抗NMDA受体脑炎6例及文献复习
赵超++张卓++段凤菊++严琪++周琼++白苗

[摘要] 本文主要探讨抗N-甲基-D-天冬氨酸(NMDA)受体脑炎患者临床表现、磁共振、脑脊液特点、治疗及预后,以提高对该病的认识。本文回顾性分析6例抗NMDA受体脑炎患者的相关临床资料,并复习相关文献。6例患者中,男3例,女3例,年龄15~61岁,所有患者血清及脑脊液抗NMDA受体抗体为阳性,1例患者脑脊液抗NMDA受体抗体及抗GABA受体抗体均为阳性;3例患者以癫痫发作为首发症状,3例以精神行为异常为首发症状;5例患者伴有不自主运动症状;头颅MRI:1例双侧丘脑DWI高信号;1例左侧颞叶T2、FLAIR高信号;其余4例正常;脑脊液化验结果与病毒性脑炎脑脊液特点相似;2例女性患者伴有畸胎瘤,1例患者伴有小细胞肺癌,经过免疫药物治疗后,症状均有不同程度恢复。抗NMDA受体脑炎以精神异常、癫痫发作为首发症状多见,抗NMDA受体脑炎患者可合并有抗GABA受体抗体阳性;部分患者核磁共振及脑脊液化验结果缺乏特异性。伴有肿瘤的患者,肿瘤切除及应用一线免疫抑制剂治疗,可显著改善预后。
[关键词] 抗N-甲基-天门冬氨酸受体脑炎;临床表现;核磁共振;脑脊液;治疗
[中图分类号] R651.2 [文献标识码] A [文章編号] 1673-7210(2017)01(b)-0175-04
A report of 6 cases with anti-N-methyl-D-aspartate receptor encephalitis and literature review
ZHAO Chao ZHANG Zhuo DUAN Fengju YAN Qi ZHOU Qiong BAI Miao MIAO Jianting LI Zhuyi
Department of Neurology, Tangdu Hospital, the Fourth Military Medical University, Shaanxi Province, Xi'an 710038, China
[Abstract] To improve the recognition of anti-N-methyl-D-aspartate (NMDA) receptor encephalitis, this paper analyzes the clinical presentation, magnetic resonance imaging (MRI), cerebrospinal fluid (CSF), treatment and prognosis. This paper analyzes the clinical data of 6 cases with anti-NMDA receptor encephalitis and reviews relevant literatures. Among 6 patients, 3 cases were male, 3 cases were female. The range of age was 15-61 years old. CSF and serum anti-NMDA receptor antibodies were positive in all patients. Anti-NMDA receptor antibodies and anti-GABA receptor antibodies were both positive in one patient. The epileptic attack as first symptom was observed in 3 patients. The mental and behavior disorder as first symptom was observed in 3 patients. 5 patients showed abnormal movements. The cranial MRI showed that DWI high signal intensity in bilateral thalamic regions in one patient. In another patient, the MRI showed T2/FLAIR high signal intensity in left temporal region, anti-NMDAR encephalitis of the left 4 patients showed no changes in the MRI. The CSF findings were in most respects similar to viral encephalitis: 2 cases had teratoma, one case had small cell lung carcinoma, and the symptoms were recovered inordinately after treatment of immunoagents. The first symptom of anti-NMDAR encephalitis was often psychiatric or seizures. Anti-NMDA receptor encephalitis patients could be combined with anti-GABA receptor antibody. The CSF and MRI findings in some patients were not specific. Patients associated with ovarian tumors underwent tumor excision and immunotherapy had remarkable efficacy.
