林致上消化道出血情况及其影响因素,以降低上消化道出血发生率。
1 资料与方法
1.1 一般资料 选取2012-01-01至2015-06-30泰州市人民医院收治的AIS患者907例,均经磁共振成像确诊,所有患者对本研究知情同意并签署知情同意书。排除标准:(1)合并消化性溃疡活动期、炎性肠病者;(2)合并消化道肿瘤及血液系统疾病者;(3)由其他原因导致上消化道出血者。
1.2 治疗及随访方法 住院期间所有患者常规给予阿司匹林治疗,100 mg/次,1次/d;出院后每月门诊或电话随访1次,每半年胃镜检查1次,若出现消化道出血则行急诊胃镜检查明确出血原因,共随访18个月。
1.3 观察指标 记录患者出血情况,包括阿司匹林致上消化道出血发生例数、出血时间及出血原因;记录患者临床资料,包括年龄、有无吸烟史(吸烟量>10支/d定义为吸烟)、有无饮酒史(饮酒量>150 ml/d定义为饮酒)、服药情况(遵医嘱服药定义为服药规律)、幽门螺杆菌(Hp)感染情况(胃镜检查Hp阳性定义为Hp感染)、既往有上消化道不适症状(包括上腹痛、返酸、胃灼热感等)、有无上消化道出血史(出现消化性溃疡、糜烂性胃炎及急性胃黏膜损伤定义为上消化道出血)及联合用药情况。
1.4 阿司匹林致上消化道出血诊断标准 患者服用阿司匹林后出现不同程度呕血、黑便或隐血试验阳性(排除食用肉类、动物血所致的假阳性)或胃镜检查证实上消化道出血。

2 结果
2.1 随访结果 907例患者随访过程中剔除85例,包括失访25例、出院后自行停用阿司匹林54例、非上消化道出血原因死亡6例,最终纳入822例患者。
2.2 出血情况 822例患者发生阿司匹林致上消化道出血53例,阿司匹林致上消化道出血发生率为6.4%;出血时间:AIS后0~3个月20例(占37.7%),AIS后4~6个月12例(占22.6%),AIS后7~9个月6例(占11.4%),AIS后10~12个月6例(占11.4%),AIS后13~15个月4例(占7.5%),AIS后16~18个月5例(占9.4%);出血原因:急性胃黏膜损伤26例(占49.1%),十二指肠溃疡17例(占32.1%),胃溃疡8例(占15.0%),食管炎1例(占1.9%),胃癌1例(占1.9%)。
2.3 单因素分析 有无阿司匹林致上消化道出血患者男性比例、吸烟史、服药规律者所占比例及联用氯吡格雷者所占比例比较,差异无统计学意义(P>0.05);有无阿司匹林致上消化道出血患者年龄、饮酒史、Hp感染发生率、既往有消化道不适症状者所占比例、有消化道出血史及联用质子泵抑制剂(PPI)者所占比例比较,差异有统计学意义(P<0.05,见表1)。
2.4 多因素Logistic回归分析 以阿司匹林致上消化道出血为因变量,以年龄、饮酒史、Hp感染、既往有上消化道不适症状、有消化道出血史及联用PPI为自变量(变量赋值见表2)进行多因素Logistic回归分析,结果显示,年龄、饮酒史、Hp感染及有消化道出血史是AIS患者阿司匹林致上消化道出血的危险因素,联用PPI是AIS患者阿司匹林致上消化道出血的保护因素(P<0.05,见表3)。
3 讨论
临床研究表明,阿司匹林致消化道出血以上消化道出血为主[4]。目前,阿司匹林致上消化道出血的具体发生机制尚不明确,可能机制如下[5]:(1)阿司匹林作用于胃黏膜磷脂层后削弱胃黏膜疏水保护屏障;(2)阿司匹林为环氧合酶(COX)抑制剂,可阻断花生四烯酸合成前列腺素,从而减弱前列腺素对胃肠道黏膜的保护作用;(3)阿司匹林可直接抑制胃十二指肠上皮碳酸盐分泌,削弱黏液-碳酸氢盐的屏障保护作用;(4)阿司匹林能抑制肝脏合并凝血酶原;(5)当胃液pH值<3.5时阿司匹林可发生去离子化,进而激活胃蛋白酶而引发出血。本研究结果显示,AIS患者阿司匹林致上消化道出血发生率为6.4%,出血发生时间主要为AIS后6个月内,主要出血原因为急性胃黏膜损伤和十二指肠溃疡。BURGER等[6]研究结果显示,缺血性脑血管病患者突然停用阿司匹林可增加心脑血管疾病发生率,故不能随意停用阿司匹林或减少阿司匹林使用剂量。因此,预防阿司匹林致上消化道出血已成为临床研究热点。
本研究结果显示,年龄、饮酒史、Hp感染及有消化道出血史是AIS患者阿司匹林致上消化道出血的危险因素,联用PPI是AIS患者阿司匹林致上消化道出血的保护因素,分析其原因可能如下:(1)老年患者存在血管脆性增加、收缩能力减退,胃黏膜萎缩、血流减少,胃黏膜保护防御功能及修复功能减弱等情况,故可增加出血风险,与LANAS等[7]研究结果相一致。(2)乙醇可通过多个途径增加出血风险:血清乙醇浓度升高可导致血小板计数减少、血小板功能减弱;乙醇可通过影响机体凝血系统而降低凝血功能,增加出血风险;乙醇对胃黏膜具有直接损伤作用,可增加上消化道黏膜损伤及出血风险;阿司匹林可增加血液中乙醇浓度[8],且两者具有协同作用,导致出血风险明显升高。(3)Hp可在胃黏膜产生氨气,释放空泡毒素,介导免疫反应,其分泌的炎性因子可导致消化道黏膜损伤。BARDOU等[9]研究结果显示,Hp感染是消化性溃疡出血的独立危险因素,故口服阿司匹林的患者应定期检测Hp。(4)有消化道出血史的患者出血风险较高。(5)PPI属于胃黏膜保护剂,可缓解阿司匹林对胃黏膜的损伤程度[10-11]。
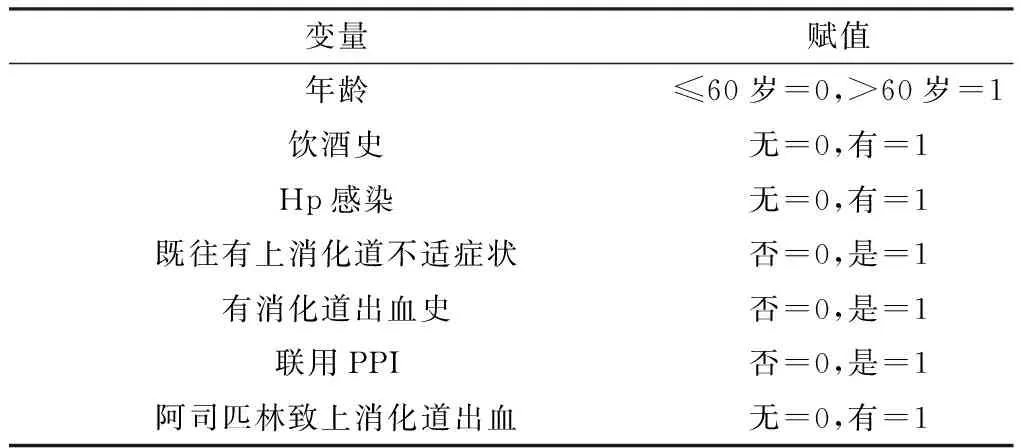
表2 变量赋值
表3 AIS患者阿司匹林致上消化道出血影响因素的多因素Logistic回归分析
Table 3 Multivariate Logistic regression analysis on influencing factors of aspirin induced- upper gastrointestinal hemorrhage in patients with AIS
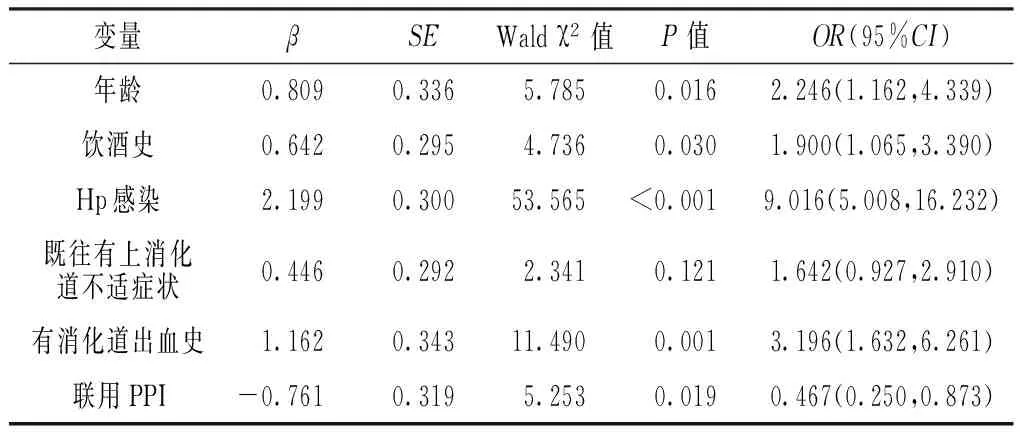
变量βSEWaldχ2值P值OR(95%CI)年龄0.8090.3365.7850.0162.246(1.162,4.339)饮酒史0.6420.2954.7360.0301.900(1.065,3.390)Hp感染2.1990.30053.565<0.0019.016(5.008,16.232)既往有上消化道不适症状0.4460.2922.3410.1211.642(0.927,2.910)有消化道出血史1.1620.34311.4900.0013.196(1.632,6.261)联用PPI-0.7610.3195.2530.0190.467(0.250,0.873)
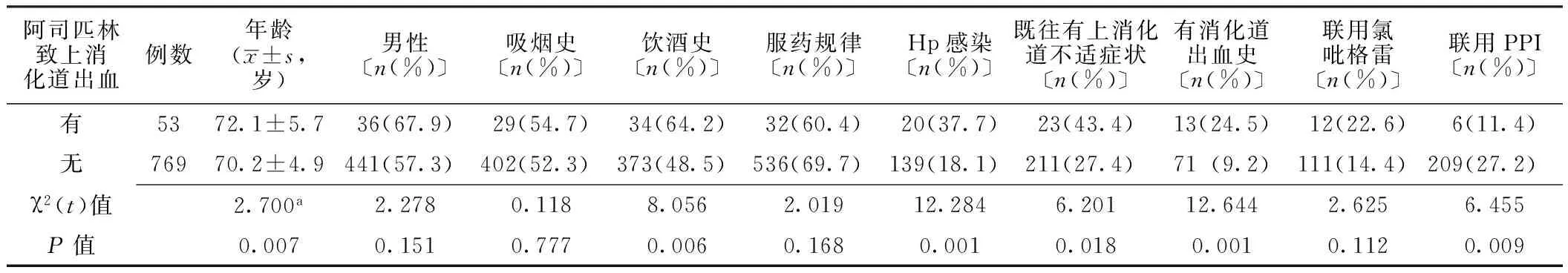
表1 有无阿司匹林致上消化道出血患者临床资料比较
注:a为t值;Hp=幽门螺杆菌,PPI=质子泵抑制剂
综上所述,AIS患者阿司匹林致上消化道出血发生率较高,出血主要发生在AIS后6个月内,主要出血原因为急性胃黏膜损伤和十二指肠溃疡,年龄、饮酒史、Hp感染及有消化道出血史是AIS患者阿司匹林致上消化道出血的危险因素,联用PPI是AIS患者阿司匹林致上消化道出血的保护因素,应引起临床重视。
作者贡献:范琳进行试验设计与实施、资料收集整理、撰写论文、成文并对文章负责;黄晶、黄玉静、吴正刚进行试验实施、评估、资料收集;刘颖进行质量控制及审校。