[Key words] Anti-N-methyl-D-aspartate receptor encephalitis; Clinical symptoms; Magnetic resonance imaging; Cerebrospinal fluid; Treatment
抗N-甲基-D-天冬氨酸(NMDA)受体脑炎[1]属于自身免疫性脑炎,于2007年首次由Dalman报道,主要临床表现为癫痫发作、精神行为异常、不自主运动等,容易误诊为病毒性脑炎和精神障碍疾病。本文对6例抗NMDA受体脑炎患者进行临床资料分析。
1 病例资料
1.1 一般资料
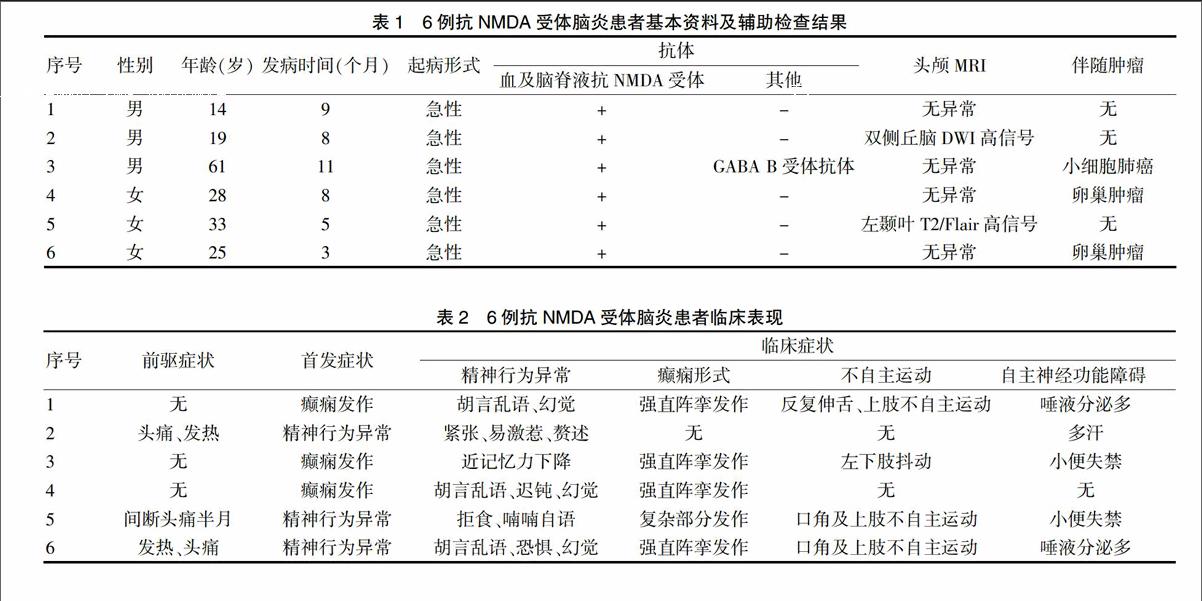
收集2015年3~12月于第四军医大学附属唐都医院神经内科确诊的抗NMDA受体脑炎患者6例,所有患者血清及脑脊液抗NMDA受体抗体均为阳性,1例患者合并有血清及脑脊液抗GABA B受体抗体阳性。见表1。
1.2 人口学特征
男3例,女3例,年龄15~61岁,平均30岁。见表1。
1.3 发病季节
6例患者发病时间分布于3~11月。见表1。
1.4 起病形式
所有患者均为急性起病。见表1。
1.5 前驅症状
前驱感染史者3例,均为低热、头痛,体温波动于37.5~39.0℃;另3例无明显诱因。见表2。
1.6 首发症状
以癫痫及精神行为异常为首发症状者各3例。见表2。
1.7 临床表现
所有患者伴有不同程度的胡言乱语、烦躁、恐惧、幻觉等精神症状及癫痫发作,其中4例患者出现不自主运动症状,5例患者出现植物神经功能紊乱症状。见表2。
1.8 头颅MRI
2例患者头颅MRI异常:1例双侧丘脑DWI高信号,1例左侧颞叶长T1、长T2信号,FLAIR高信号。其余4例正常。见表1。
1.9 脑电图表现
1例患者脑电图为慢波背景脑波,左侧各导可见单发尖慢波发放。1例患者脑电图呈弥漫性慢波,颞区为主,颞下颌切迹导联可见多次段阵中至高波幅尖慢波,以左侧颞区为著。其余患者脑电图未见明显异常。
1.10 脑脊液
1例正常,2例压力轻度升高,2例压力及白细胞数轻度升高,1例白细胞数及蛋白数均轻度升高。见表3。
表3 6例抗NMDA受体脑炎患者脑脊液特点
注:1 cmH2O=0.098 kPa
1.11 肿瘤
2例女性患者合并有卵巢畸胎瘤,1例老年男性患者合并有小细胞肺癌。见表1。
1.12 治疗
1例激素冲击治疗,2例均激素+丙球冲击治疗,3例肿瘤患者行激素+丙球冲击+手术切除。
1.13 预后
本组6例患者,入院时改良Rank评分总和为28分,出院6个月后进行随访,改良Rank评分总和降至6分,其中3例患者完全恢复正常。
2 讨论
2.1 病因