本文无利益冲突。
[1]WA D,ZHU P,LONG Z.Comparative Efficacy and Safety of Anti-Platelet Agents in Cerebral Ischemic Disease:A Network Meta-Analysis[J].J Cell Biochem,2017.DOI:10.1002/jcb.26065.
[2]AMARENCO P,KIM A S.Aspirin′s Benefits Were Previously Underestimated and Are Primarily Accrued in the Acute Setting[J].Stroke,2017,48(5):1438-1440.DOI:10.1161/STROKEAHA.117.015061.
[3]FELDMAN M,FRIEDMAN I S,BRANDT L J.Sleisenger and Fordtran′s gastrointestinal and liver disease:pathophysiology,diagnosis management[M].Elsevier Medicine,2010.
[4]SAPOZNIKOV B,VILKIN A.Minidose aspirin and gastrointestinal bleed-A retrospective,case-control study in hospitalized patients[J].Dig Dis Sci,2005,50(9):1621-1624.
[5]NEGOVAN A,IANCU M,MOLDOVAN V,et al.Clinical Risk Factors for Gastroduodenal Ulcer in Romanian Low-Dose Aspirin Consumers[J].Gastroenterol Res Pract,2016,2016:7230626.DOI:10.1155/2016/7230626.
[6]BURGER W,CHEMNITIUS J M,KNEISSL G D,et al.Low-dose aspirin for secondary cardiovascular prevention cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation review and meta-analysis[J].J Intern Med,2005,257(5):399-414.
[7]LANAS A,PEREZ-AISA M A,FEU F,et al.A nationwide study of mortality associated with hospital admission due to severe gastrointestinal events and those associated with nonsteroidal anti inflammatory drug use[J].Am J Gastroenterol,2005,100(8):1685-1693.
[8]GENTRY R T,BARAONA E,AMIR I,et al.Mechanism of the aspirin induced rise in blood alcohol levels[J].Life Sci,1999,65(23):2505-2512.
[9]BARDOU M,BARKUN A N.Preventing the gastrointestinal adverse effects of nonsteroidal anti inflammatory drugs:from risk factor identification to risk factor intervention[J].Joint Bone Spine,2010,77(1):6-12.DOI:10.1016/j.jbspin.2009.11.008.
[10]XU H,PING Y,LIN H,et al.Antiplatelet Strategies and Outcomes in Patients with Noncardioembolic Ischemic Stroke from a Real-World Study with a Five-Year Follow-Up[J].Transl Stroke Res,2017,8(3):228-233.DOI:10.1007/s12975-016-0516-0.
[11]ALVAREZ-SABN J,QUINTANA M,SANTAMARINA E,et al.Triflusal and aspirin in the secondary prevention of atherothrombotic ischemic stroke:a very long-term follow-up[J].Cerebrovasc Dis,2014,37(3):181-187.DOI:10.1159/000357662.
(本文编辑:谢武英)
Incidence of Aspirin-induced Upper Gastrointestinal Hemorrhage and the Influencing Factors in Patients with Acute Ischemic Stroke
FANLin,LIUYing,HUANGJing,HUANGYu-jing,WUZheng-gang
DepartmentofNeurology,thePeople′sHospitalofTaizhou,Taizhou225300,China
Objective To analyze the incidence of aspirin-induced upper gastrointestinal hemorrhage and the influencing factors in patients with acute ischemic stroke.Methods A total of 907 patients with acute ischemic stroke were selected in the People′s Hospital of Taizhou from 2012-01-01 to 2015-06-30,all of them
aspirin during hospitalization and were followed up for 18 months after discharge,incidence of aspirin-induced upper gastrointestinal hemorrhage was recorded,and influencing factors of aspirin-induced upper gastrointestinal hemorrhage in patients with acute ischemic stroke were analyzed by multivariate Logistic regression analysis.Results A total of 85 patients were rejected during the follow-up,therefore a total of 822 patients enrolled in this study at last;the incidence of aspirin-induced upper gastrointestinal hemorrhage was 6.4%(53/822),hemorrhage occurrence time:20 cases during 0 to 3 months after attack(accounting for 37.7%),12 cases during 4 to 6 months after attack(accounting for 22.6%),6 cases during 7 to 9 months after attack(accounting for 11.4%),6 cases during 10 to 12 months after attack(accounting for 11.4%),4 cases during 13 to 15 months after attack(accounting for 7.5%),5 cases during 16 to 18 months after attack(accounting for 9.4%);hemorrhage causes:26 cases with acute gastric mucosa injury(accounting for 49.1%),17 cases with duodenal ulcer(accounting for 32.1%),8 cases with gastric ulcer(accounting for 15.0%),1 case with oesophagitis(accounting for 1.9%),1 case with stomach cancer(accounting for 1.9%).No statistically significant differences of male ratio,smoking history,proportion of patients with regular medication or patients using clopidogrel in patients with or without aspirin-induced upper gastrointestinal hemorrhage(P>0.05),while there statistically significant differences of age,drinking history,Hp infection,proportion of patients with previous digestive tract discomfort,patients with history of gastrointestinal bleeding and patients using proton pump inhibitor(PPI)in patients with or without aspirin-induced upper gastrointestinal hemorrhage(P<0.05).Multivariate Logistic regression analysis results showed that,age〔OR=2.246,95%CI(1.162,4.339)〕,drinking history〔OR=1.900,95%CI(1.065,3.390)〕,Hp infection〔OR=9.013,95%CI(5.008,16.232)〕and history of gastrointestinal bleeding〔OR=3.196,95%CI(1.632,6.261)〕were risk factors of aspirin-induced upper gastrointestinal hemorrhage in patients with acute ischemic stroke(P<0.05),while using PPI was the protective factor〔OR=0.467,95%CI(0.250,0.873),P<0.05〕.Conclusion Incidence of aspirin-induced upper gastrointestinal hemorrhage and the influencing factors is relatively high in patients with acute ischemic stroke,mainly occurred after 6 months of attack,acute gastric mucosa injury and duodenal ulcer are the major hemorrhage causes;age,drinking history,Hp infection and history of gastrointestinal bleeding are risk factors of aspirin-induced upper gastrointestinal hemorrhage in patients with acute ischemic stroke,while using PPI was the protective factor.
Brain ischemia;Aspirin;Upper gastrointestinal bleeding;Root cause analysis
泰州市人民医院院级课题(ZL201624)
R 743.31
A
10.3969/j.issn.1008-5971.2017.07.012
2017-05-26;
2017-07-12)
225300江苏省泰州市人民医院神经内科