NMDA受体[2]是离子型谷氨酸受体的一种,在中枢神经系统的突触形成、突触可塑性、兴奋性毒性、记忆获得及学习中扮演重要作用,由来源于NR家族的3个(NR1、NR2、NR3)亚单位组成的异源四聚体,而有功能作用的NMDA受体主要是由2个NR1和2个NR2的不同排列组合组成(NR1/NR1/NR2A/NR2A,NR1/NR1/NR2B/NR2B,NR1/NR1/NR2C/NR2C)[3]。NR1亚单位包含一个甘氨酸结合区,是NMDA受体的抗原识别区。目前关于NMDA受体抗原表位如何启动自身免疫与B淋巴细胞等炎症细胞接触反应,进而产生抗NMDA抗体尚不清楚。在中枢神经系统,NMDA受体抗原表位是通过激活浆细胞产生抗体,而在外周系统,抗NMDA抗体与NMDA受体的细胞外抗原表位相结合,通过受损的血脑屏障进而到达中枢神经系统[4]。70%~90%的抗NMDA受体脑炎患者伴有头痛、发热等前驱症状,提示感染可能参与抗NMDA受体脑炎的自身免疫过程[5]。抗NMDA抗体与受体NR1亚单位细胞外区域氨基末端的抗原表位接触后,导致受体加帽与交联,受体内化增加,使得突触表面受体密度降低,引起谷氨酸能神经传导障碍,产生相应的临床症状[6]。抗NMDA受体脑炎患者容易合并卵巢肿瘤的原因在于成熟或不成熟卵巢组织中表达NMDA受体相关抗原表位,打破了机体免疫耐受[1]。
2.2 临床表现
抗NMDA受体脑炎发病率具体不清,30岁以下多见,女性多于男性,男女比例1∶4[5],好发时间为4~9月,部分患者伴有畸胎瘤[7]。该病临床表现多样,多数患者在病程中可出现以下临床事件[5,8],前驱感染史:发病前可出现发热、头痛、咳嗽、腹泻等感染症状;精神行为异常:表现为胡言乱语、躁狂、幻听、幻视等症状;癫痫发作:患者可表现为全面强直阵挛发作、精神运动性发作;记忆力下降:以近事记忆下降为主;无应答期:表现为缄默不语、淡漠等;运动障碍:面舌及肢体不自主运动、舞蹈样动作等;自主神经功能紊乱:表现为心动过速、流涎、中枢性发热等;中枢性低通气:需气管插管维持呼吸。
本组患者平均年龄30岁,女3例,男3例,其中有1例患者为老年男性,伴有畸胎瘤者2例,小细胞肺癌1例。3例患者有前驱感染史,表现为发热、头痛不适;3例以精神行为异常首发;3例以癫痫发作为首发表现,表现为全面强直-阵挛发作;4例患者存在不自主运动症状:1例表现为反复伸舌,双上肢不自主运动,1例表现为左下肢抖动,2例口角不自主运动;5例患者存在自主神经功能紊乱:2例表现为唾液分泌过多(流涎),1例表现为多汗,其余2例小便失禁。尽管多数文献报道抗NMDA受体脑炎主要见于青年人,合并肿瘤时多见于畸胎瘤,但在我们的病例中可见1例老年患者(>60岁)发病,并伴有小细胞肺癌,而国外仅有少量文献报道[9-10]过类似病例。因此,对于临床主要以精神行为异常、癫痫发作、不自主运动、自主神经功能障碍为突出表现的年轻或老年患者,均需高度警惕抗NMDA受体脑炎可能,必要时行全身肿瘤筛查。
2.3 头颅MRI
在病情进展过程中,部分抗NMDA受体脑炎患者头颅MRI是正常的[11],只有大约50%的患者头颅MRI存在异常[12],表现为T2及Flair像高信号,可累及海马、颞叶、额叶、胼胝体等部位。對于头颅MRI正常的患者,必要时行PET-CT检查,病变区域可发现葡萄糖高代谢改变[13]。本组患者在临床症状较重时行头颅MRI,只有2例头颅MRI表现异常:1例双侧丘脑DWI高信号,1例左侧颞叶T1、T2、Flair高信号,其余4例正常。提示患者头颅MRI表现与症状严重程度并不完全一致,需结合患者临床表现及相关辅助检查,对病情进行整体评估;同时也说明颅内病变范围不仅可累及边缘系统,也可累及边缘系统以外。
2.4 脑脊液检查
抗NMDA受体脑炎患者脑脊液化验检查可表现为压力、白细胞数、蛋白轻度升高,也可正常,呈淋巴细胞反应性炎症,体现了免疫介导的炎症过程[1,11,14]。本组患者中,脑脊液正常1例,压力升高2例,压力及白细胞数均轻度升高2例,白细胞数及蛋白数均轻度升高1例。总体来看,此类患者脑脊液化验结果缺乏特异性,因此需注意与病毒性脑炎相鉴别。有研究指出血清和脑脊液中抗NMDA受体抗体滴度越高,提示合并畸胎瘤可能性越大,预后越差[15]。由于该抗体在鞘内合成,脑脊液抗体浓度高于血清浓度,部分患者血清抗体可自行转阴[16]。因此临床工作中,我们需同时检测脑脊液及血清抗NMDA受体抗体,增加诊断阳性率,避免漏诊,指导临床诊断。
2.5 脑电图
抗NMDA受体脑炎患者脑电图可出现弥漫性或多灶性慢波,偶可出现癫痫波[11];大多数患者在病程中可出现不自主运动症状,多与癫痫发作无相关性,两者难以区分时可行动态脑电图鉴别[17];大约30%的抗NMDA受体脑炎患者脑电图可见典型“δ刷”(1~3 Hz的δ活动上叠加20~30 Hz节律性的β活动),其特异性较强但敏感性差[18]。本组患者中,2例动态脑电图主要以弥漫性慢波背景为主,夹杂有少量尖慢波,其余脑电图未见异常。在临床中,常规行动态脑电图监测,有利于抗NMDA受体脑炎的早期诊断及临床症状的区分。
2.6 治疗及与预后
据文献报道,抗NMDA受体脑炎患者对免疫治疗效果较好,70%~80%患者经免疫治疗后可恢复[19-20]。一线药物治疗包括激素、免疫球蛋白、血浆置换,二线药物治疗包括环磷酰胺、利妥昔单抗[11-12]。一线药物治理效果不佳时可考虑使用二线药物治疗,一定程度可缩短病程,但仍有少部分患者脑炎会再次复发。此时,长疗程免疫抑制剂治疗可在一定程度上减少复发风险,改善预后[21]。对于伴有肿瘤的患者,手术切除是首选治疗方式[11],早期诊断、积极的手术干预及药物治疗,可以降低致残率及致死率[22]。另外,抗NMDA受体脑炎容易被误诊为病毒性脑炎和精神障碍疾病[23],这些患者在病情演化过程中如果出现癫痫发作、精神行为异常的表现时,需高度警惕抗NMDA受体脑炎的可能。
[参考文献]
[1] Dalmau J,Tüzün E,Wu H,et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma [J]. Ann Neurol,2007,61(1):25-36.
[2] Cull-Candy S,Brickley S,Farrant M. NMDA receptor subunits:diversity,development and disease [J]. Curr Opin Neurobiol,2001,11(3):327-335.
[3] Furukawa H,Singh SK,Mancusso R,et al. Subunit arrangement and function in NMDA receptors [J]. Nature,2005, 438(7065):185-192.
[4] Moscato EH,Jain A,Peng X,et al. Mechanisms underlying autoimmune synaptic encephalitis leading to disorders of memory,behavior and cognition:insights from molecular,cellular and synaptic studies [J]. Eur J Neurosci,2010, 32(2):298-309.
[5] Dalmau J,Lancaster E,Martinez-Hernandez E,et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis [J]. Lancet Neurol,2011,10(1):63-74.
[6] Hughes EG,Peng X,Gleichman AJ,et al. Cellular and Synaptic Mechanisms of Anti-NMDA Receptor Encephalitis [J]. J Neurosci,2010,30(17):5866-5875.
[7] Adang LA,Lynch DR,Panzer JA. Pediatric anti-NMDA receptor encephalitis is seasonal [J]. Ann Clin Transl Neurol,2014,1(11):921-925.
[8] Lim J,Lee S,Jung K,et al. Anti-N-Methyl-D-Aspartate Receptor Encephalitis in Korea:Clinical Features,Treatment,and Outcome [J]. J Clin Neurol,2014,10(2):157-161.
[9] Rainey K,Gholkar B,Cheesman M. Anti-NMDA receptor encephalitis:an easily missed diagnosis in older patients [J]. Age Ageing,2014,43(5):725-726.
[10] Jeraiby M,Depincé-Berger A,Bossy V,et al. A case of anti-NMDA receptor encephalitis in a woman with a NMDA-R+ small cell lung carcinoma(SCLC)[J]. Clin Immunol,2016,166/167:96-99.
[11] Leypoldt F,Wandinger KP. Paraneoplastic neurological syndromes [J]. Clin Exp Immunol,2014,175(3):336-348.
[12] Zaborowski MP,Spaczynski M,Nowak-Markwitz E,et al. Paraneoplastic neurological syndromes associated with ovarian tumors [J]. J Cancer Res Clin Oncol,2015,141(1):99-108.
[13] Baumgartner A,Rauer S,Mader I,et al. Cerebral FDG-PET and MRI findings in autoimmune limbic encephalitis:correlation with autoantibody types [J]. J Neurol,2013, 260(11):2744-2753.
[14] Wang R,Guan H,Ren H,et al. CSF findings in patients with anti-N-methyl-d-aspartate receptor-encephalitis [J]. Seizure,2015,29:137-142.
[15] Gresa-Arribas N,Titulaer MJ,Torrents A,et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis:a retrospective study [J]. Lancet Neurol,2014,13(2):167-177.
[16] Peery HE,Day GS,Dunn S,et al. Anti-NMDA receptor encephalitis. The disorder,the diagnosis and the immunobiology [J]. Autoimmun Rev,2012,11(12):863-872.
[17] Cohen AL,Wong-Kisiel LC. Case of a Two-Year-Old Boy With Recurrent Seizures,Abnormal Movements,and Central Hypoventilation [J]. Semin Pediatr Neurol,2014, 21(2):114-118.
[18] Veciana M,Becerra JL,Fossas P,et al. EEG extreme delta brush:An ictal pattern in patients with anti-NMDA receptor encephalitis [J]. Epilepsy Behav,2015,49:280-285.
[19] Zekeridou A,Karantoni E,Viaccoz A,et al. Treatment and outcome of children and adolescents with N-methyl-d-aspartate receptor encephalitis [J]. J Neurol,2015,262(8):1859-1866.
[20] Dogan OM,Golombeck KS,Bien C,et al. Immunoadsorption therapy in autoimmune encephalitides [J]. Neurol Neuroimmunol Neuroinflamm,2016,3(2):1-10.
[21] Guan H,Kong W,Peng B,et al. Clinical analysis of relapsing anti-N-methyl-D-aspartate receptor encephalitis [J]. Zhonghua Yi Xue Za Zhi,2015,95(13):996-1001.
[22] Titulaer MJ,Mccracken L,Gabilondo I,et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis:an observational cohort study [J]. Lancet Neurol,2013,12(2):157-165.
[23] Lazar-Molnar E,Tebo AE. Autoimmune NMDA receptor encephalitis [J]. Clin Chim Acta,2015,438:90-97.
(收稿日期:2016-10-11 本文編辑:张瑜杰)